So I had obgyn final on the 18th and psych final on the 19th.
Obstetrics and gynaecology final
We got an e-mail the day before that the exam would start at 9. The examiner was Péter Gőcze. We drew four topics, two from ob and two from gyn, and sat down to prepare. I drew good topics, in my opinion. These are the questions I was asked.
10. Placenta praevia
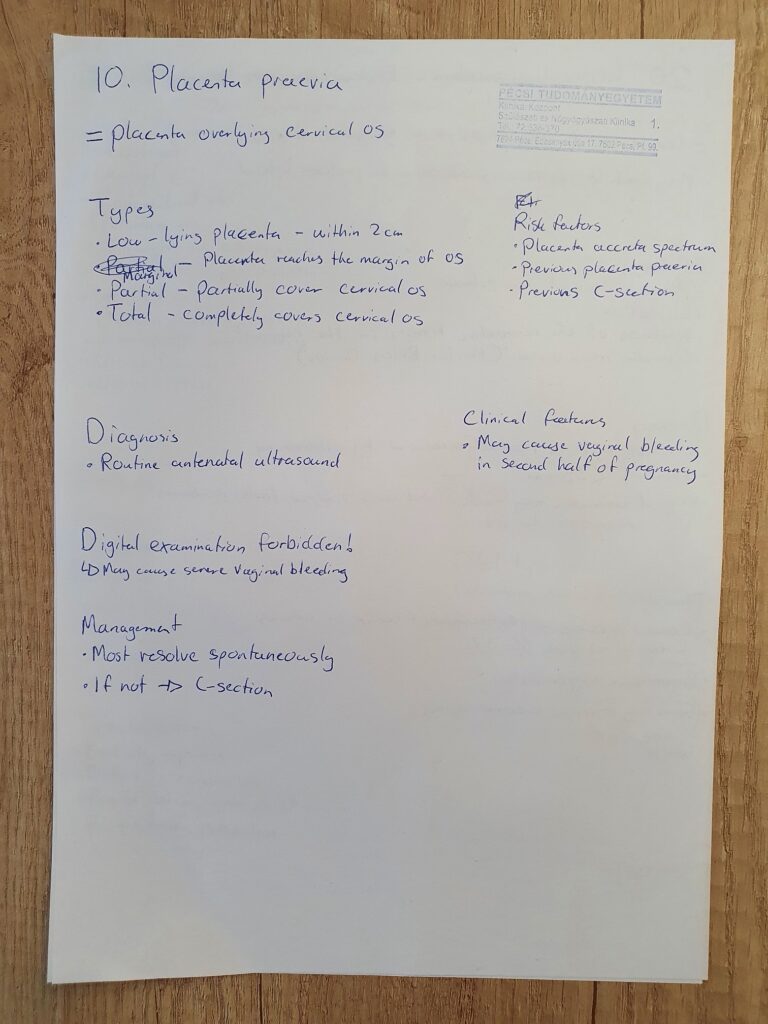
I began by telling him everything I’d written down. He then begins asking questions.
- Examiner: When a patient arrives outpatient clinic with a bleeding in the second half of pregnancy, not a heavy bleeding, and you perform ultrasound and diagnose placenta praevia centralis. The patient is around 30 weeks of gestation. What can you do?
- Me: 🤷♂️ (What can you do? There isn’t really anything we can do to treat placenta praevia, right?)
- M: I think we would just call the patient back later to see if it resolves spontaneously, but if it doesn’t, we should plan an elective C-section.
- E: But the bleeding is not severe (I feel like I didn’t really understand what I said here). What can we do?
- M: I stop and think for a moment because I have no idea. I go with a far-fetched idea.
- M: Maybe we could give tranexamic acid to decrease the bleeding?
- E: No, no. Something else. Sometimes contractions can cause bleeding. (What?)
- M: Then maybe we can give something to decrease contractions, like atosiban?
- E: That’s right. Let’s say the woman is 29 weeks of gestation, what can you give to prevent the very common problem of premature newborns?
- M: Steroids to induce lung maturation.
- E: That’s right. And also, you have to store blood in the institute which is compatible with the mother, because if the patient has heavy bleeding you have to perform an urgent operation, and may need transfusion. It’s very important to have blood available.
- (It makes sense, I just thought that that was something which was always available, not that you’d have to proactively find and store it)
- E: What do you think, what is the relatively common problem if the patient has a heavy bleeding?
- M: So if the bleeding is severe enough it can compromise the circulation of the foetus as well, causing perinatal asphyxia.
- E: Yeah, and?
- M: It can also cause DIC in the mother.
- E: That’s right. What can you do in case of the DIC?
- M: It’s important to replace the clotting factors which are lost.
- E: How can you do that?
