Table of Contents
Page created on January 20, 2020. Last updated on January 12, 2024 at 19:36
A. Basic topics
1. Psoriasis
- A type of systemic papulosquamous dijusease
- Epidemiology
- 2% of whites, less common in other skin colours
- 20 – 40 years
- Family history
- 50 – 100 years
- No family history
- Etiology
- Polygenic inheritance (HLA)
- Triggers
- Streptococci URTI
- Irritation of skin
- Staph
- HIV
- Mechanical irritation
- Alcohol
- Stress
- Drugs
- Beta blockers
- Lithium
- Interferon
- Chloroquine
- Pathophysiology
- Acanthosis
- Hyperplasia of stratum spinosum
- Elongated rete ridged
- Parakeratosis – nuclei retention
- Hyperkeratosis
- Munro microabscesses
- T-cell secreted cytokines
- Overexpression of beta-defensin -> no secondary superinfection
- Acanthosis
- Clinical features
- Symptom-free intervals with relapsing
- Lesions
- Well-demarcated
- Salmon-coloured erythematous, silvery scaling plaques
- Mainly on scalp, back and extensor surfaces
- Elbow
- Knees
- Scalp
- Gluteal cleft
- Pruritus
- Nail involvement
- Nail pitting (small depressions in nail)
- Oil drop sign – well-circumscribed yellow-red discoloration
- Brittle nails
- Onycholysis – separation of the nail plate
- Nail separates from the skin below -> becomes grey
- Psoriatic arthritis
- 5 – 30% of patients
- Very debilitating
- Distal and proximal interphalangeal joints
- Spine
- Diagnosis (CASPAR)
- > 3 of these
- Psoriasis
- Psoriatic nail problems
- Negative rheumatoid factor
- Dactylitis – sausage finger
- Radiological signs
- Treatment
- NSAIDs
- DMARDs
- Other forms
- Guttate psoriasis
- Drop-sized lesion
- In children after strep
- Inverse psoriasis
- Skin folds and flexor surfaces
- Guttate psoriasis
- Diagnosis (mostly clinical)
- Auspitz sign – pinpoint bleedings when scales are scraped off
- Koebner phenomenon – skin damage causes psoriasis to appear there
- Skin biopsy – rarely needed
- Parakeratosis
- Munro microabscesses
- Acanthosis
- Differential diagnosis
- Atopic dermatitis/atopic eczema
- Poorly demarcated
- Severe pruritus
- Exudative, not dry
- Flexor surfaces
- Seborrheic dermatitis
- Greasy-looking yellow scales
- On face and trunk
- Atopic dermatitis/atopic eczema
- Treatment
- Moisturizer
- Avoid nicotine, alcohol
- Topical
- Steroids
- Triamcinolone
- Fluocinonide
- Clobetasol
- Vitamin D derivatives
- Calcipotriene
- Tar preparations
- Retinoids
- Steroids
- Systemic
- MTX
- Retinoids
- Cyclosporine
- Biological therapy
- Adalimumab, infliximab, etanercept – TNF alpha
- Secukinumab – IL-17
- Briakinumab – IL-23
- Phototherapy
- UVB therapy
- Narrow-band UVB
- PUVA (psoralen + UVA)
- Psoralen increases photosensitivity of skin
- UVA radiation
- UVB therapy
- Complications
- Increased CV risk
- Metabolic syndrome
- Kidney disease
2. Pyodermas
- “Free” pyodermas
- Impetigo
- Superficial skin infection
- Highly infectious
- Children
- Most common bacterial skin infection in children
- Etiology
- Staph aureus – 80%
- Strep pyogenes
- Risk factors
- Diabetes
- Immunosuppression
- Secondary – superinfection of atopic dermatitis, etc
- Clinical features
- Honey-crusted lesions
- The result of ruptured pustules
- Central face
- Itching
- Can be bullous
- Honey-crusted lesions
- Types
- Ecthyma
- A form of impetigo that extends into the dermis and ulcerates
- Risk factors
- Diabetes
- Immunosuppression
- Round superficial ulcers
- Ecthyma
- Treatment
- Antibacterial wash
- Mild – topical antibiotics
- Mupirocin
- Severe – oral antibiotics
- Amoxicillin
- Complications
- Post-streptococcal GN
- Cellulitis
- Deeper than impetigo
- Infection of deep dermis and subcutaneous tissue
- Etiology
- Staph aureus -> purulent cellulitis
- Strep pyogenes -> nonpurulent cellulitis
- Primary – entry through minor skin injury
- Secondary – to systemic infection
- Clinical features
- Erythematous lesion with poorly defined margins
- Purulent cellulitis -> purulent exudate
- Treatment
- Penicillin
- Erysipelas
- Special type of cellulitis caused by strep pyogenes
- Epidemiology
- Children
- Poor circulation
- Stasis
- Diabetics
- Chronic oedema
- Spreads by superficial lymph vessels
- Clinical features
- On lower limbs – 80%
- On face – rarely
- Large erythema, irregular borders
- Tender
- Rapidly advancing borders
- Oedema
- Warm
- Fever
- Site of entry needs to be located
- Ulcers
- Interdigital lesion
- Fungal infections
- Treatment
- Antibiotics
- Primary: Amoxicillin and clavulanic acid
- Secondary: Ciprofloxacin and clindamycin
- Tertiary: Ceftriaxone and metronidazole
- Bed rest
- Icing
- Compression
- Elevation
- Antibiotics
- Complications
- Necrotizing fasciitis
- Sepsis
- Residual erysipelas
- Necrotizing fasciitis
- Necrotizing infection of deep subcutaneous tissue
- Etiology
- Strep pyogenes
- Staph aureus
- Pseudomonas
- Clinical features
- Painful, haemorrhagic, necrotizing lesion
- High mortality
- Treatment
- Surgical removal of affected fascia (necrectomy)
- Antibiotics
- Intensive care
- Follicular pyodermas
- Folliculitis
- Any age group
- Terminal or vellus hairs
- Usually bacterial
- Mainly staph aureus
- Clinical features
- Tender papule/pustule of hair follicle
- Treatment
- Dicloxacillin
- Incision and drainage for large lesions
- Furuncle
- Well-demarcated, firm, painful, purulent nodule
- Large red base
- Subcutaneous abscess
- Carbuncle
- Coalescence of furuncles
- Skin abscess
- Large nodule
- Folliculitis
3. Basal cell carcinoma and squamous cell carcinoma
- Basal cell carcinoma
- Most common skin cancer
- Related to mutations in the hedgehog pathway
- Risk factors
- Chronic sun exposure
- Old age
- Skin types I and II
- Clinical features
- Pearly papule or nodule
- Rolled border
- Central crater of ulceration
- On sun-exposed skin
- Usually upper lip/nose area
- Slow growing
- Types
- Nodular BCC
- Most common type
- Superficial BCC
- On trunk
- Flat plaque lesion
- Nevoid basal cell carcinoma syndrome
- Nodular BCC
- Prognosis
- Virtually never metastasizes
- Locally aggressive
- Diagnosis
- Full-thickness biopsy -> histology
- Treatment
- Surgical excision
- Irradiation
- Mohs micrographic surgery
- Hedgehog pathway inhibitors
- For low-risk, spf BCC
- Photodynamic therapy
- Cryotherapy
- 5-FU
- Imiquimod cream
- Follow-up
- Physical examination at 3, 6, 12 months
- Sun protection
- Squamous cell carcinoma
- Second most common skin cancer
- Risk factors
- Chronic sun exposure
- Precancerous lesions
- Actinic keratosis
- Bowen disease (SCC in situ)
- Leukoplakia
- Radiation
- Chronic scars, ulcers
- Arsenic, tar
- Clinical features
- Painless, non-healing, bleeding ulcer or nodule
- Rapid growing
- On sun-exposed areas
- Face and neck
- Lower lip
- Prognosis
- 5% risk of metastasis
- Diagnosis
- Punch biopsy
- Treatment
- Surgical excision with 5 mm safety border
- Radiation therapy
- Mohs micrographic surgery
- For low-risk, small
- Cryotherapy
- Curettage
- For metastasis
- Chemotherapy
- Platina
- 5-FU
- EGFR inhibitors – cetuximab
- PD-1 inhibitor – cemeplimab
- Chemotherapy
- Follow-up
- Physical examination
- Regional ultrasound
- Chest x-ray
- Abdominal US
- Sun protection
4. Atopic dermatitis
- Affects 10% of children, but only 1 – 3% of adults
- Associated with other atopic diseases
- Asthma
- Allergic rhinitis
- Etiology
- Polygenic inheritance
- Environmental riggers
- Dust
- Heat
- Infection
- Skin irritation
- Pathophysiology
- Epidermal skin barrier defect
- -> water loss
- -> allergens can penetrate barrier
- Abnormal immune response
- Epidermal skin barrier defect
- Clinical features
- Morphology
- Acute
- Erythematous maculopapular rash
- Dry plaques
- Oedema
- Chronic
- Lichenification
- Scaling
- Fissures
- Acute
- Mostly on flexor surfaces
- Except in infants
- Pruritus
- Dry skin
- Cheilitis
- Morphology
- Diagnosis
- Clinical
- Serum IgE elevated
- Serum LDH elevated
- Complications
- Staph infection
- Eczema herpeticum
- Tinea
- Treatment
- Emollients
- Topical corticosteroids
- Mometasone
- Clobetasol
- Topical calcineurin inhibitors
- Tacrolimus
- Oral antihistamines
- Oral immunosuppressive therapy
- Corticosteroids
- Cyclosporine
- Biological treatment
- Anti-IL-4 – dupilumab
- Anti-IL-5 – mepolizumab
- Anti-IL-31 – prevents itching
- Anti-TSLP
5. Leg ulcer
- Leg ulcer
- Etiology
- Chronic venous disease
- Peripheral artery disease
- Neuropathic ulcer
- Diabetes
- Decubitus
- Trauma
- Infections
- Dermatoses (SLE, pyoderma gangrenosum)
- Neoplastic
- Morphology
- Venous ulcer
- Above the ankle
- Mild pain
- Pain improves when raising leg
- Shallow ulcer
- Arterial ulcer
- Punched-out well-defined ulcer
- Pressure points of the legs (malleolus, toes)
- Severe pain
- Pain worsens when raising leg
- Venous ulcer
- Treatment
- Underlying disease
- Surgical
- Irrigation
- Debridement
