I had Clinical Biochemistry yesterday. I studied 3 days for it. My main examiner was Dr. Tamás Nagy. Dr. Ágnes Péterfalvi was the co-examiner. The exam takes place in the department. We showed up outside where the clinical biochemistry seminars took place.
You draw two random topics from one pile. Few examiners give you a lab result to analyze; the examiners yesterday only gave them to those who were between two grades. Even then, they didn’t have to come up with a diagnosis based on the results. It was more of a discussion of what the result tells you, what differential diagnoses can be, what the next steps in diagnosis can be, etc.
My two topics were “19. Laboratory diagnostic approaches in anemias” and “48. Tumor markers and their informational value in the clinical laboratory practice”. The subject and exam are plagued by typical POTE bullshit which I will explain more about later. There are some topics which are 0% covered in the lectures or seminars, like 27 (only like 2 slides with no useful information), 39 and 40.
19. Laboratory diagnostic approaches in anemias
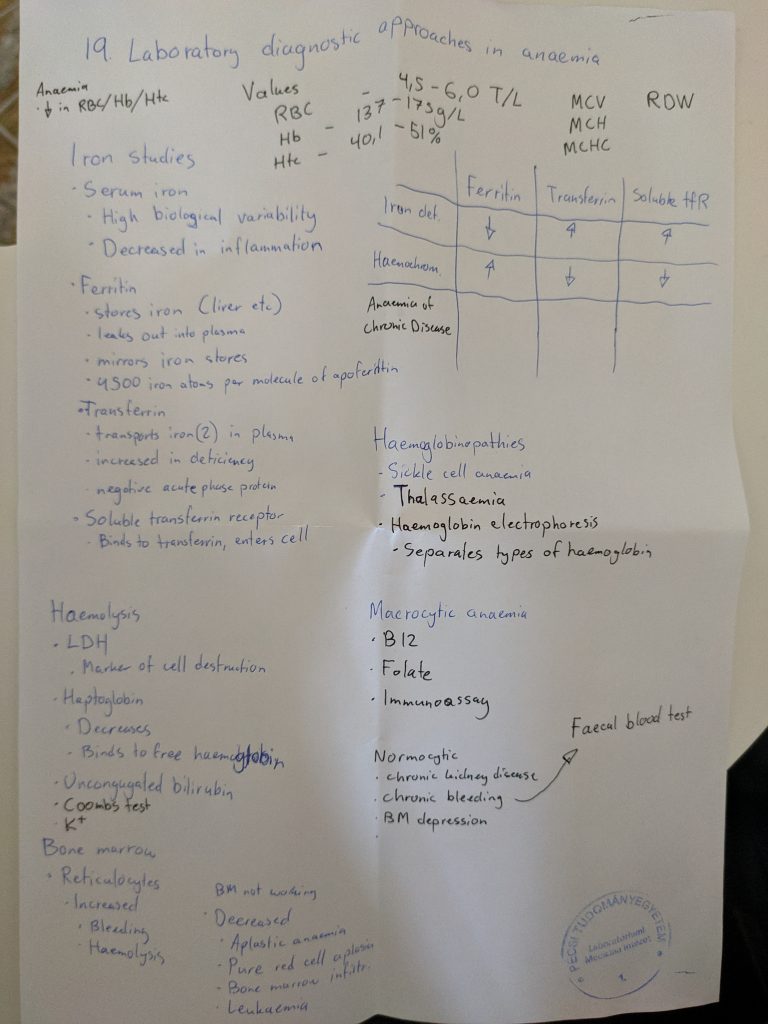
This was my best topic. I had written down almost everything which is important. I began by saying that the definition of anaemia is a reduction in RBC count, haematocrit or haemoglobin. The examiner stopped me by saying that it’s wrong, and only the haemoglobin matters for the diagnosis of anaemia. What he said isn’t correct according to uptodate or even the co-examiner’s own seminar! She was my seminar teacher and I have her powerpoints. Typical POTE bullshit.
Anyway, I go on by talking about the classification according to cell size, what the different causes of microcytic, macrocytic, normocytic etc. can be. While I’m talking about haemolytic anaemias the examiner says “I think it’s appearent that you know this. Let’s go to the next topic.” Good start!
