Table of Contents
Page created on October 6, 2018. Last updated on November 4, 2019 at 18:48
Summary
Renovascular hypertension is a type of secondary hypertension that occurs due to stenosis of the renal artery, leading to RAAS activation.
Renoparenchymal hypertension is another type of secondary hypertension that occurs due to loss of renal parenchyme and the renal depressor system.
Introduction
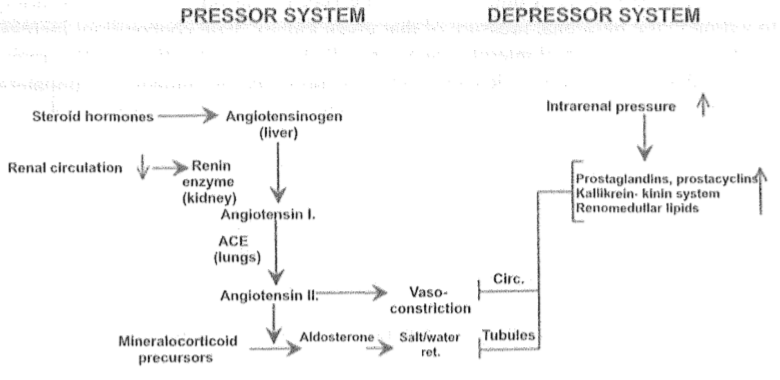
Because the renin-angiotensin-aldosterone system depends on the kidneys to produce renin are the kidneys very central in hypertension as well. However, the kidneys also have a system they can use to decrease blood pressure, the renal depressor system (like in de-blood pressure).
Kidney-related hypertension is called renal hypertension, and it is further divided into two types: renovascular and renoparenchymal. Renal hypertension is a secondary type of hypertension.
Renovascular hypertension
Recall that when renal blood flow (RBF) is reduced, the juxtaglomerular cells in the kidney start producing renin. The kidneys do this because a reduced RBF usually means that the volume of the blood is too low, which also means that the blood pressure is too low. As renin is produced the RAAS is activated and the end result is vasoconstriction and increased salt and water retention, in order to bring back the blood volume to normal.
However, if a renal artery is stenosed (often due to atherosclerosis) will the RBF be reduced without the blood volume or blood pressure actually being low. The juxtaglomerular cells will nevertheless activate the RAAS, which will increase the blood pressure above the normal.
Renovascular hypertension was discovered in an experiment carried out by a guy named Harry Goldblatt. He operated on an animal with two functioning kidneys and put a clip on one of the renal arteries. The animal ended up developing hypertension, and this hypertension could be normalized by administrating drugs which inhibits the ACE enzyme (ACE inhibitors). This indicates that the hypertension comes from the RAAS.
The other, un-stenosed kidney compensates for the hypertension by increasing its sodium and water excretion, which returns the blood volume and cardiac output back to normal. However, it cannot change the high levels of angiotensin in the blood due to contralateral RAAS activation, which causes peripheral vasoconstriction and therefore keeps the TPR and blood pressure high anyway.
If we remove the clip of the renal artery after a short time the blood pressure will normalize as the RAAS will stop being overactive. However, if the clip is removed after a long time the hypertension will persist even after removing the clip! How is this possible?
The hint to understanding this is shown by the fact that removing the contralateral kidney (the one whose artery was never clipped) will cause the blood pressure to return to normal. This indicates that the contralateral kidney somehow was the problem. To understand this, we must look at the kidney parenchyme’s role in hypertension.
Renoparenchymal hypertension
As introduced earlier, the kidney has a system for decreasing the blood pressure as well. This depressor system comes from the function of the kidney parenchyme, which secretes vasodilatory substances like prostacyclins and kinins.
In the experiment the contralateral kidney was exposed to the effects of hypertension for too long, so its parenchyme started to become injured. This parenchymal injury causes the kidney to lose its depressor function, meaning that the kidney no longer can keep the blood pressure down. The result is hypertension.
Any systemic hypertension will cause kidney parenchyme damage and resulting renoparenchymal hypertension. If a patient for example has high blood pressure due to a sedentary lifestyle for a long time, and then decides to fix his shit and start working out, the blood pressure might not be reduced anyway, because the chronic hypertension has caused so much damage to the kidneys.
Other things than hypertension can cause renal parenchyme damage and therefore hypertension, like:
- Acute glomerulonephritis
- Chronic pyelonephritis
- Polycystic kidney
- Diabetic nephropathy
- Hydronephrosis