- M: It’s also a transfusion (I forgot exactly which blood product we use)
- E: Yeah but which?
- M: (I say the first that comes to mind) Prothrombin complex?
- E: No.
- M: Fresh frozen plasma?
- E: Yes. Previously a lot of women died because of this. The problem is that we don’t know which phase DIC is in, and this is why the best way is to use fresh frozen plasma because it contains all types of factors. And blood. Fresh frozen plasma and blood, this is the best method to treat DIC.
- E: Okay. What is your next topic?
20. Cervical incompetence; Etiology, diagnosis, therapy
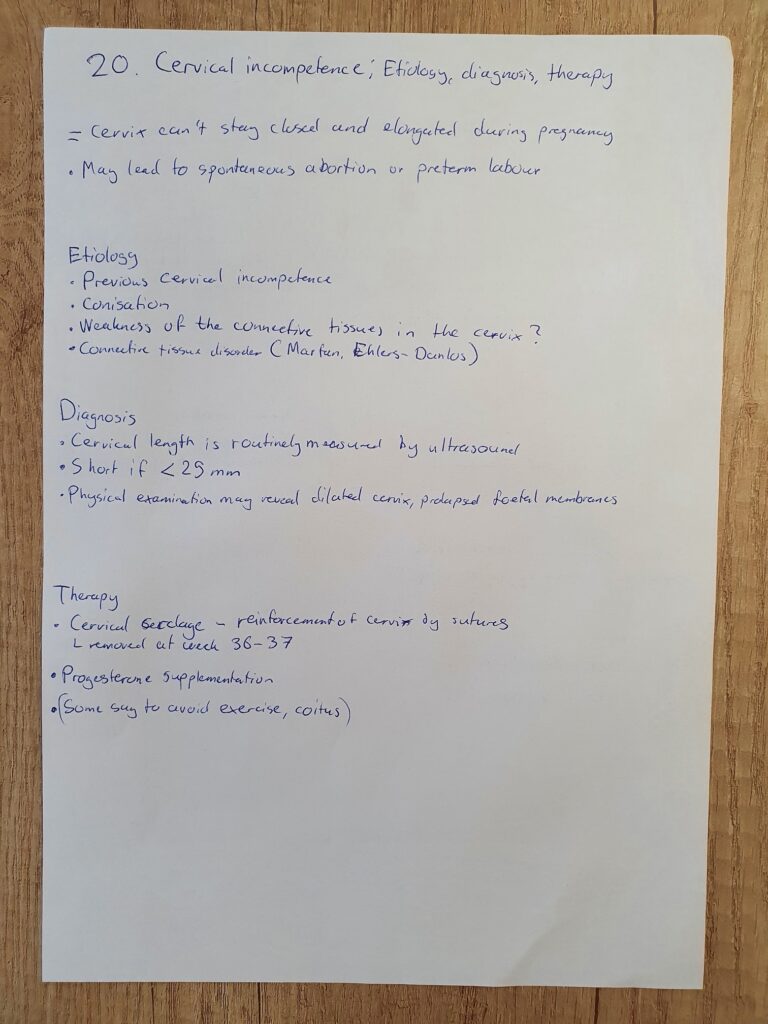
Once again I begin by telling him what I’d written down.
- E: What is very important to do before performing cerclage? What must we always do?
- M: Once again I have no idea
- M: We should supplement progesterone? Said in a tone of absolute doubt
- E: No.
- M: Thinking
- E: If we don’t do it, we can get premature rupture of the membranes
- M: So we have to rule out infection?
- E: That’s right. It’s obligatory to make a culture. Only if the culture is sterile can we do a cervical cerclage.
- E: What kind of other procedure can you do to treat cervical incompetence before pregnancy?
- M: I’m pretty sure I’ve never heard of any such procedure. The only other thing I’ve read about which can treat cervical incompetence is progesterone supplement, so..
- M: You can give progesterone supplement?
- E: No, not that. There’s a surgical procedure which you can do.
- He turns toward the other students in the room and asks them whether they’ve heard about it. No one responds. Eventually he gets up, walks toward a whiteboard in the room, and starts drawing and explaining.
- E: So you cut out a piece of the anterior wall of the cervix, then you suture it. This forms a scar. It’s usually the anterior part of the cervix which is weak, and this strengthens it. It’s very effective but you can only do it before the pregnancy. During the pregnancy, the only option is cerclage, like you mentioned.
- E: Okay. What is your next question?