48. Tumor markers and their informational value in the clinical laboratory practice
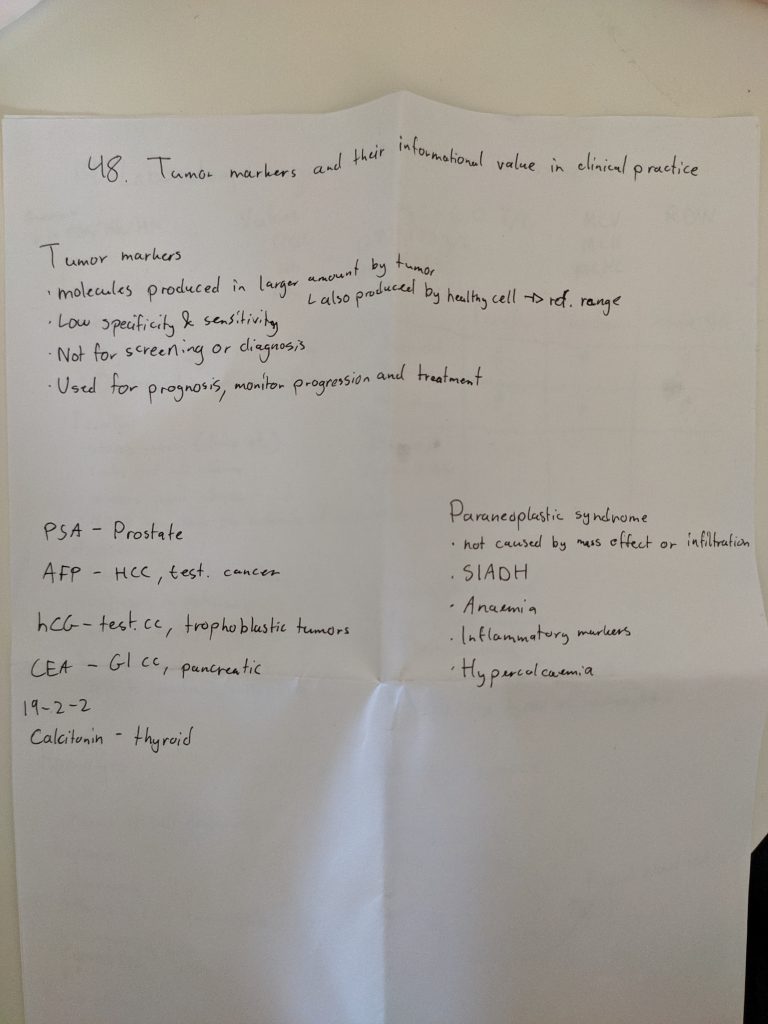
I start by explaining the definition of tumor markers. I explain that they’re often low sensitivity and specificity and therefore not useful for screening or diagnosis. I say that they’re value lies in determining prognosis, monitoring treatment response and relapse.
I mention some examples of tumor markers, the ones I had written down. There’s not much more to say (there’s wasn’t much more on the lecture). They then start to ask me many questions about stuff which wasn’t on the lecture. I don’t know the answer to many of the questions. They try to help me with the answer to each question, in some cases I can think my way to the answer but in other cases I couldn’t.
They then decide to give me 4. I immediately get a little angry inside, because I had mentioned everything they taught us about tumor markers and that somehow wasn’t enough for a 5? What?
I ask them if I can fight for a 5. They accept. They ask me some questions (more questions about stuff which wasn’t on the lecture). They also give me a lab test to evaluate. They eventually agree to give me a 5, even though I didn’t really answer many of their questions, at least not without a lot of help.
I remember some of the questions from my exam, but to be honest I can’t remember which questions were asked before they wanted to give me a 4 and which ones they asked after I asked to fight for a 5. Anyway, here they are.
- Tamás: Do you check the PSA before or after you do rectal digital examination?
- Me: After?
- T: No, you do it before. Why?
- (No idea)
- T: During rectal digital examination you might physically stimulate the tumor or benign prostate hyperplasia, which can stimulate them to release PSA, which gives a falsely elevated result.
- T: Do you know a non-cancer factor which increases CEA?
- (No idea)
- T: It’s a bad habit many people have.
- M: Alcohol?
- T: No, the other common bad habit.
- M: Smoking?
- T: Yes, smoking can elevate CEA and cause a false positive result.
- T: PSA can be elevated in both BPH and prostate cancer. What can the laboratory do to make the PSA measurement be more specific for cancer?
- (No idea)
- Turns out you can measure “free” PSA, and the free PSA is more specific for cancer. Lower free PSA means increased risk for cancer.
They gave me a lab test. The test includes reference ranges and exclamation marks at the tests which are outside the refence. The lab I saw had elevated CEA and CA 19-9, cholesterol, uric acid and a positive stool blood result.
- T: What can this be?
- M: Probably GI cancer, it explains the blood in the stool, and the tumor markers are often elevated in GI cancers. High cholesterol can also be a sign of bad diet, which is a risk factor for these cancers.
- T: What can explain the elevated uric acid?
- M: Maybe this test was taken after chemotherapy and it’s due to tumor lysis syndrome.
- T: Yes, most likely.
They also asked me about K-RAS, what it is and why it’s important. I said it’s a proto-oncogene which can be mutated in GI cancers. They agreed and asked what the importance of it is. With some help I arrived at the conclusion that K-RAS can be tested for in cancers, and its mutations influences the prognosis and treatment of the patient.
Other than the typical POTE bullshit they were very nice. It was almost impossible to fail with them, so I wouldn’t worry about failing clinical biochem. I studied the lectures and seminars, and even though they appearently don’t contain all the information they expect us to know, it should be more than enough to pass. They also ask basic stuff from patho and pathophys, nothing difficult.
My next exam is public health on thursday. I was originally planning to do derma on friday, but I realized I’m way too tired to do that, so I changed it to public health instead.