- Removal of dead, damaged or infected tissue
- Wet dressing
- Skin grafting
- Local therapy
- Wound healing
- Compression
- Treating adjacent skin
- Etiology
- Peripheral artery disease
- Staging
- Fontaine stage I – symptom free
- Fontaine stage II – Claudication > 50m
- Fontaine stage III – Claudication < 50m
- Fontaine stage IV – Necrosis, gangrene
- Diagnosis
- Inspection
- Doppler index
- Angiography
- Therapy
- Conservative
- Interventional radiology
- Vascular surgery
- Staging
- Lymphoedema
- Treatment
- Conservative (Compression)
- Vascular surgery
- Treatment
- Chronic venous diseases
- Older females
- Risk factors
- Female
- Previous thrombus
- Pregnancy
- Standing for long periods
- Oral contraceptives
- Varicose veins
- Dilated torturous superficial veins with knots
- Chronic venous insufficiency
- Increased venous pressure -> oedema -> tissue ischaemia
- Clinical features
- Local oedema
- Red-brown pigmentation (haemosiderosis)
- Loss of hair
- Smooth skin
- Stasis dermatitis
- CEAP classification
- Clinical
- Etiology
- Anatomy
- Pathophysiology
- Diagnosis
- Doppler ultrasound
- Treatment
- Conservative
- Compression
- Elevation of legs
- Lymphatic drainage massage
- Vein ablation
- Thermal ablation
- Chemical ablation (sclerotherapy)
- Conservative
6. Skin diseases caused by human papilloma virus (HPV)
- Warts (verruca)
- Histology
- Hyperkeratosis (hyperplasia of str. corneum)
- Acanthosis (hyperplasia of epidermis)
- Papillomatosis
- Hard papules/plaques
- Risk factors
- Immunosuppression
- Due to HPV
- Verruca vulgaris (common wart)
- HPV 1, 2, 4, 7
- Most common in kids
- On elbows, knees, fingers, palms
- Skin-coloured or whitish, rough, scaly papules
- Cauliflower-appearance
- Verruca plana (flat warts)
- HPV 3, 11
- On face, back of hand, legs
- Skin-coloured, smooth papules, flat surface
- Verruca plantaris (plantar warts)
- HPV 1, 2, 4
- Soles of the feet
- Skin-coloured
- Rough surface
- Treatment
- Usually resolves by themselves (can take years)
- Topical treatment
- Keratolytics
- Salicylic acid
- Retinoic acid
- Cytostatic
- Podophyllin
- 5-FU cream
- Immune therapy
- Imiquimod
- Keratolytics
- Surgery
- Cryotherapy
- Surgical excision
- Leaves permanent, painful scars
- Prevention
- Vaccination
- Cervarix – 16, 18
- Silgard – 6, 11, 16, 18
- Gardasil 9 – 6, 11, 16, 18, 31, 33, 45, 52, 58
- Vaccination
- Histology
- Condyloma acuminata – genital warts
- HPV 6, 11
- Exophytic, cauliflower-like lesions
- In anogenital area or mucous membranes
- STD
- Giant condyloma acuminatum
- HPV 6, 11
- Exophytic wart-like locally invasive squamous cell carcinoma without tendency to metastasize
- Precancerous lesions
- Vulvar intraepithelial neoplasia
- Vaginal intraepithelial neoplasia
- Flat condylomata
- Flat, white-brown plaques in anogenital region
- High risk of malignancy
- Anogenital squamous cell carcinoma
- Vaginal cancer
- Vulvar cancer
- Anal cancer
- Penile cancer
7. Herpes simplex virus (HSV) infections of the skin
- Herpes viruses
- α herpes viruses
- Lie latent in sensory ganglia neurons
- Replicate quickly
- Herpes simplex 1
- Herpes simplex 2
- Varicella zoster virus
- β herpes viruses
- Lie latent in leukocytes
- Human herpes virus 6 – roseola infantum/sixth disease
- Human herpes virus 7
- CMV
- γ herpes viruses
- Lie latent in lymphocytes
- Human herpes virus 8
- EBV
- Are oncogenic
- α herpes viruses
- HSV infections
- Labial herpes
- On lips
- HSV-1 in 90%
- HSV-2 in 10%
- Clinical features
- Prodromal symptoms – 24 hours before outbreak
- Pain
- tingling
- Burning
- Recurring, erythematous vesicles that turn into painful ulcerations
- Prodromal symptoms – 24 hours before outbreak
- Complications
- Herpetic gingivostomatitis
- In children and immunocompromised
- Often the primary infection
- Erythema, painful ulceration on perioral skin and oral mucosa
- Herpetic gingivostomatitis
- Genital herpes
- On genital organs
- HSV-2 in most cases
- HSV-1 rarely
- Incubation period – 2 – 7 days
- Clinical features
- Many are asymptomatic
- Painful lymphadenopathy
- Vesicles that ulcerate
- Eczema herpeticum
- HSV-1, HSV-2
- On pre-existing skin conditions
- Atopic dermatitis
- Extensive disseminated and painful eruptions on head and upper body
- Erythematous skin with multiple, round vesicles
- It’s an emergency
- Treatment -> IV acyclovir
- Herpetic whitlow
- In children and healthcare workers who come into contact with saliva
- Direct contact with infected saliva through a break in the skin
- Pain, burning, oedema in finger
- Lymphadenopathy
- Treatment
- Decreases duration and severity
- Most effective if initiated within 72 hours
- Mild disease
- Oral acyclovir (5 x 800mg for 10 days)
- Severe disease
- IV acyclovir
- Acyclovir-resistance -> foscarnet
- Labial herpes
8. Skin diseases caused by varicella zoster virus
- Varicella (chickenpox)
-
- Primary infection during childhood
- Lasts 6 days in immunocompetent persons
- Transmission
- Highly contagious
- Airborne transmission
- Incubation period 2 weeks
- Clinical features
- Lesions covering the entire body
- Severe pruritus
- Macules -> papules -> vesicles with erythematous base -> crusts
- All of these stages are present simultaneously, which is a hallmark for the disease
- Fever
- Virus remains latent in sensory ganglia
- Diagnosis
- Clinical -> characteristic rash
- Tzanck smear, PCR
- Treatment
- For pruritus
- Calamine lotion
- Pramoxine gel
- Oral antihistamines
- Therapy
- Only for severe cases or high-risk groups (adults, immunosuppressed)
- Acyclovir
- Post-exposure prophylaxis
- Active immunization (vaccine)
- Passive immunization (immunoglobulins)
- For pruritus
- Prevention
- Vaccination
- Complication
- Bacterial superinfection
- Impetigo
- Phlegmon
- Scarring
- Congenital varicella syndrome (if chickenpox during pregnancy)
- Bacterial superinfection
- Shingles (herpes zoster)
- Reactivation
- Older patients
- Triggers
- Immunosuppression
- Advanced age
- Malignancy
- Malnutrition
- Clinical features
- Erupts in dermatome pattern
- Severe pain
- Erythematous maculopapular rash -> vesicles -> rupture
- Complications
- Herpes zoster oticus
- Herpes in facial and vestibulocochlear nerve
- Blindness
- Herpes zoster ophthalmicus
- Herpes in ophthalmic part of trigeminal nerve
- Facial paresis
- SN hearing loss
- Post-herpetic neuralgia
- Herpes zoster encephalitis
- Herpes zoster oticus
- Diagnosis
- Clinical -> characteristic rash
- Treatment
- Wet dressing with aluminium acetate
- 5 x 800mg acyclovir for 10 days
- NSAIDs
-
9. Autoimmune bullous skin diseases
- Bullous pemphigoid
- In elderly
- Benign disease, responds well to treatment
- Most common autoimmune bullous disease
- Pathomechanism
- Autoantibodies against hemidesmosomes
- Clinical features
- Prodromal stage
- Weeks before onset of blistering
- Urticarial lesions
- Large, tense, subepidermal bulla
- Don’t rupture easily
- Intensely pruritic
- Lower limbs, axilla
- Rarely oral involvement
- Prodromal stage
- Diagnosis
- Negative Nikolsky
- Histology and immunofluorescence
- Treatment
- Prednisone (0,5 – 1 mg/bwkg)
- Azathioprine, immunosuppressants
- Pemphigus vulgaris
- In middle-aged, elderly
- Deadly without treatment
- Pathomechanism
- Autoantibodies against desmosomes
- Acantholysis – loss of cell-cell adhesion
- Clinical features
- Painful, flaccid, intraepidermal (superficial) blisters
- -> lesions rupture
- -> erosions and crusts
- -> re-epithelialization with hyperpigmentation but no scarring
- No pruritus
- Lesions often begin in oral mucosa then to body parts exposed to pressure
- Diagnosis
- Positive Nikolsky – Skin comes off with scraping
- Histology and immunofluorescence
- Treatment
- High-dose prednisone (1-2 mg/bwkg)
- Azathioprine, other immunosuppressants
- Dermatitis herpetiformis
- In young adults
- Risk factors
- Coeliac disease
- Iodide sensitivity
- HLA-DR3
- HLA-DQ2
- Pathomechanism
- Tissue transglutaminase and epidermal transglutaminase antibodies
- Clinical features
- Chronic, recurrent
- Tense, grouped, subepidermal vesicles
- Herpetiform appearance, hence the name
- Intensely pruritic
- Bilateral, symmetrical distribution
- Elbows, knees
- No mucosal involvement
- Diagnosis
- Coeliac antibodies
- Histology and immunofluorescence
- Treatment
- Dapsone
- Gluten-free diet
- Epidermolysis bullosa
- Group of disorders where subepidermal blisters form following trauma
- Not autoimmune
- Epidermolysis bullosa simplex
- Junctional epidermolysis bullosa
- Dystrophic epidermolysis bullosa
- Epidermolysis bullosa acquisita
10. Lupus erythematosus and its variants
- Systemic lupus erythematosus
- Clinical features
- Skin
- Butterfly rash
- Nasolabial fold spared
- Photosensitivity
- Discoid rash -> atrophic scars
- Oral ulcers
- Butterfly rash
- Systemic
- Arthritis
- Fever
- Etc.
