Table of Contents
Page created on April 29, 2018. Last updated on December 18, 2024 at 16:55
Hypersensitivity responses are pathological overreaction responses by the immune system that lead to tissue damage. There are four different types of hypersensitivity reactions. The first three are mediated by immunoglobulins while the last is mediated by cells and cytokines. There is usually overlap between type I, type II and type III, so if someone has a type I reaction, they probably have type II and type III to some degree as well.
Hypersensitivity type I – immediate hypersensitivity
The type I reaction is the allergic reaction. It applies to allergies like pollen allergy. It is mediated by IgE antibodies and mast cells.
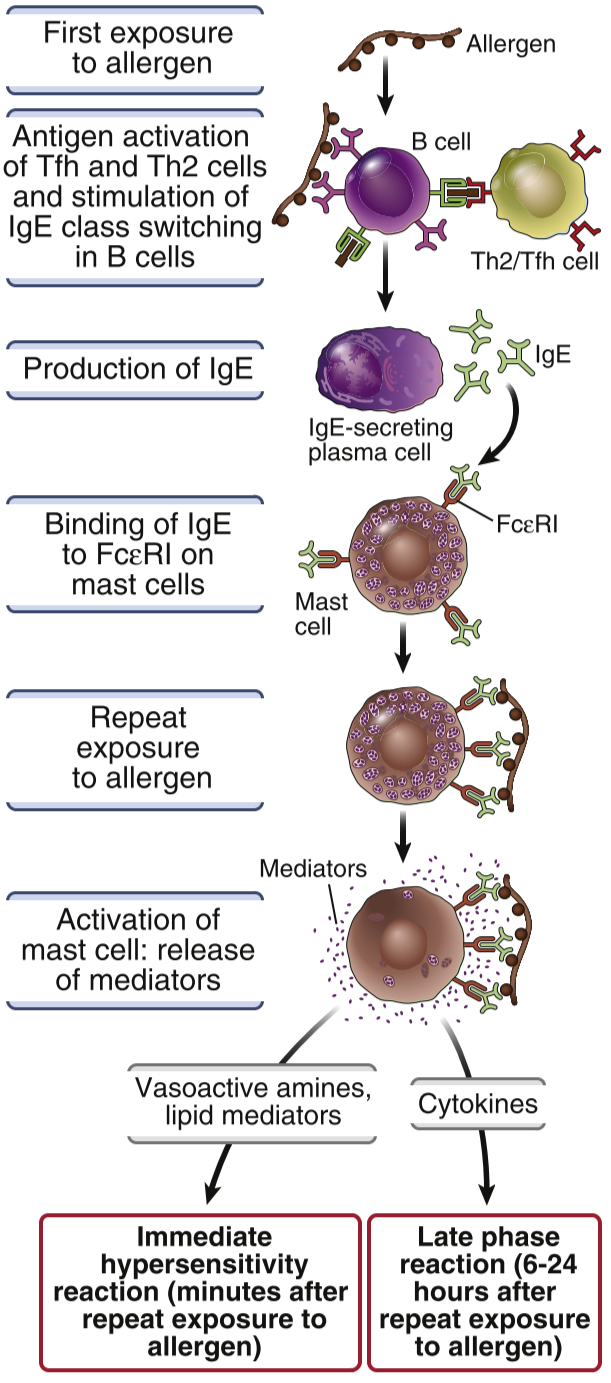
Th2 cells meet with the antigen, causing them to produce cytokines like IL-4, IL-5 and IL-13. IL-4 induces isotype switching to IgE. The body will then produce a lot of IgE against the allergen, which will bind to FcεR I on mast cells. The mast cells are now sensitized, as they are now very sensitive to subsequent encounters with the same allergen.
When the body is re-exposed to the allergen the IgE antibodies that are now bound to the mast cells will bind to the allergen. This causes the mast cells to release many different molecules. Vasoactive amines like histamine causes vasodilation and smooth muscle contraction. Proteases cause damage to the tissues by degrading proteins. Prostaglandins and leukotrienes are produced from arachidonic acid and also cause vasodilation and smooth muscle contraction. Lastly, cytokines like TNF recruits other white blood cells to the tissue and causes inflammation.
Hypersensitivity type I can be treated in multiple ways. The best but also least available treatment is the allergen-free environment. Antihistamines also work well in the short term, but studies have shown that histamine is important in restricting tumor development, so chronic use of antihistamines is therefore not ideal. Non-specific immunosuppressants like cortisol can also be used to treat allergies, but long-term exposure to cortisol can cause other problems.