3. Indications and methods of hysterectomy
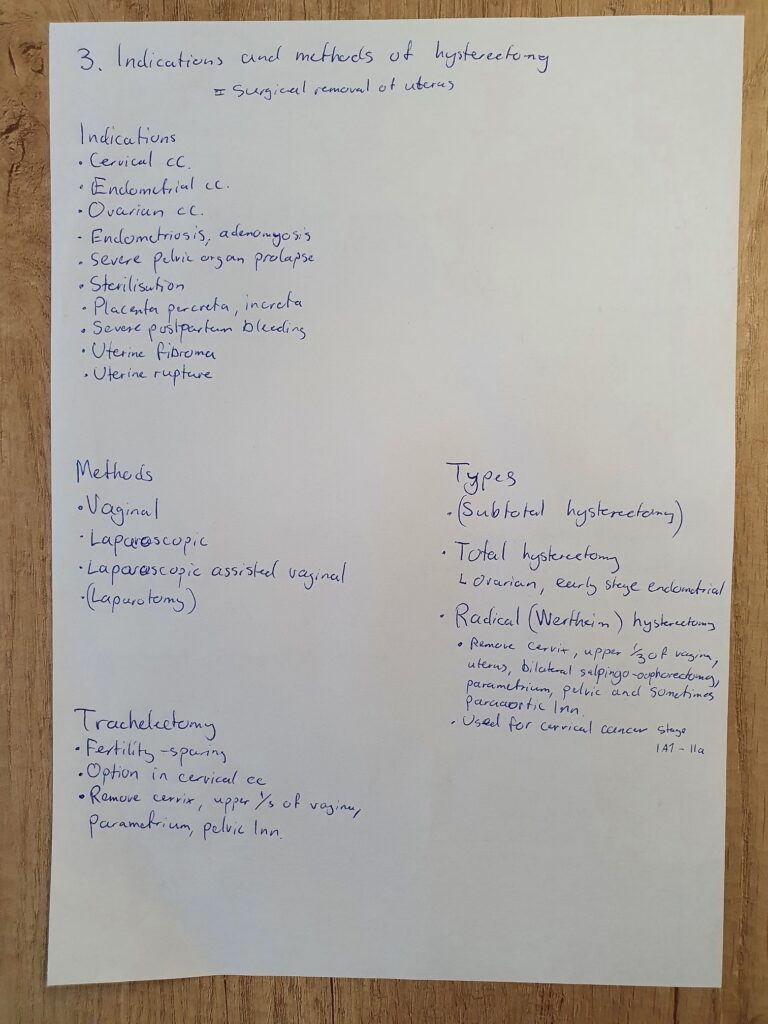
Once again I begin by telling him what I’d written down (except the part about trachelectomy).
- E: Do we always have to remove the cervix, or not?
- M: Uhm…
- E: Consider a young woman. You should know that after a total hysterectomy the vaginal prolapse can happen because of damage to the ligaments holding the vagina. And this is why we in young women often use the Chrobak operation. Have you heard about it?
- M: No I have not.
- Once again he asks the other students. No one responds.
- E: Yeah, it’s when the cervix remains in place and we just remove the body of the uterus. It can be useful because the sexual function of the woman remains normal and prolapse of the vagina can be prevented.
- Okay, so it’s just subtotal hysterectomy. Thanks for not just saying that.
- E: Okay. Next question.
13. The criteria and potential complications of IUD
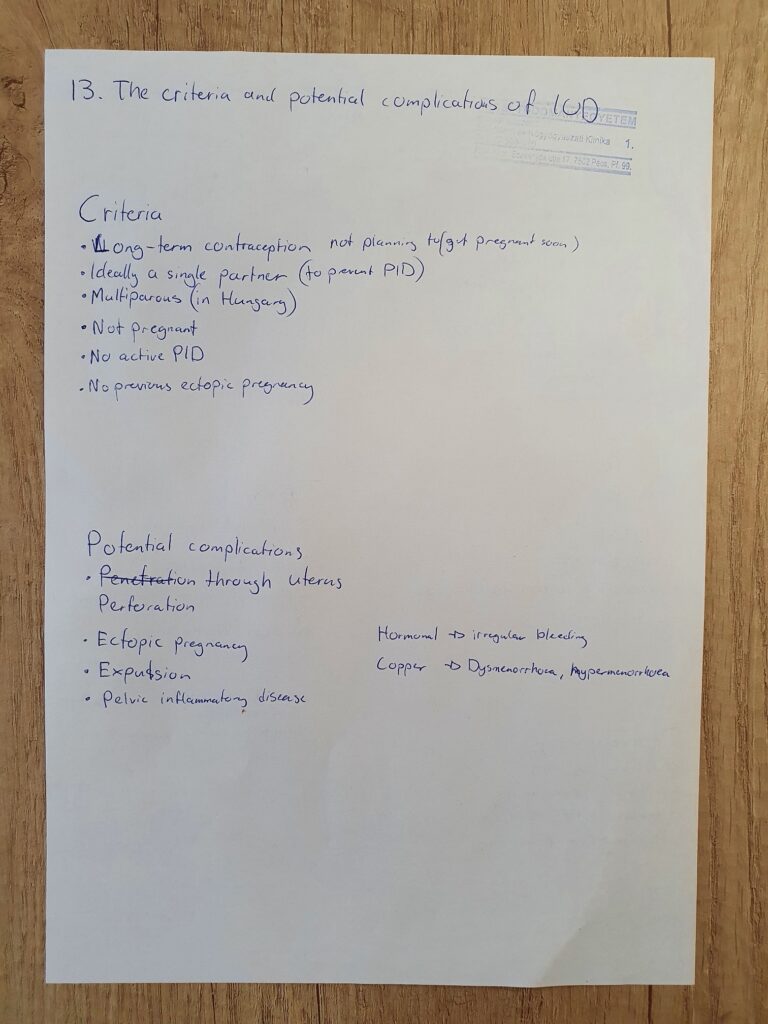
I kept this for last because I didn’t actually know that many criteria and complications. I told him what I’d written down.