- Skin
- Treatment
- Steroids
- Cyclophosphamide
- Azathioprine
- Clinical features
- Cutaneous lupus erythematosus
- Chronic discoid lupus erythematosus (CDLE)
- Epidemiology
- Most common cutaneous type
- African American women
- Clinical features
- Erythematous scaling plaques
- -> leaves atrophic scars
- Ocular and mucosal lesions
- Affects face, scalp, neck (sun-exposed areas)
- No systemic symptoms
- Epidemiology
- Subacute cutaneous lupus erythematosus (SCLE)
- Clinical features
- Persisting diffuse erythema on face or sun-exposed areas
- Annular or psoriasiform erythematous plaques
- Morbilliform rash on trunk
- Affects neck, shoulders, forearms
- Diagnosis
- Anti-Ro antibody
- Clinical features
- Drug-induced lupus erythematosus (DILE)
- Resolves after discontinuation of the drug
- In elderly
- May occur years after starting the drug
- Etiology
- Sulpha drugs
- Thiazides
- Sulfamethoxazole
- Sulfasalazine
- Sulfonylurea
- Methyldopa
- Isoniazid
- Especially slow acetylators
- Phenytoin
- Sulpha drugs
- Clinical features
- Rash
- Myalgia
- Fever
- Polyarthritis
- Serositis
- Diagnosis
- Anti-histone antibodies
- Treatment of cutaneous lupus erythematous
- Hydroxychloroquine
- Steroids
- Immunosuppressants
- Sunscreen
- Chronic discoid lupus erythematosus (CDLE)
11. Scleroderma and its variants
- Scleroderma
- Abnormal growth of connective tissue
- In all types the skin is thickened and hardened
- Classification of scleroderma
- Systemic sclerosis/systemic scleroderma
- Limited systemic sclerosis/CREST syndrome
- Diffuse systemic sclerosis
- Systemic sclerosis sine scleroderma
- Localized scleroderma
- Morphea
- Linear scleroderma
- Systemic sclerosis/systemic scleroderma
- Systemic sclerosis
- Sclerosis of internal organs in addition to the skin
- Skin symptoms
- Thickening and hardening of skin
- Depigmentation (except perifollicular area)
- Salt-and-pepper appearance
- Sclerodactyly
- Face
- Loss of expression
- Shortened frenulum
- Microstomia
- Limited systemic sclerosis/CREST syndrome
- More common
- Skin manifestations are limited to hands, fingers and face
- Organ involvement is rare and limited
- Clinical features
- Calcinosis cutis – calcium deposits on pressure points of extremities
- Raynaud’s phenomenon
- Esophageal hypomobility
- Sclerodactyly
- Red-blue discoloration of fingers
- Fibrosis of fingers
- Atrophy and necrotic spots
- Telangiectasia
- Diffuse systemic sclerosis
- Less common
- More aggressive
- Early organ involvement
- Clinical features
- Oesophageal dysmotility
- Small bowel dysmotility
- Pulmonary hypertension
- Interstitial lung disease
- Cardiac fibrosis
- Renal disease
- Localized scleroderma
- No organ involvement, only skin
- Only localized parts of the skin are affected
- Morphea
- Isolated patches of hardened skin
- No organ involvement
- Treatment
- PUVA
- Intralesional steroid injection
- Linear scleroderma
- Starts as a line of hardened skin
- Develops in childhood
- Treatment
- PUVA
12. Malignant melanoma
- Epidemiology
- Only 2% of skin cancer
- Responsible for most skin cancer-related deaths
- Higher incidence in sun-rich countries like Australia compared to Europe
- Average age at onset ~50
- Risk factors
- Excessive UV exposure
- Fitzpatrick skin type I and II
- Easily burns
- Almost never suntans
- Often have freckles
- Precancerous lesions
- Dysplastic nevi
- Dysplastic nevus syndrome – 100% risk of developing melanoma
- Lentigo maligna
- Congenital nevi
- Indoor tanning
- Sunburns in childhood (>3)
- Positive family history
- Immunosuppression
- Familial genetic mutations
- BRAF (most common)
- NRAS
- p16 family
- Pathogenesis
- 2 growth phases:
- Radial/horizontal growth phase
- Tumor grows horizontally along epidermis
- No capacity to metastasize
- Vertical growth phase
- Tumor grows vertically into the dermis
- Can metastasize
- Subtypes
- Superficial spreading melanoma
- 60% of all cases
- Slow radial growth phase, mostly superficial spreading
- Nodular melanoma
- 20% of all cases
- Reddish-brownish-blackish nodule
- Can be ulcerated
- Has no radial growth phase, only vertical
- Poorer prognosis
- Lentigo maligna melanoma
- 10% of cases
- Originates from lentigo maligna in elderly
- Slow radial growth phase
- Lesion is often a large and irregularly shaped patch
- Acral lentiginous melanoma
- 5% of cases
- Slow radial growth phase
- Occurs on nailbeds, palms and soles of dark-skinned and Asian persons
- Unrelated to UV exposure
- Amelanotic melanoma
- Non-pigmented nodule
- Superficial spreading melanoma
- Clinical features
- Pruritic, bleeding skin lesion
- On the back or chest in men
- On extremities in women
- Diagnosis
- ABCDE criteria – distinguishing between benign and malignant lesions
- Asymmetry
- Border irregular
- Colour irregular
- Diameter enlarged (> 5 mm)
- Evolution (changes over time)
- Ugly duckling sign
- The lesion looks different from other nevi on the same patient
- Dermoscope
- Histopathological
- Gives definitive diagnosis
- Full-thickness biopsy with 1 – 2 mm safety margin
- Shows atypical melanocytes and atypical architecture
- ABCDE criteria – distinguishing between benign and malignant lesions
- Prognosis
- Breslow depth – from the top of the stratum granulosum to the deepest invasive cell
- Presence of ulceration
- Number of mitoses
- Clark level
- The subtype
- Presence of metastasis
- Usually metastasizes to liver, lung, brain, bone
- Can metastasize into unusual locations like the heart and gallbladder
- Metastases are black
- Staging
- TNM
- T = Based on Breslow depth
- “a” – if there is no ulceration
- “b” – if there is ulceration
- N – lymph node
- Any melanoma with lymph node involvement is stage III
- M – metastasis
- Any melanoma with metastasis is stage IV
- Treatment
- Surgical excision with safety margin
- Melanoma in situ – 0,5 cm safety margin
- Breslow depth < 1 mm – 1 cm safety margin
- Breslow depth > 1 mm – 1 – 2 cm safety margin
- Non-surgical treatment
- For stage III and stage IV melanoma
- Immune checkpoint inhibitors
- Anti-CTLA-4 antibodies
- Ipilimumab
- Anti-PD-1 antibodies
- Nivolumab
- Pembrolizumab
- Anti-CTLA-4 antibodies
- Inhibitors of mutated proteins
- BRAF inhibitor – dabrafenib
- MEK inhibitor – trametinib
- Surgical excision with safety margin
13. Fungal diseases of the skin and its appendages
- Diagnosis of fungal infections
- KOH preparation -> hyphae/yeasts visible under microscope
- KOH dissolves keratin
- Culture
- Wood-light – green fluorescence UV lamp
- KOH preparation -> hyphae/yeasts visible under microscope
- Treatment of fungal infections
- Terbinafine – for dermatophytoses
- Fluconasol – for candida
- Itraconazole – for candida, dermatophytoses
- Ketoconazole – for Malassezia (pityrasis versicolor)
- Epidermomycoses
- By dermatophytes
- Risk factors
- Children
- Immunocompromised
- Diabetes
- Clinical features
- Pruritus
- Scaling
- Erythema
- Treatment
- Topical antifungals
- Terbinafine
- Azoles
- Oral antifungals
- For immunocompromised persons
- Terbinafine
- Itraconazole
- Topical antifungals
- Tinea facialis – face
- Tinea corporis – body
- Tinea cruris – inguinal area
- Tinea manuum – hands
- Usually affects two feet and one hand (syndrome)
- Because the person scratches the feet with the dominant hand
- Tinea pedis – feet
- Onychomycoses
- Discoloured and brittle nails
- Candida
- Tinea unguium
- Treatment
- Terbinafine
- Itraconazole
- Trichomycosis
- Tinea capitis – scalp
- Dandruff
- Smooth areas of hair loss
- Kerion – very inflamed abscess-like mass
- Favus – yellow crust
- Tinea capitis – scalp
- Candida
- Albicans most common
- Risk factors
- Immunosuppression
- Diabetes
- Antibiotic therapy
- Skin infections
- Oral candidiasis
- Angular cheilitis
- Vulvovaginal candidiasis
- Balanitis
- Intertrigo – infection of the skin folds
- Interdigital candidiasis
- Diaper rash
- Chronic mucocutaneous candidiasis
- Congenital impaired T-cell function
- Clinical features
- Pruritic erythematous plaque
- White layer – on mucous membranes, genital organs
- Systemic
- Candida sepsis
- Fever that doesn’t improve with antibiotics
- Invasive candidiasis
- Candida sepsis
- Pityriasis versicolor
- Risk factors
- Hot, humid environment
- Excessive sweat
- Clinical features
- Hypomelanotic macules
- Treatment
- Topical ketoconazole cream
- Ketoconazole shampoo
- Risk factors
- Cryptococcosis
- Immunocompromised patients
- Cutaneous cryptococcosis
- Molluscum contagiosum-like papules
- Can also cause pneumonia and meningitis
- Cryptococcal meningitis
- Treatment
- Fluconazole
- Amphotericin
- Flucytosine
- Aspergillosis
- Immunocompromised patients
- Necrotizing nodules
- Abscess
14. Drug allergy
- Classification according to timeline
- Immediate (< 1 hour)
- Urticaria
- Angioedema
- Rhinitis
- Bronchospasm
- Anaphylaxis
- Non-immediate (> 1 hour)
- Delayed urticaria
- Maculopapular exanthema
- Erythroderma
- Vasculitis
- Stevens-Johnson syndrome (SJS)
- Toxic epidermal necrolysis (TEN)
- Drug reaction with eosinophilia and systemic symptoms (DRESS)
- Acute generalized exanthematous pustulosis (AGEP)
