Page created on November 18, 2018. Last updated on December 18, 2024 at 16:56
Hypersensitivity reactions in general
Sometimes can immune system reaction injure the tissues of the body. These types of immune system reactions are called hypersensitivity reactions. This occurs when the immune system is inadequately controlled, or the immune reaction might inappropriately target host tissues instead of foreign pathogens.
There are many causes of hypersensitivity reactions:
- Reaction against self-antigens
Normally does the body tolerate (not react against) self-antigens. Sometimes the self-tolerance fails, which causes the immune system to target host cells.
- Reaction against microbes
The immune system should react against microbes to get rid of them, however in some cases the immune reaction is too aggressive or the microbe is very persistent and hard to get rid of. Antibodies against microbes are usually not present in the blood for a long time, but if the microbe is persistent can the presence of high levels of antibodies actually cause harm. The antibodies can bind to the microbe antigens and form immune complexes, which can deposit in tissues and cause harm.
Persistent microbes also cause prolonged inflammation, which is what causes tissue injury in tuberculosis for example.
- Reaction against environmental antigens
Immune system reaction against environmental antigens like ragweed, grass, gluten or dust mites is what causes allergies.
Type 1 hypersensitivity
This type of hypersensitivity reaction is also called immediate hypersensitivity because it occurs very quickly (within minutes). It is the type of reaction that occurs in hay fever, seasonal rhinitis, asthma or even anaphylaxis.
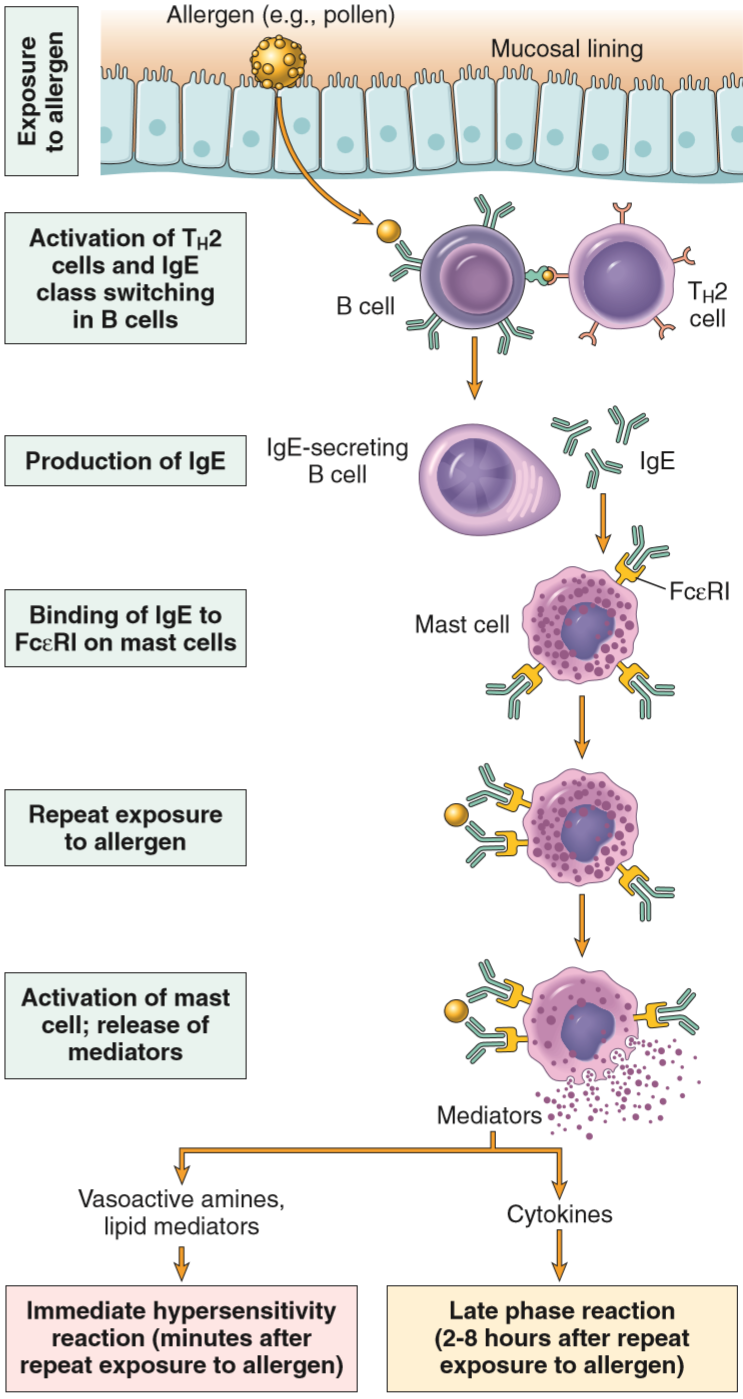
It begins when an allergen is taken up by an antigen-presenting cell, which will present it to a Th2 cell. The Th2 cell will respond by producing three interleukins, each with different functions:
- IL-4 stimulates B-cells to start isotype switching to produce IgE antibodies.