Type II hypersensitivity – cytotoxic hypersensitivity
The type II hypersensitivity reaction can occur in allergy against medications like penicillin and is the reaction that happens in the case of some diseases which we’ll come back to later. It’s mediated by IgG and IgM, but mostly IgG.
Let’s take penicillin as an example. Penicillin can function as haptens that bind to proteins on red blood cells. This causes these proteins to be recognized as foreign antigens by the body. Macrophages will phagocytose the RBC – penicillin complex, present antigens to Th cells which causes Th -> Th2 differentiation. Th2 cells then produce IL-4, which induce isotype switching to IgG1 (and IgE). The body will then produce IgG1 antibodies that bind to penicillin.
IgG1 will then opsonize the RBCs that are covered by penicillin. This opsonization causes activation of the classical pathway of the complement system, increased phagocytosis and activation of ADCC. These three mechanisms will then kill RBCs, which is obviously not good.
AB0 blood group incompatibility, erythroblastosis fetalis, Graves’ disease and myasthenia gravis are also examples of type II hypersensitivities. Graves’ disease happens when the body produces antibodies against the TSH receptor on cells of the thyroid gland. These antibodies will then activate the receptor, which will cause hyperthyroidism. In myasthenia gravis the body produces antibodies against the nicotinic acetylcholine receptors, which inhibits the binding of acetylcholine to the receptors, which causes muscle weakness.
Type III hypersensitivity – immunocomplex disease

Type III hypersensitivity occurs when there is a slight excess of antigens in the body, and the body struggles to get rid of all of them. Antibodies and complement factors will bind to these antigens to form small immune complexes. Large immune complexes can easily be phagocytosed by macrophages but macrophages struggle to take care of small immune complexes. These small complexes then deposit in blood vessels (mainly) and in tissues. These deposited immune complexes activate the complement system which causes recruitment of immune cells that produce inflammation.
A type of reaction called the Arthus reaction is a type of type III hypersensitivity response. It’s characterized by a local inflammation of blood vessels in the skin. Other diseases that are of this type of hypersensitivity are lupus (SLE) and farmer’s lung disease.
Type IV hypersensitivity – Delayed Type Hypersensitivity
The type IV hypersensitivity was already talked about in topic 16, but we’ll talk a little bit about it here as well.
DTH begins 1-2 weeks after the first contact with the antigen. APCs produce IL-12 in the response to the antigen which causes Th -> Th1 differentiation. Th1 cells will then proliferate and become sensitized. Re-exposure or persistence of the antigen will activate the Th1 cells which will cause activation of macrophages and other inflammatory immune cells. In the case of re-exposure, this reaction takes 48-72 hours, which gives the DTH its name.
If there is a chronic (long-lasting) DTH reaction, granulomas will form. DTH reactions are found in the case of multiple sclerosis, rheumatoid arthritis, type 1 diabetes, tuberculosis and contact dermatitis.
Summary
| Type I | Type II | Type III | Type IV – DTH | |
| Mediated by | Antibodies | Antibodies | Antibodies | Cells and cytokines |
| Antibody or cell involved | IgE | IgG and IgM | IgG and IgM | Th1 and macrophages |
| Antigen | Exogenous | Haptens for cell surfaces | Soluble (as immune complex) | Specific pathogens and allergens |
| Response time | 15-30 minutes | Minutes-hours | 3-8 hours | 48-72 hours |
| Examples | Pollen allergy | Erythroblastosis fetalis, Graves’ disease | Lupus, farmer’s lung disease | Tuberculosis, poison ivy |
Hello !
Thanks for your work !
Where does the figure comme from please ? Do you have any sources ?
Many thanks !
It is taken from the book «Basic Immunology
Functions and Disorders of the Immune System» by Abbas, Abul K. Lichtman, Andrew H. Pillai, Shiv. You will have to contact the publisher (Elsevier – Health Sciences Division) for these rights. In the fifth edition it’s on page number 234 with figure number 11-2.
There appears to be a slight error for the Hypersensitivity Type 1. IL4 is not produced by the Macrophage to induce Th-Th2 transformation. As you write correctly for Hypersensitivity Type 2, IL4 is produced by the Th2 cells after they have been activated by Macrophages (via MHC2).
You’re right. It’s fixed now. Thanks!