- Symmetrical drug-related intertriginous and flexural exanthemas (SDRIFE)
- Immediate (< 1 hour)
- Classification according to pathomechanism
- Type I hypersensitivity
- IgE-mediated mast cell activation as a reaction to a soluble antigen
- All immediate drug allergies
- Treatment
- Eliminate culprit drug
- Antihistamines
- Type III hypersensitivity
- IgG-mediated complement activation as a reaction to a soluble antigen
- Vasculitis
- Serum sickness
- Type IVa hypersensitivity
- Cell-mediated macrophage activation as a reaction to a presented antigen
- Tuberculin reaction
- Contact dermatitis
- Type IVb hypersensitivity
- Cell-mediated eosinophil activation as a reaction to a presented antigen
- DRESS
- Maculopapular exanthema
- Erythroderma
- Type IVc hypersensitivity
- Cell-mediated T-cell activation as a reaction to a presented antigen
- Stevens-Johnsons syndrome
- Toxic epidermal necrolysis
- Type IVd hypersensitivity
- Cell-mediated neutrophils activation as a reaction to a presented antigen
- AGEP
- Type I hypersensitivity
- Drug-induced urticaria
- Drugs
- Penicillin
- Aspirin
- NSAIDs
- Drugs
- Angioedema/Quincke-oedema
- Drugs
- NSAIDs
- Aspirin
- ACE-inhibitors (not technically a drug allergy)
- Clinical features
- Facial oedema
- If laryngeal involvement – dyspnoea, inspiratory stridor
- Treatment
- Epinephrine
- Steroids
- Antihistamines
- Drugs
- Anaphylaxis
- Drugs
- Lidocaine
- Anaesthetics
- Aspirin
- Contrast
- NSAIDs
- After minutes – hours
- Clinical features
- Hypotension
- Bronchospasm, laryngeal oedema -> dyspnoea, inspiratory stridor
- Treatment
- Epinephrine
- Steroids
- Antihistamines
- Drugs
- Drug-induced vasculitis
- Drugs
- Antibiotics
- Analgesics
- Clinical features
- Painful, palpable purpura
- Urticaria
- Resolve after drug cessation
- Drugs
- Serum sickness
- Drugs
- NSAIDs
- Penicillins
- Clinical features
- Fever
- Rash
- Arthralgia
- Resolve after drug cessation
- Drugs
- Maculopapular exanthema
- On trunk, extremities
- No eosinophilia
- No systemic symptoms
- Resolve after drug cessation
- Erythroderma
- Erythema, scaling of the whole body
- Eosinophilia
- No systemic symptoms
- Resolve after drug cessation
- DRESS syndrome
- Drug-related eosinophilia and systemic symptoms
- Also called drug-induced hypersensitivity syndrome
- Drugs
- Allopurinol
- Antiepileptics
- Antibiotics
- Risk factors
- Older age
- Renal failure
- Certain HLA alleles
- Clinical features
- Fever
- Pruritic morbilliform rash
- Facial oedema
- Multiorgan failure can occur
- Fatal in 10%
- Treatment
- Drug cessation
- Steroids
- Drug-related eosinophilia and systemic symptoms
- Toxic epidermal necrolysis (TEN) and Stevens-Johnson syndrome (SJS)
- If < 10% of skin surface is involved -> SJS
- If 10 – 30% of skin surface is involved -> SJS/TEN overlap
- If > 30% of skin surface is involved -> TEN
- Drugs
- Antibiotics
- Antiepileptics
- Sulpha drugs
- Allopurinol
- Risk factors
- HIV infection
- Clinical features
- High fever
- Painful erythematous macules
- -> Lesions form bullae
- -> Extensive, full-thickness epidermal necrosis and sloughing
- Resembles superficial burns
- Mucous membranes almost always involved
- Stomatitis
- Oral ulcers
- Conjunctivitis
- Urethritis
- Circulatory shock
- Diagnosis
- Clinical
- Positive Nikolsky sign
- Treatment
- Supportive care
- Drug cessation
- High-dose steroid
- IV immunoglobulin
- GM-CSF
- Mortality 10 – 50%
- Acute generalized exanthematous pustulosis (AGEP)
- Drugs
- Penicillins
- Quinolones
- Sulpha drugs
- Clinical features
- Erythematous, oedematous pustules
- Begin in intertriginous areas, progress over the whole body
- Fever
- Treatment
- Drug cessation
- Antipyretics
- Oral steroids
- Drugs
15. Urticaria
- Also called hives
- Etiology
- Basically anything, but often idiopathic
- Physical urticaria
- Most common
- Pressure
- Dermatographic urticaria
- Elevated/decreased body temperature
- Sweating
- Sun-exposure
- Allergic urticaria
- Foods
- Fish
- Shellfish
- Nuts
- Eggs
- Drugs
- Penicillin
- Aspirin
- ACE inhibitors
- NSAIDs
- Inhalants
- Foods
- Autoimmune urticaria
- Vasculitic urticaria
- Infectious urticaria
- Others
- Insect bites/stings
- Pregnancy
- Exercise
- Additives to food, dermatological products, soaps, etc.
- Classification
- Acute < 6 weeks
- 95% of acute cases resolve
- 5% progress into chronic
- Chronic > 6 weeks
- 25% of all urticaria patient
- Etiology can’t be established in many cases
- Acute < 6 weeks
- Pathomechanism
- Local capillary vasodilation and transudation of fluid -> intradermal oedema
- Mostly due to histamine, bradykinin, complement factors
- Mast cell degranulation occurs
- In some cases, due to hypersensitivity type I
- Clinical features
- Pruritus
- Diffuse urtica/wheals
- Circumscribed, sharply demarcated
- Erythematous plaques, sometimes with central clearing
- Individual lesions disappear after 24 hours
- Angioedema may also occur
- Diagnosis
- Extensive history is essential
- Any new dermatological products, drugs, etc.
- Lab tests
- Inflammatory markers
- Autoantibodies
- Infections
- Prick test
- Patch test
- Extensive history is essential
- Treatment
- For chronic
- Oral antihistamines
- Cyclosporine
- Leukotriene antagonist
- Omalizumab (anti-IgE)
16. Scabies, pediculosis
- Scabies
- Sarcoptes scabiei var hominis
- Obligate human parasite
- Transmission by direct physical contact or contact with infected clothes
- Highly contagious
- Incubation period 3 – 6 weeks
- Risk factors
- Nursing homes
- Childcare facilities
- Prisons
- Pathomechanism
- Female mites burrow into stratum corneum, lays eggs and feces
- Feces and dead mites trigger type IV hypersensitivity
- Clinical features
- Intense pruritus, especially at night
- Skin lesions
- Elongated erythematous papules
- 2 – 10 mm burrows (elevations in the skin)
- Vesicles
- Excoriation due to itching
- Predilection sites – warm areas with thin skin
- Wrists
- Fingers
- Male genitalia
- Diagnosis
- Dermoscope
- Clinical
- Treatment
- Permethrin 5% lotion
- Applied to the whole body and left on the skin for 8 – 12 hours
- The rest of the family should be treated too
- Lindane 1% lotion
- Oral ivermectin
- Symptomatic treatment of pruritus
- Oral antihistamines
- Topical steroids
- Permethrin 5% lotion
- Sarcoptes scabiei var hominis
- Pediculosis
- Lice infection
- Transmission by direct physical contact or indirect contact with infected clothes, etc.
- Risk factors
- Crowded places
- School
- Homeless
- Pathomechanism
- Delayed allergic reaction to lice saliva
- May be asymptomatic for weeks while sensitization occurs
- Pediculosis capitis
- Pediculus humanus capitis (head louse)
- Most common in children
- Clinical features
- Scalp/neck pruritus
- Louse eczema on back of neck
- Diagnosis
- Detection of lice on the scalp or hair
- Treatment
- Permethrin shampoo
- Lindane shampoo
- Malathion shampoo
- Then mechanical removal with a fine-toothed comb
- Cleaning of all hair tools, bedding, clothes, etc.
- Pediculosis corporis
- Pediculus humanus corporis (body louse)
- Most common in crowded, unsanitary living conditions
- Clinical features
- Pruritus
- Bites on skin
- Scratching lines
- Diagnosis
- Detection of lice in clothing
- Treatment
- Topical permethrin
- Cleaning of all bedding, clothes, etc.
- Pediculosis pubis
- Pthirus pubis (crab louse)
- Transmitted by sexual contact
- Most common in teenagers and young adults
- Pruritus in genital area
- Blue-purple macules in patients with chronic infection
- Diagnosis
- Detection of lice in pubic hair
- Treatment
- Topical permethrin
- Cleaning of all bedding, clothes, etc.
17. Pigmented nevi
- A nevus is a benign lesion of melanocytes in the skin or oral mucosa
- Can be pigmented or non-pigmented (most are pigmented)
- Histological classification
- Junctional nevi
- Flat, well-demarcated brown macules
- Grows in the epidermis at the dermal-epidermal junction
- Compound nevi
- Elevated
- Grows in the epidermis at the dermal-epidermal junction and in the dermis
- Dermal nevi
- Elevated
- May be hard and grow hair
- Grows in the dermis only
- Junctional nevi
- Clinical classification
- Congenital
- Small (< 1,5 cm)
- Medium
- Giant (> 20 cm)
- Acquired
- Common acquired nevus
- < 6 mm
- Symmetric
- Homogenous surface
- Even pigmentation
- Round or oval shape
- Sharply demarcated border
- Atypical/dysplastic nevus
- Share some similarities to melanoma
- Must be differentiated from melanoma
- Fried egg or target-shaped
- May evolve
- Atypical colour
- Irregular, poorly demarcated
- Spitz nevus
- Not brown, rather pink, tan, red, etc.
- In children
- Halo nevus
- Nevus surrounded by halo of depigmentation
- Reed nevus
- Very dark
- On limbs
- Nevus spilus
- Tan macule speckled with smaller, darker macules
- Blue nevus
- Common acquired nevus
- Congenital
- Dysplastic nevus syndrome
- Also called familial atypical multiple mole and melanoma syndrome (FAMMM)
- High number (> 50) of common and atypical nevi and family history of melanoma
- Almost 100% of developing melanoma
- Diagnosis
- History
- Family history?
- History of skin lesions?
- History of sunburns?
- When did nevus appear?
- Has it changed?