- IL-5 activates and recruits eosinophils to the site of the inflammation
- IL-13 activates epithelial cells and stimulates mucus secretion
B-cells then produce IgE antibodies against the allergen. The Fc-part (not the antigen-binding part) of these antibodies will bind to a type of Fc-receptor on the surface of mast cells called FcεRI. Now that the mast cells are covered in IgE antibodies (that point outward) do we say that the mast cells are sensitized.
When the patient with sensitized mast cells meets the allergen later will the allergen not be taken up by antigen-presenting cells but instead bind to the IgE antibodies on the surface of mast cells. This activates the mast cells, causing them to release three groups of molecules:
- Vasoactive amines like histamine. Adenosine, proteases and chemotactic factors for neutrophils and eosinophils is also released. These molecules are stored in granules inside the mast cell and the granules are released. Histamine causes vasodilation, smooth muscle contraction and increased permeability. Adenosine causes bronchoconstriction and inhibits platelet aggregation. The proteases may damage tissues.
- Arachidonic acid derivatives, like prostaglandins and leukotrienes. These molecules aren’t stored in granules but are instead produced when the activation happens. Prostaglandins cause intense bronchospasm and increases mucus production. Leukotrienes are both chemotactic for neutrophils and are very strong vasodilators and bronchoconstrictors.
- Cytokines like TNFα, IL-4, IL-5 and IL-13, which amplify the immune reaction by the mechanisms described above. TNFα activates other leukocytes.
This hypersensitivity has both immediate and late phases.
The immediate response is characterized by vasodilation, oedema and smooth muscle spasm, which appears 5-30 minutes after exposure to the antigen and ends after 60 minutes.
The late-phase response starts 2-24 hours after exposure and is characterized by inflammation and tissue destruction. Eosinophils, neutrophils, basophils, monocytes and Th2-cells are important in this reaction. Mucosal epithelial damage occurs.
Clinical manifestations of type 1 hypersensitivity range from just annoying to life-threatening. Local hypersensitivity reactions like hay fever or grass or gluten allergy, cause symptoms like urticaria, diarrhoea or running nose. Systemic reactions however can cause anaphylactic shock, which can occur in bee, peanut or penicillin allergies for example.
The tendency to have type 1 hypersensitivity reactions has a genetic component, and patients with this tendency are said to have atopy. Patients who have atopy usually develop one or more of the following: eczema, hay fever or allergic asthma. If someone has one of these conditions is the probability of also having the others high as well.
Type 2 hypersensitivity
This type of hypersensitivity, also called antibody-mediated hypersensitivity is characterized by the body producing antibodies against antigens it should normally leave alone, like host antigens or harmless exogenous antigens.
Opsonization is an important term here. Normally, when a bacterium or virus enters the body will the immune system produce antibodies against them. These antibodies will bind to and cover the pathogen. Opsonization is the term for covering something in antibodies. Complement factors like C3 can then bind to the opsonized pathogen. What happens next is that phagocytes like macrophages and neutrophils can phagocytose the pathogens by recognizing the opsonization. Phagocytes carry receptors that recognize both the complement factors and antibodies and use these receptors to bind and ingest the pathogen. Opsonized pathogens that aren’t phagocytosed will be eliminated in the spleen.
If antibodies are produced against antigens found on cells in our body will the phagocytes eat them up as well (phagocytes can’t recognize the target as a host cell, they only see whether the target has antibodies attached to them).