- Physical examination
- Assess skin type
- Examination with dermoscope
- ABCDE
- Ugly duckling sign
- History
18. Vasculitides
- Cutaneous small vessel vasculitis = cutaneous leukocytoclastic vasculitis
- Small vessel vasculitides with cutaneous involvement
- Most cases are idiopathic
- Types
- Immune complex mediated vasculitides
- Cryoglobulinaemic vasculitis
- IgA vasculitis = Henoch Schönlein purpura
- Urticarial vasculitis
- ANCA-associated vasculitides
- Granulomatosis with polyangiitis
- Eosinophilic granulomatosis with polyangiitis
- Immune complex mediated vasculitides
- Common clinical features
- Palpable purpuras
- Erythematous papules
- Urticaria
- Systemic symptoms
- Fever
- Myalgia
- Arthralgia
- Renal disease
- Prognosis
- 90% spontaneously resolve within months
- 10% become chronic or recurrent
- Cryoglobulinaemic vasculitis
- Cryoglobulins = immunoglobulins that precipitate in the cold
- They precipitate within the walls of small vessels
- Etiology
- Viral infections
- Autoimmune connective tissue diseases
- Haematological malignancies
- Clinical features
- Palpable purpura (in 90%)
- Myalgia
- Arthralgia
- Peripheral neuropathy
- Glomerulonephritis
- Diagnosis
- Examination of cryoglobulins in blood during attack
- Treatment
- Treat underlying disease
- If severe
- Steroids
- Immunosuppressants
- Biological therapy
- Cryoglobulins = immunoglobulins that precipitate in the cold
- IgA vasculitis = Henoch-Schönlein purpura
- IgA deposit in the vessels
- Typically affect children after a respiratory tract infection
- Clinical features (typical tetrad)
- Palpable purpura (in 100%)
- Arthritis
- Abdominal pain
- Haematuria
- Treatment
- Self-limiting in most cases – no treatment needed
- NSAIDs
- Steroids if severe
- Urticarial vasculitis
- Persistent urticaria
- Associated with autoimmune connective tissue diseases
- Can be due to hypocomplementemia (deficiency of complement factors)
- In which case there is also systemic involvement
- Clinical features
- Recurrent episodes of painful, persistent urticarial lesions that last > 24 hours
- Angioedema can occur
- Treatment
- Antihistamines
- Steroids
- NSAIDs
- Dapsone
- Granulomatosis with polyangiitis
- Potentially lethal
- Clinical features
- Skin symptoms (in 50%)
- Papules
- Purpuras
- Oral ulcers
- Chronic rhinosinusitis
- Lower respiratory tract infections
- Glomerulonephritis
- Skin symptoms (in 50%)
- Treatment
- Steroids
- Immunosuppressants
- Eosinophilic granulomatosis with polyangiitis
- Clinical features
- Skin symptoms (in 50%)
- Nodules
- Palpable purpuras
- Severe asthma
- Allergic rhinitis
- Respiratory tract infections
- Skin symptoms (in 50%)
- Treatment
- Steroids
- Immunosuppressants
- Clinical features
- Polyarteritis nodosa
- Medium-sized vessel vasculitis
- Clinical features
- Skin symptoms (in 25%)
- Palpable purpuras
- Punched-out ulcers
- Coronary artery disease
- Renal disease
- Polyneuropathy
- Skin symptoms (in 25%)
- Treatment
- Steroids
- Immunosuppressants
19. Contact dermatitis
- Contact dermatitis
- Types
- Important types
- Allergic contact dermatitis
- Irritant contact dermatitis
- Phototoxic contact dermatitis
- Photoallergic contact dermatitis
- Not so important types
- Seborrheic dermatitis
- Infectallergic dermatitis
- Perioral dermatitis
- Stasis dermatitis
- Important types
- Clinical features (rash)
- Acute
- “Sunburn type”
- Erythema
- Oedema
- Vesicles
- Urtica
- Pruritus
- “Exanthema type”
- Macule
- Papule
- Plaque
- Wheal
- “Sunburn type”
- Subacute
- Erythema
- Fissure
- Scaling
- Chronic
- Hyperkeratosis
- Fissure
- Scaling
- Lichenification
- Acute
- Diagnosis
- Patch test
- Contains haptens in patches which are applied to the back
- Reading at 48, 72, 168 hours
- Contains common haptens according to European and local standards
- Cosmetic ingredients
- Plants
- Metals
- etc.
- + = erythema, oedema
- ++ = papule, vesicle
- +++ = bulla, erosion, ulcer
- Crescendo – reaction worsens with time
- Typical for allergic contact dermatitis
- Decrescendo – reaction improves with time
- Typical for irritant contact dermatiti
- Patch test
- Treatment
- Identification of cause
- Topical
- Emollients (moisturizers)
- Corticosteroids
- Calcineurin inhibitors
- Systemic
- Antihistamines
- Corticosteroids
- Types
- Allergic contact dermatitis
- Etiology
- Poison ivy
- Nickel
- Chromium
- Perfumes
- Soaps
- Cosmetics
- Tattoos
- Latex
- Rubber
- Topical medications
- Budesonid
- Pathomechanism
- Type IVa hypersensitivity
- Mediated by a hapten, which binds to an endogenous protein and becomes an immunogenic allergen
- The body is sensitized to the allergen upon first contact
- With repeated contact a rash develops
- Etiology
- Irritant contact dermatitis
- Etiology
- Solvents – remove lipids in the stratum corneum
- Like alcohol
- Acids, bases, salts – destroy proteins in the stratum corneum
- Dust – mechanically destroys stratum corneum
- Excessive hand washing
- Mineral oils
- Detergents
- Metals
- Dry air
- Warm air
- Cold air
- Solvents – remove lipids in the stratum corneum
- Pathomechanism
- Not immune-mediated
- Due to direct irritation -> leads to damage of stratum corneum
- -> release of inflammatory mediators
- Etiology
- Phototoxic contact dermatitis
- More common than photoallergic type
- Etiology
- Topical
- Bergamot
- Psoralen (in plants)
- Tar
- Systemic
- Tetracycline
- Sulphonamides
- Quinolones
- HCTZ
- Topical
- Pathomechanism
- UV radiation converts a photosensitive molecule into a cytotoxic one
- Only occurs on sun-exposed skin
- Phototoxic contact dermatitis is exploited in psoralen-UVA (PUVA) treatment
- Photoallergic contact dermatitis
- Less common than phototoxic type
- Etiology
- PABA
- Perfumes
- Aromatic oils
- Benzocaine
- Pathomechanism
- UV radiation converts a photosensitive molecule (a photoallergen) into an allergen -> type IV hypersensitivity
- Only occurs on sun-exposed skin
20. Precancerous lesions and intraepidermal carcinoma
- Precancerous lesions
- Lentigo maligna
- Actinic keratosis
- Cutaneous horns
- Leucoplakia
- Intraepidermal carcinoma/carcinoma in situ
- Bowen disease
- Erythroplasia of Queyrat
- Paget disease
- Lentigo maligna
- Precancerous lesion of dysplastic melanocytes
- Occurs in elderly
- Risk factor: UV exposure
- Darkly pigmented macule
- On sun-exposed areas
- Face, neck
- Irregular borders
- 1 mm – 2 cm
- Irregular colour
- On sun-exposed areas
- Treatment
- Surgical excision with safety margin
- Actinic keratosis
- Precancerous lesions of squamous cells
- Occurs in elderly with light skin
- Risk factor: UV exposure
- Clinical features
- Small lesion with rough surface
- -> lesion grows and becomes erythematous and scaly
- On sun-exposed areas
- May develop into a cutaneous horn
- Treatment
- Few lesions
- Cryotherapy
- Many lesions
- 5-FU
- Imiquimod
- Prevention with sunscreen
- Few lesions
- Leucoplakia
- Hyperkeratosis and dysplasia of epithelium and mucous membranes
- Risk factors
- Smoking
- Alcohol
- Clinical features
- White plaque that cannot be scraped off
- Most commonly in oral cavity
- Differential diagnosis
- Oral candidiasis
- Oral hairy leukoplakia
- Treatment
- Avoidance of risk factors
- Cryotherapy
- Bowen disease
- Squamous cell carcinoma in situ of skin
- Risk factors
- UV exposure
- HPV 16, 18
- Arsenic
- Clinical features
- Erythematous and scaly lesion
- Irregular shape, sharp borders
- On sun-exposed areas
- Treatment
- 5-FU
- Imiquimod
- Erythroplasia of Queyrat
- = Bowen disease of glans penis
- Squamous cell carcinoma in situ of penile mucosa
- Risk factors
- Chronic inflammation
- HPV 16, 18
- Clinical features
- Sharply demarcated, non-healing plaques or papules
- May ulcerate or bleed
- Treatment
- 5-FU
- Imiquimod
- Paget disease of the breast
- Ductal carcinoma in situ of the nipple and areola
- Clinical features
- Erythematous, scaly, vesicular rash
- Pruritus
- Burning
- Treatment
- Surgical removal
21. Cutaneous and mucosal manifestations and treatment of syphilis
- Sometimes called lues
- Treponema pallidum
- Risk factors
- Men who have sex with men
- Promiscuity
- Unprotected sex
- Incubation period 10 – 90 days (average 21)
- Has 4 characteristic stages
- Primary syphilis
- Characterised by a special lesion called a chancre
- Chancres occur at the site where the bacterium enters the body
- It’s a painless, firm ulcer with indurated borders and a smooth base
- Chancres resolve spontaneously without scarring after 3 – 6 weeks
- Secondary syphilis
- Known as the “great imitator” as its skin symptoms resemble those of many other skin diseases
- Both systemic and mucocutaneous lesions
- Begins 8 – 12 weeks after primary infection
- Lasts 2 – 6 weeks
- Disseminated, symmetric rash
- Polymorphic, i.e. can take on many appearances
- Typically nonpruritic macular or papular rash
- Reddish-brown
- Roseola syphilitica = macules on trunk and flexor aspects of the extremities
- Corona veneris
- Maculopapular lesions
- On forehead or back of neck
- Clavus syphiliticus = maculopapular lesions on palms and soles
- Mucous patches
- White patches on mucous membranes
- Condyloma lata
- Broad-based, wart-like papular erosions
- In anogenital region, intertriginous folds, oral mucosa
- Patchy alopecia
- Leucoderma syphiliticum
- Hypopigmentation
- Necklace of Venus = hypopigmentation around the neck
- Differential diagnosis: pityriasis versicolor
- Non-cutaneous and non-mucosal symptoms
- Pharyngitis
- Iritis
- Hepatitis
- Generalized nontender lymphadenopathy
- Meningitis
- Latent syphilis
- The patient is seropositive but there are no symptoms
- Can last months, years or the rest of the patient’s life
- There are four outcomes
- The disease resolves and the patient becomes healthy
- The disease reactivates as secondary syphilis
- The disease progresses into tertiary syphilis
- The patient dies before any of these outcomes occur
- Tertiary syphilis
- Occur in approx. 30% of untreated patients in the latent stage
- Late benign syphilis
- Gummas
- Destructive and ulcerative granulomatous lesions with necrotic centre
- Can occur anywhere on or in the body, even on organs and bones
- Nodules
- Psoriasiform granulomatous lesions
- Gummas
- Cardiovascular syphilis
- Aortitis with resulting aneurysm of the aorta
- Dilated aortic root
- Neurosyphilis
- Early neurosyphilis
- Meningitis
- Stroke
- Late neurosyphilis
- Tabes dorsalis
- Demyelination of the dorsal column and dorsal root ganglia
- Causes a broad-based ataxia
- Dysesthesia
- General paresis
- Widespread cerebellar atrophy
- Dementia
- Argyll Robertson pupil (Bilateral miosis, pupils don’t react to light)
- Tabes dorsalis
- Early neurosyphilis
- Diagnosis
- Direct visualization of treponema
- In the primary stage, when the serological tests below can be negative
- Darkfield microscopy
- Specimen from a lesion
- Nontreponemal tests – for screening
- RPR
- VDRL
- Sensitive, not specific
- Treponemal test – for confirming the diagnosis
- TPPA
- FTA-ABS
- Specific, not sensitive
- Direct visualization of treponema
- Primary syphilis
-
- Treatment
- For prevention, primary, secondary and early latent syphilis
- 2,4 million units of benzathine penicillin G intramuscularly – single dose
- For tertiary (except neurosyphilis) and late latent syphilis
- 2,4 million units of benzathine penicillin G IM – once weekly for three weeks
- For neurosyphilis
- IV penicillin G for 10 to 14 days
- Jarisch-Herxheimer reaction may occur
- Systemic reaction to bacterial endotoxins
- Is usually self-limiting
- In case of penicillin allergy
- Doxycycline
- Desensitization to penicillin, then use penicillin as normal
- For prevention, primary, secondary and early latent syphilis
- Treatment
22. Diagnosis and treatment of gonorrhoea
- Epidemiology
- Young adults
- Neisseria gonorrhoeae
- Clinical features in men
- Incubation time – 2 to 10 days
- 15% are asymptomatic
- Acute gonococcal urethritis
- Discomfort
- Dysuria
- Purulent discharge
- Chronic gonococcal urethritis
- Complications
- Epididymitis
- Seminal vesiculitis
- Prostatitis
- Clinical features in women
- Incubation time – days to weeks
- 30 – 60% are asymptomatic
- Acute salpingitis
- Dysuria
- Increased discharge
- Abnormal bleeding
- Complications
- Pelvic inflammatory disease
- Disseminated gonococcal infection (arthritis-dermatitis syndrome)
- Occurs in 2% of cases
- 85% are women
- Intermittent fever
- Migratory arthritis
- Pain spreads from one joint to another
- Skin lesions
- Flea bite-like papules
- Haemorrhagic pustules on palms, soles
- Gonococcal conjunctivitis (in neonates)
- Etiology
- Direct contact from genitalia to hand to eye
- Perinatally
- Treatment
- Silver nitrate eye drops
- Etiology
- Diagnosis
- PCR (a type of NAAT)
- First choice
- Of first urine – in men
- Of vaginal swab – in women
- Of pharyngeal swab – if oral sex occurred
- Gram staining
- Culture
- PCR (a type of NAAT)
- Treatment
- Ideal treatment for gonorrhoea:
- Treats the gonorrhoea
- Treats and any coexisting syphilis and chlamydia
- Is single dose
- Covers resistant strains of gonorrhoea (many are resistant to cephalosporins)
- Either
- Single-dose ceftriaxone IM + single-dose azithromycin PO
- or single-dose cefixime PO + single-dose ciprofloxacin PO
- Postgonococcal urethritis can occur
- Due to secondary colonization with mycoplasma and chlamydia
- Treatment: tetracycline
- Ideal treatment for gonorrhoea:
23. Acne and its treatment
- Common acne = Acne vulgaris
- (comedo/comedones = plugged hair follicle (pore))
- Risk factors
- Genetic predisposition
- Hormonal changes
- Puberty
- Menstrual cycle
- Certain foods
- Smoking
- Skin products that block pores
- Pathomechanism
- Hyperactivity of sebaceous glands
- Hyperkeratosis of follicular keratinocytes
- Bacterial hypercolonization
- Propionibacterium acnes (= cutibacterium acnes)
- Inflammation
- Clinical features
- On face, shoulders, upper chest, back
- Primary lesions
- Non-inflammatory acne – comedonal acne
- Closed comedones = whiteheads
- Small papules that contain whitish material
- The whitish material is keratin and sebum
- Open comedones = blackheads
- Small papules with black material
- The black material is oxidized keratin and sebum
- Closed comedones = whiteheads
- Inflammatory acne
- Papular acne
- Pustular acne
- Nodular acne (> 5 mm)
- Non-inflammatory acne – comedonal acne
- Secondary lesions
- Erythema
- Hyperpigmentation
- Scarring
- Hypertrophic scars
- Depressed scars
- Pitted scars
- Special types of acne
- Acne inversa = hidradenitis suppurativa
- Inflammation of hair follicles due to physical blockage by skin folds, etc
- Acne fulminans
- Sudden onset, very severe acne
- In teenage boys
- Acne inversa = hidradenitis suppurativa
- Diagnosis
- Anamnesis
- Clinical examination
- Laboratory examinations
- Exclude hyperandrogenism, like PCOS, CAH, androgen-producing tumors
- Treatment
- Options
- Topical benzoyl peroxide
- Comedolytic
- Bactericidal
- Retinoids
- Oral or topical
- Tretinoin, isotretinoin, adapalene
- Normalize keratinocyte differentiation
- Decrease sebum production
- Highly teratogenic
- Females must produce negative pregnancy test and use at least one, optimally two methods of contraception
- Hepatotoxic
- Liver enzymes, cholesterol must be monitored
- Antibiotics
- Oral (doxycycline, minocycline)
- Topical (erythromycin, clindamycin)
- Bactericidal
- Decrease inflammation
- Oral contraceptives
- In females
- Can be added in treatment failure
- Topical combination therapy
- Benzoyl peroxide + topical retinoid
- Benzoyl peroxide + topical antibiotic
- Benzoyl peroxide + topical retinoid + topical antibiotic
- Topical benzoyl peroxide
- Treatment algorithm
- Mild cases
- Topical benzoyl peroxide
- Topical retinoid
- Topical combination therapy
- Moderate cases
- Topical combination therapy
- Oral antibiotic + topical combination therapy
- Severe cases
- Oral retinoid
- Mild cases
- Options
24. Local therapy in dermatology
- Unilateral treatment allows for easier treatment response evaluation than with systemic treatment
- Topical preparations/formulations consist of a drug in a non-active base/vehicle
- Drugs used on skin must be dissolved or suspended in a vehicle
- The choice of drug depends on the diagnosis
- The choice of vehicle depends on the state of the skin
- The drug will be transferred from the vehicle to stratum corneum
- The base determines the rate at which the drug is absorbed through the skin
- Vehicles
- Liquid vehicles
- Water
- Ethanol
- Glycerol
- Solid vehicles (powders)
- Zinc oxide
- Titanium oxide
- Talc
- Starch
- Fatty vehicles (greases)
- Vegetable fats
- Animal fats
- Mineral oils
- Petrolatum
- Liquid vehicles
- Types of topical preparations
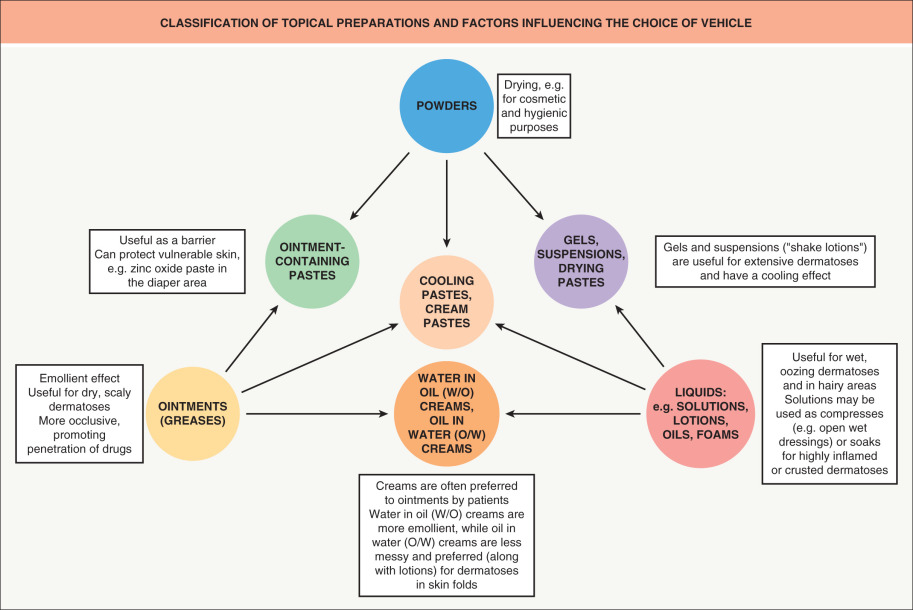
- Topical preparations
- Solution
- Drug dissolved in a liquid solvent like alcohol or water
- Convenient to apply (can be applied with a dropper)
- Lotions
- Water-based emulsion
- Thicker than solution
- Good for hairy skin
- They cool inflammatory lesions and dry exudative lesions
- Creams
- A semisolid emulsion of water in oil or oil in water
- Thicker than lotion
- Good for weeping lesions
- When applied with wet compress -> good for inflamed skin
- Ointments
- Semisolid grease or oil, without water
- Good for scaly or dry lesions
- When applied with wet compress -> good for inflamed skin
- Gels
- Soft, semisolid preparation
- Liquefy on contact with the skin
- Foam
- Aerosolized solution with a pressurized propellant
- Good for hairy skin
- Powders
- Solid
- For lesions in moist or intertriginous areas
- Cooling paste
- Contains oil, water and powder
- Often contains zinc oxide
- Cools inflamed skin
- Solution
- Dressings
- Protect open lesions, facilitate healing, increase drug absorption
- Non-occlusive dressings (wet dressings)
- Dressings wetted with saline or water
- Applied to the lesion and removed when the solution has evaporated
- Good for thick or crusted lesions
- Good for oozing lesions
- Occlusive dressings
- Increase the absorption and effectiveness of topical therapy
- Can be applied over topical preparations to increase absorption
- Can be applied to open wounds to allow them to heal
- Moisturizing agents (emollients)
- Restore water and oil to skin and help maintain skin hydration
- More effective in slightly wet skin, like after a shower
- Available as lotions, creams, ointments, etc.