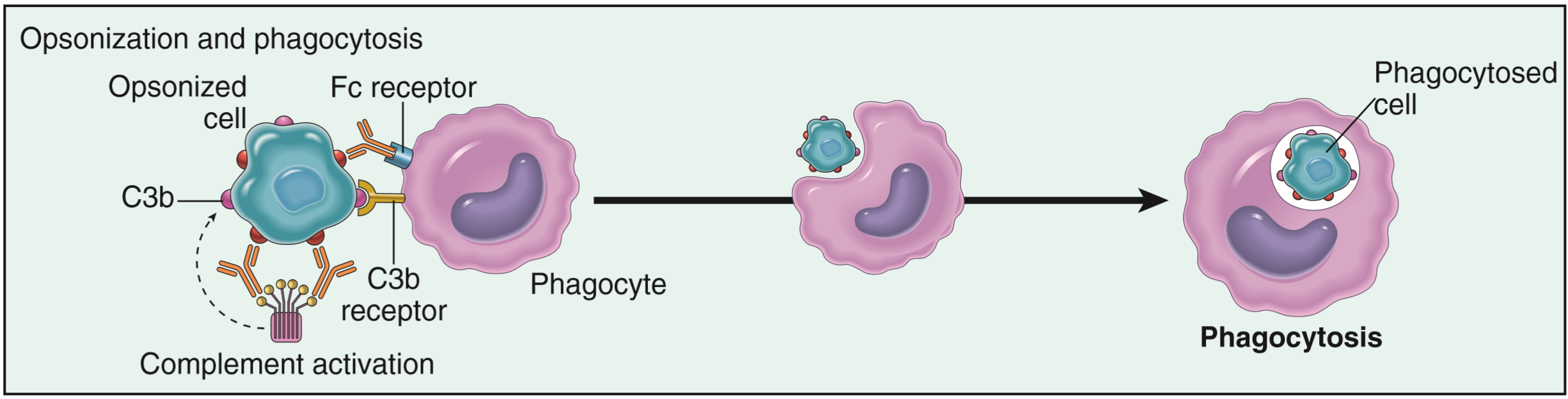
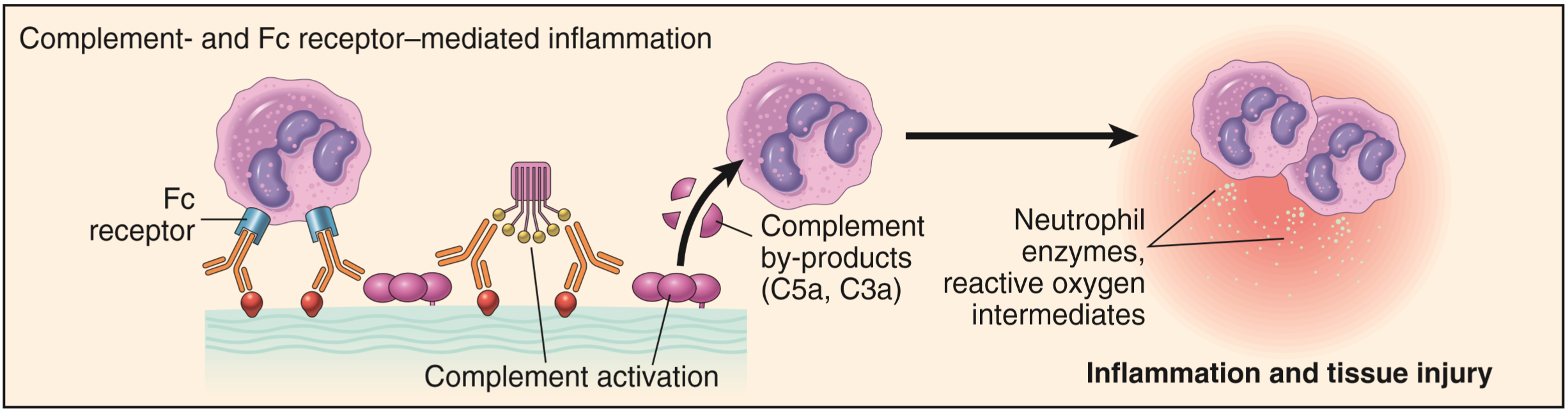
Inflammation occurs because the complement system is activated (via the classical pathway) by opsonized pathogens or cells. The complement system has many functions, and one of them is to cause inflammation. Leukocytes (that aren’t phagocytes) can also recognize the opsonized cells and cause inflammation.