- Indicated in dry skin conditions
- Contains occlusives and humectants
- Humectants
- These agents attract water, increasing the water-holding capacity of the stratum corneum
- Glycerine
- Urea
- Lactic acid
- Glycolic acid
- Occlusives
- Form a physical barrier to prevent water loss
- Waxes
- Petrolatum
- Oils
- Drying agents (powders)
- To treat excessive moisture, like between skin folds, the groin, etc
- Corn starch
- Talc
- Topical agents to alleviate pruritus
- Pramoxine
- Hydrocortisone
- Menthol
- Phenol
- Keratolytics
- These agents facilitate exfoliation of epidermal cells
- Used to treat hyperkeratotic diseases like
- Psoriasis
- Seborrheic dermatitis
- Acne
- Urea
- Salicylic acid
- Lactic acid
- Glycolic acid
- Steroids
- Widely used in dermatology
- Indications
- Cutaneous lupus erythematosus
- Psoriasis
- Lichen
- Contact dermatitis
- Atopic dermatitis
- Allergic skin reactions
- Mostly used steroids
- Hydrocortisone (low potency)
- Triamcinolone (medium potency)
- Clobetasol (high potency)
- Side effects
- Skin atrophy
- “Steroid acne”
- Striae
- Contact allergy
- “Steroid rosacea” = perioral dermatitis
- When potent steroids are used on the face
- Telangiectasias
- Papules, pustules
- Topical antibiotics
- Mostly used in acne
- Tetracyclines
- Metronidazole
- Erythromycin
- Clindamycin
- Bacitracin
- Silver nitrate
- Low concentration – debride wounds
- High concentration – cauterizes bleedings in wounds
- Imiquimod
- Immune regulator
- Indications
- Warts
- BCC
- Actinic keratosis
- Topical calcineurin inhibitors
- Tacrolimus
- Pimecrolimus
- Indications
- Atopic dermatitis
- 5-fluorouracil
- Indications
- Actinic keratosis
- BCC
- Warts
- Indications
- Fingertip units (FTU)
- 1 FTU = the amount of topical preparation expressed from a tube when applied from the distal skin-crease to the tip of the index finger
- 1 FTU is approx. 0,5 g
- 1 FTU covers approx. 300 cm2, which is enough for one hand
- 2,5 FTU covers the face and neck
- Fingertip units are useful when telling patients how much they should use of a preparation
B. topics
1. The structure of the skin and its function
- 2 m2 and 4 kg
- Structure
- Epidermis
- Stratum corneum
- Stratum lucidum
- Stratum granulosum
- Stratum spinosum
- Stratum basale
- Dermo-epidermal junction
- Basement membrane
- Dermis
- Papillary dermis
- Loosely arranged collagen
- Supplies epidermis with nutrients through dermal papillae
- Reticular dermis
- Densely packed reticular, elastic, collagen fibres
- Connective tissue
- Dense innervation
- Papillary dermis
- Subcutis/hypodermis
- Fat
- Connective tissue that anchors the skin to the deep fascia
- Epidermis
- Function
- Mechanical, chemical, physical, microbial barrier
- Desmosomes attach keratinocytes to each other
- Hemidesmosomes attach keratinocytes to basement membrane
- Protect against UV radiation
- Melanocytes
- Immune function
- Skin associated lymphatic tissues (SALT)
- Langerhans cells – tissue macrophages in stratum spinosum
- Recruits the immune system when something crosses the barrier
- Vitamin D synthesis
- Sensory
- Touch
- Meissner corpuscles – fine touch
- Ruffini corpuscles – pressure
- Vibration
- Pacinian corpuscles
- Temperature and pain
- Free nerve endings
- Touch
- Temperature regulation
- Mechanical, chemical, physical, microbial barrier
2. Alopecias
- Phases of hair growth
- Anagen phase – hair growth
- Catagen phase – transition phase
- Telogen phase – resting phase
- Repeat
- Types of alopecia
- Diffuse alopecia
- Androgenetic alopecia
- Most common cause
- In androgen-sensitive hair follicles
- Bitemporal scalp in men
- Frontal scalp in women
- Androgens shorten the anagen phase
- Telogen effluvium
- Endocrine disorders
- Drugs
- Malnutrition
- Severe stress
- Androgenetic alopecia
- Circumscribed alopecia
- Alopecia areata
- Autoimmune
- Bacterial infection
- Stress
- Syphilitic alopecia
- Scarring alopecia
- Trauma
- Burn
- Ulcerating skin diseases
- Alopecia areata
- Diffuse alopecia
- Treatment
- Finasteride
- Minoxidil
- Hair transplant
- PUVA
- Imiquimod
- Tacrolimus
- etc.
3. Dermatomyositis
- = inflammatory myopathy with skin involvement
- In older adults
- In children (juvenile dermatomyositis)
- Etiology
- Autoimmune
- Associated with malignancies (in adults)
- Clinical features
- Muscle atrophy and weakness
- Heliotrope rash
- Erythematous/purple rash of periorbital area
- Gottron papule
- Erythematous papules on knuckles
- Shawl erythema
- Erythema of neck, upper trunk
- Diagnosis
- Creatine kinase
- LDH
- Autoantibodies
- Muscle biopsy
- Treatment
- Steroids
4. Symptoms, diagnosis and treatment of non-gonorrhoeic urethritis
- Epidemiology
- Chlamydia is most common STD (except HPV)
- Etiology
- Chlamydia trachomatis D-K
- Mycoplasma
- Ureaplasma
- Trichomonas
- Clinical features in females
- 90% are asymptomatic
- Urethritis
- Mucopurulent discharge
- Postcoital bleeding
- Extra in trichomonas
- Yellow-greenish discharge
- Abnormal vaginal odour
- Clinical features in males
- 50% are asymptomatic
- Prostatitis
- Epididymitis
- Complication: Reiter syndrome/reactive arthritis
- Most commonly after chlamydial urethritis
- Associated with HLA-B27
- Affects young males
- Clinical triad
- Arthritis
- Conjunctivitis
- Urethritis
- Diagnosis
- PCR of vaginal swab or first catch urine
- Mycoplasma
- Chlamydia
- (also Gonorrhoea)
- Whiff test – trichomoniasis
- KOH added – fishy odour
- Microscopy
- PCR of vaginal swab or first catch urine
- Treatment
- Chlamydia
- Single dose 1g PO azithromycin
- Trichomonas
- Single dose 2g PO metronidazole
- Others
- Doxycycline
- Azithromycin
- Chlamydia
5. Clinical forms and treatment of Kaposi sarcoma
- Caused by HHV8
- Malignant tumor of endothelial cells
- 4 types
- Classic – in older males
- Endemic – in Africa
- Immunosuppressive therapy-related
- AIDS-related
- Clinical features
- Multiple cutaneous lesions
- Purplish macules -> patches -> papules -> plaques -> nodules
- Rapidly growing
- Initially seen on face, oral cavity or chest
- Organs can be involved
- Multiple cutaneous lesions
- Treatment
- Vinblastine
- Radiotherapy
- Treat underlying HIV
6. Lichen planus
- Chronic inflammatory disease of unknown etiology
- Associated with hep C
- Cutaneous lichen planus
- 5 P’s
- Purple
- Planar
- Pruritic
- Polygonal
- Papules
- Wickham striae – characteristic white lines
- 5 P’s
- Mucosal lichen planus
- Wickham striae in oral cavity
- Painful, erosive lesions in oral cavity
- Can also affect oesophagus
- Genital lichen planus
- Papules on genital organs
- Treatment
- Topical/oral steroids
- Phototherapy
7. Clinical outcome and symptoms of AIDS
- General cutaneous clinical features
- Opportunistic infections
- Oral/oesophageal candidiasis
- Cryptococcus
- Aspergillosis
- Dermatophytes
- Herpes simplex infections
- Psoriasis
- Herpes zoster
- AIDS can cause reactivation
- Molluscum contagiosum
- Atopic dermatitis
- Seborrheic dermatitis
- Drug reactions
- More severe in AIDS
- Often cause morbilliform rash
- Opportunistic infections
- Specific cutaneous clinical features
- Acute HIV syndrome
- Before AIDS develops
- Maculopapular morbilliform rash
- Eosinophilic folliculitis
- Pruritic, erythematous papules on follicles
- Affects the upper body only
- Oral hairy leucoplakia
- EBV
- White plaques
- On inferolateral surface of tongue
- Bacillary angiomatosis
- Bartonella
- Multiple erythematous papules and nodules
- Bleed easily
- Kaposi sarcoma
- Acute HIV syndrome
8. Benign tumours of the skin
- Epidermal origin
- Seborrheic keratosis
- Most common benign skin tumor in elderly
- Immature keratinocytes
- Clinical features
- Multiple darkly pigmented, soft papules/plaques
- Greasy, wax-like
- “Stuck-on” appearance
- May be pruritic
- May bleed easily
- Increase in number and size with time
- Treatment
- No treatment necessary
- Cryotherapy, laser, excision for cosmetic reasons
- Keratoacanthoma
- On sun-exposed skin
- From pilosebaceous glands
- Rapid growths for a few weeks -> then spontaneous resolution after months
- Treatment
- Excision
- Radiotherapy
- Sebaceous nevus
- Apocrine nevus
- Seborrheic keratosis
- Benign mesenchymal tumors
- Dermatofibroma
- Fibroblasts
- Slowly growing
- Skin-coloured or brownish nodules
- Most commonly on lower extremities
- Fitzpatrick sign – when squeezed the surface retracts inwards
- Characteristic for dermatofibroma
- Treatment only for cosmetic reasons
- Acrochordon (skin tag)
- Lipoma
- Slow growing
- Round
- Soft
- “Rubbery”
- Leiomyoma
- Dermatofibroma
- Vascular tumors
- Angioma
- Haemangioma
- Pyogenic granuloma
- Benign vascular tumor
- Soft, round, bright red tumor
- Bleeds easily
- Skin adnexal benign tumors – of accessory skin structures like glands, hair follicles
- Syringoma
- Hidradenoma
- Trichoepithelioma
- Dermal eccrine cylindroma
- Solid, skin-coloured nodules
- On head, neck, face
- Other
- Epidermoid cyst
- Pigmented nevus
- Neurofibroma
- Neurofibromatosis
9. Paraneoplastic skin disorders
- Indicate underlying malignancy
- Occur due to tumor-associated immunological and endocrine mechanisms
- Autoimmune reactions
- Growth factor synthesis
- etc.
- Often therapy-resistant
- Obligate paraneoplastic disorders
- Leser-Trélat sign
- Multiple, sudden-onset seborrheic keratoses
- Solid cancers, especially GI tract
- Malignant acanthosis nigricans
- EGF production
- Asymmetric velvety thickening and hyperpigmentation of skin folds
- Pruritus
- GI, lung cancers
- Erythema gyratum repens
- Adenocarcinoma
- Acrodermatitis psoriasiformis
- Upper airway cc
- Hypertrichosis acquisita
- Acrokeratosis bazex/acrokeratosis paraneoplastica
- Psoriasiform lesions
- Upper airway cc or GI cc
- Paraneoplastic pemphigus
- Leser-Trélat sign
- Facultative paraneoplastic disorders
- Pyoderma gangrenosum
- Painful, rapidly progressive ulcerated lesions
- Also in Crohn’s
- Bullous pemphigoid
- Dermatomyositis
- Sweet syndrome
- Painful erythematous papules, plaques, nodules
- Herpes zoster generalisatus
- Acquired, generalized ichthyosis
- Pyoderma gangrenosum
10. Rosacea, rhinophyma
- Rosacea
- Chronic inflammatory skin disease
- More common in females
- Triggers
- Alcohol
- Stress
- Smoking
- Hot weather
- Clinical features
- No comedones or seborrhoea
- Erythematotelangiectatic rosacea
- Central facial erythema
- Telangiectasia
- Papulopustular rosacea
- Papules, pustules and erythema
- Phymatous rosacea
- Skin thickens
- Inflammatory nodules
- Rhinophyma – large, bulbous nose
- Ocular rosacea
- Conjunctival hyperaemia
- Blepharitis
- Dry eyes
- Keratitis
- Treatment
- Avoid triggers
- Topical
- Metronidazole
- Ivermectin
- Azelaic acid
- Oral
- Tetracycline
- Metronidazole
- Isotretinoin
- Rhinophyma – surgical treatment
11. Tuberculosis of the skin and its treatment
- Cutaneous tb is a rare form of extrapulmonary tb
- Multiple types
- Tuberculous chancre
- Occurs at the site where m. tuberculosis enters the skin
- In people who don’t already have TB
- Papule -> painless ulcer
- TB verrucosa cutis
- Occurs at the site where m. tuberculosis enters the skin
- In people who already have TB
- Purplish warty growth
- Lupus vulgaris
- Apple-jelly nodules (gelatinous consistency)
- Sharply defined reddish-brown lesions
- On head
- Scrofuloderma
- Direct extension of underlying TB from lymph nodes, bones or joints to the skin
- Firm, painless nodules -> ulcerate
- Miliary TB
- Haematogenous dissemination of m. tuberculosis
- Small (millet-sized) erythematous papules -> ulcers, abscesses
- Tuberculids
- Papulonecrotic tuberculid
- Necrotic papules
- Erythema induratum
- Hard nodules on back of legs of women
- Papulonecrotic tuberculid
- Tuberculous chancre
- Diagnosis
- Tuberculin skin test (TST) / purified protein derivative (PPD)
- Interferon gamma release assay (IGRA)
- Treatment
- RIPE for 2 months
- RI for 4 months
12. Photodermatoses and phototherapy
- Photodermatoses – skin diseases that develop due to light exposure
- Photodermatoses of unknown origin
- Solar dermatitis = sunburn
- UVB radiation causes apoptosis of keratinocytes -> release of inflammatory cytokines
- Clinical features
- Pruritus, pain
- Erythema, oedema
- Blisters (severe)
- Treatment
- Wet compress
- Cooling ointments
- Topical steroids
- Polymorphous light eruption (PLE)
- Chronic disease
- In adult females
- Most common photodermatitis
- Clinical features
- Itching, burning erythema
- Malaise, headache
- Solar urticaria
- Rare
- Type I hypersensitivity
- Urtica at site of sun exposure
- Actinic prurigo
- Chronic actinic dermatitis
- Solar dermatitis = sunburn
- Photodermatoses of known origin
- Phototoxic reactions
- Photoallergic reactions
- Diagnosis
- Photo-patch test
- UVA applied, then patch
- Read immediately, then at 24, 48, 72 hours
- Photo-provocation test
- Differentiate between solar urticaria, chronic actinic dermatitis, polymorphous light eruption, SLE
- Photo-patch test
- Treatment
- Photohardening
- Photoprotection
- Phototherapy
- Indications
- Psoriasis
- Atopic dermatitis
- Alopecia areata
- Granuloma annulare
- Cutaneous T-cell lymphoma
- Vitilligo
- Photodermatoses
- BCC
- Actinic keratosis
- Mechanisms
- Thickens epidermis
- Hyperpigmentation
- Immunosuppressive effect
- Anti-tumor effect
- Procedure
- Minimal erythematous dose (MED) is determined
- The dose of UV light depends on the MED
- Types
- Narrow-band UVB
- Broad-band UVB
- Selective UVB
- Psoralen + UVA
- Photodynamic therapy
- Uses visible light, not UV
- For cancers that are caused by UV (BCC)
- Indications
13. Lyme Borreliosis
- Tick-borne
- Borrelia burgdorferi
- Clinical features
- Stage I – early localized Lyme disease
- Within 7 – 14 days
- Erythema migrans
- Circular, slowly-expanding red ring with central clearing around the bite site
- Target-like rash
- Flu-like symptoms
- Stage II – early disseminated Lyme disease
- Multiple erythema migrans
- Migratory arthralgia
- Early neuroborreliosis
- Lyme carditis
- Stage III – late Lyme disease
- Acrodermatitis chronica atrophicans
- Inflammation and atrophy of skin of extremities
- Chronic Lyme arthritis
- Late neuroborreliosis
- Acrodermatitis chronica atrophicans
- Stage I – early localized Lyme disease
- Diagnosis – serology
- Treatment
- Doxycycline
- First-line
- Amoxicillin
- In pregnant
- Ceftriaxone
- If neuroborreliosis or Lyme carditis
- Doxycycline
14. Types of allergic skin reactions
- Type I hypersensitivity
- Skin reactions
- Angioedema
- Urticaria
- Diagnosis – prick test
- Treatment
- Antihistamines
- Epinephrine
- Skin reactions
- Type II hypersensitivity
- Not important
- Type III hypersensitivity – immune complex-mediated
- Cutaneous vasculitis
- Serum sickness
- Treatment
- Steroids
- Type IV hypersensitivity
- Type IVa – Allergic contact dermatitis
- Type IVb – Drug-related eosinophilia and systemic symptoms (DRESS)
- Type IVc – Toxic epidermal necrolysis/Stevens-Johnson syndrome
- Type IVd – Acute generalized exanthematous pustulosis (AGEP)
- Diagnosis – patch test
- Treatment
- Steroids
15. Cutaneous manifestation of diabetes mellitus
- 30% of all diabetes patients will experience skin symptoms
- Non-specific skin conditions
- Impetigo
- Candida intertrigo
- Psoriasis
- Necrotizing fasciitis
- Acanthosis nigricans
- Specific skin conditions
- Diabetic dermopathy
- Reddish, oval/round scaly patches
- Often on the shins
- Diabetic bullae
- Painless bullae
- Can be very large
- Intraepidermal bullae
- More common
- Filled with clear fluid
- Heal without scarring or atrophy
- Subepidermal bullae
- Less common
- Filled with blood
- Heal with scarring and atrophy
- Diabetic sclerosis
- In diabetes type 1
- Sclerosis of finger skin -> restricted mobility
- Foot ulcers (diabetic foot)
- Necrobiosis lipoidica diabeticorum
- Erythematous patches on lower legs
- May ulcerate and become infected
- Diabetic dermopathy
16. Primary skin lesions, basics of dermatohistopathology
- Primary skin lesions
- Flat lesions
- Macule
- A flat skin lesion < 1 cm in size with discolouration
- Patch
- A flat skin lesion > 1 cm in size with discolouration
- Macule
- Infiltrative lesions
- Papule
- An elevated palpable skin lesion < 0,5 cm in size
- Epidermal
- Plaque
- An elevated palpable skin lesion > 0,5 cm in size
- Intradermal
- Tuber
- An elevated palpable skin lesion whose infiltration involves the entire depth of the dermis
- Nodule
- A circumscribed elevated lesion > 1 cm
- In dermis and subcutis
- Tumor
- Large solid mass of tissue
- Papule
- Fluid-filled lesions
- Vesicle
- Small fluid-containing lesion
- Intraepidermal
- Bulla
- Large fluid-containing lesion
- Intraepidermal or subepidermal
- Urtica/wheal
- Transient oedema in the dermis
- Pustule
- Collection of pus in or below the epidermis
- Vesicle
- Flat lesions
- Dermatopathological terms
- Acantholysis
- Separation of epidermal cells due to dissolution of desmosomes
- E. g. in pemphigus vulgaris
- Acanthosis
- Hyperplasia of stratum spinosum
- E.g. in acanthosis nigricans
- Hypergranulosis
- Hyperplasia of stratum granulosum
- E.g. in lichen planus
- Hyperkeratosis
- Hyperplasia of stratum corneum
- E.g. in psoriasis
- Papillomatosis
- Hyperplasia and enlargement of dermal papillae
- Parakeratosis
- Keratinocytes in stratum corneum retain their nuclei
- E.g. in
- Psoriasis
- Dandruff
- Spongiosis
- Intraepidermal oedema
- E.g. in
- Atopic dermatitis
- Allergic contact dermatitis
- Acantholysis
17. Secondary skin lesions, basics of dermatohistopathology
- Secondary skin lesions
- Scales
- Detaching fragments of a thickened stratum corneum
- Dry and usually whitish
- Erosion
- Loss of epidermis
- Heal without scarring
- Excoriation
- Loss of papillary dermis
- Heals with scarring
- Fissure
- Painful, deep, linear opening of skin through the epidermis and into the dermis
- Rhagades
- Cracks or tears in the skin caused by stretching of brittle skin
- Ulcer
- Skin defect with loss of epidermis and upper papillary dermis
- Usually leave scars
- Crust
- Dried secretion
- Red-brown crust – blood
- Yellow crust – serum
- Honey-coloured crust – purulent streptococcus exudate
- Yellow-green crust – purulent staphylococcus exudate
- Scar
- Permanent fibrous lesions
- A result of the repair process
- Hypertrophic scar = keloid scar
- Atrophic scar
- Atrophy
- Thinning of epidermis and dermis
- Lichenification
- Increased thickness of epidermis
- Cobblestone-like surface
- A result of chronic rubbing or scratching
- Scales
18. Cutaneous T-cell lymphomas
- Mycosis fungoides
- CD4+ T-cell lymphoma
- Progresses slowly
- Stage I – patch stage
- Scaly, pruritic, well-demarcated patches
- Stage II – plaque stage
- Scaly, pruritic, well-demarcated plaques
- Large
- Stage III – tumor stage
- Dome-shaped purple or red nodules
- Treatment
- Topical steroids
- Topical chemo
- Phototherapy
- Biological therapy
- Systemic chemo
- Sézary syndrome
- Can develop from mycosis fungoides or de novo
- Clinical triad
- Systemic skin lesions
- Erythroderma
- Palmar and plantar hyperkeratosis
- Pruritus
- Generalized lymphadenopathy
- Atypical T-cells in blood
- Systemic skin lesions
- Treatment
- Extracorporal photopheresis
- Phototherapy
- Chemotherapy
- Adult cutaneous T-cell leukaemia/lymphoma
- HTLV-I associated
- Similar lesions to mycosis fungoides
Hi,
I would add more specific treatment for erysipelas:
Primary: Amoxicillin and clavulanic acid
Secondary: Ciprofloxacin and clindamycin
Tertiary: Ceftriaxone and metronidazole
The examiners are extremely strict on this and the other derma-notes got these mixed up.
Kind regards
Very low clinical yield, but if it’s important for the exam then I’ll add it. Thanks!
Juncional nevi: Only in epidermis
Compound nevi: Epidermis and dermis
Intradermal nevi: Only in dermis
https://www.mypathologyreport.ca/compound-nevus/
added
Has anyone shopped at The King of Vape Vapor Store located in 1656 Annapolis Road?
I’m sure someone, somewhere has shopped there, but I haven’t at least.
For the topic: “23. Acne and its treatment”
Our dermatology teacher denied several times today; that food & certain hair/facial products can exacerbate or be a risk factor for acne.
What do you say to this?
Throughout your career as a medical student and doctor you will hear many opinions and “facts” from others which contradicts with the opinion of the overall scientific community. I can’t think of any specific examples but I’ve experienced this many times. Nobody is perfect, and this includes doctors. Like everywhere else in life you must be critical of what you hear and research contradictory facts for yourself. Luckily, most of what we’re taught is correct.
There are many scientific articles which have shown a connection between certain foods and cosmetic products and acne. This article could be a good start: https://www.aad.org/public/diseases/acne/causes/diet. But I wouldn’t encourage you to start an argument with your teacher, as I’m sure nothing good will come of it.