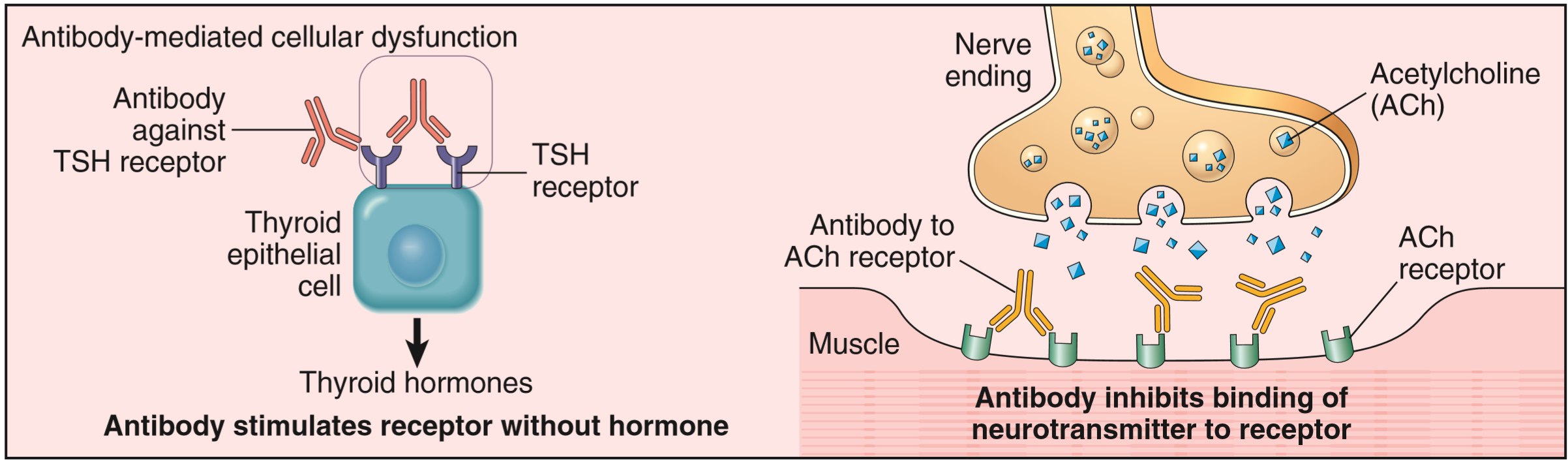
Antibodies can disrupt cell function in other ways as well, without causing phagocytosis and inflammation. As is the case in myasthenia gravis will antibodies bind to nicotinic acetylcholine receptors in neuromuscular junctions (without activating the receptor). When the acetylcholine receptors are occupied by antibodies can they not bind acetylcholine, effectively paralyzing the muscle. In Graves disease will antibodies bind to the TSH receptors found on thyroid epithelial cells, and activate the receptors (unlike in m. gravis). This tricks the thyroid to believe that the levels of TSH in the blood is very high, which stimulates the thyroid to produce more thyroid hormones, causing hyperthyroidism.
Here’s a table of important diseases caused by hypersensitivity type 2:
| Disease | Target antigen | Mechanism of disease | Clinicopathological manifestations |
| Erythroblastosis foetalis | Antigens on foetal RBCs | Maternal IgG crosses placenta, haemolyses RBCs | Anaemia in foetus |
| Autoimmune haemolytic anaemia | RBC membrane proteins | Opsonization and phagocytosis of RBCs | Haemolysis, anaemia |
| Pemphigus vulgaris | Proteins in intercellular junctions between epidermal cells | Antibodies activate proteases, destroys the junctions | Skin vesicles |
| Vasculitis caused by ANCA | Proteins inside neutrophil granules | Neutrophil degranulation and inflammation | Vasculitis |
| Acute rheumatic fever | Antibody against streptococcus also targets myocardium | Inflammation, macrophage activation | Myocarditis |
| Myasthenia gravis | Acetylcholine receptor | Antibody blocks the receptor | Muscle weakness, paralysis |
| Graves disease | TSH receptor on thyroid cells | Antibody activates the receptor | Hyperthyroidism |
| Insulin-resistant diabetes | Insulin receptor | Antibody blocks the receptor | Hyperglycaemia, ketoacidosis |
| Goodpasture syndrome | NC1 protein in glomerular basement membrane and lung alveoli | Inflammation | Nephritis, lung haemorrhage |