- E: Do you know the name of the IUD which contains progestins?
- M: Well I know the name of those used in Norway, but I don’t know if they have the same name in Hungary. Mirena and Kyleena?
- E: That’s right. What’s the indication of the Mirena? Why is it so popular? We can use not just for contraception, after all.
- M: For endometriosis as well.
- E: Yes, very good. And?
- Here I kind of blank out. I knew of other indications for hormonal IUD but I just couldn’t recall any
- E: Endometrial hyperplasia, for example. During menopause, as the progestin component. And dysmenorrhoea.
- M: Yeah, of course.
- E: Okay. I think it was good, but not excellent.
Finishing thoughts
So that was it. I got a 4 in the end. The exam took like 20 minutes.
I don’t think he mentioned the name of the pre-pregnancy operation for cervical incompetence, and I’ve searched for it but found nothing. We never had a lecture or seminar on cervical incompetence, so how would I know about this?
According to a helpful commenter, this is apparently “isthmorrhaphy“, which, from what I can find, is not exactly popular.
Regarding the “Chrobak operation”, from what I can find it looks like this term is almost never used (subtotal hysterectomy instead). Also, we never had a lecture or seminar on this topic either.
Regarding screening patients for infection before cerclage, this appears to be controversial, and UpToDate states that there is insufficient evidence to support that preprocedure culture improves outcomes.
So I’ve spent a lot of time and resources writing notes for this. I’ve used many sources, including lectures, UpToDate, and the Norwegian guidelines for obstetrics and gynaecology. When I spend so much time and effort studying something, and end up not being able to answer questions on the exam because certain things were never taught to us, is basically unfindable in other sources, or not evidence-based, it makes me disappointed and annoyed. But anyway, I’m glad I’m done.
Psychiatry final
We got the email from Tényi the day before the exam that we would start at 7:00. We show up, both 6th year students and 5th year students from all three programmes. Luckily, he deliberately allowed the 6th year students to have the exam first.
There’s not to much to say about the exam. During the practice you write two patient case reports. In the exam he asked me what the two diagnoses were (schizophrenia and anorexia nervosa), and he asked me to explain a bit about the anorexia case, which I did. I realise in hindsight that I spoke mostly about my impressions around the case rather than stuff directly related to psychiatry, but it was fine. He then started asking the usual rapid-fire questions, beginning with questions related to anorexia and eating disorders, before turning to other questions.
I answered all questions correctly, except that I forgot narcissistic personality disorder when listing the cluster B ones, but it was fine. I got a 5 in the end, and the exam took like maybe 5 – 10 minutes? It was a nice experience.
Next up
I begin my paediatrics practice in Pécs on Monday, which will be my only practice in Pécs (except for 1 week of internal medicince, as I could only do 7 weeks in Norway). Paeds is my next exam, but luckily that’s some weeks away still, so I can take it easier for a while.
Hi, I wanted to know where is the location of OBGYN exam ? I’m in 5th year currently, is it in the white building first floor where the seminars were held ? (Or on the left side of the white building in the wards somewhere?) Help regarding where exactly I need to go would be appreciated, thanks
It’s in the building where there is a big lecture hall in the middle and the obgyn seminars are, yes. They usually pick up the students from the entrance, but the exam is in a room on the first floor. I forget which direction.
I think the procedure you guys are looking for is called “isthmorrhaphy”. You won’t find alot about it on the internet. We learned it in german program from the old professor, who is not up-to-date anymore.
Best greetings
Thank you so much!! This has annoyed me for so long.
Regarding ”Chrobak operation”, I am not the best student when it comes to attendance. However, one of the few seminars I attended ,OBGYN Johnny Sins talked about it in the Prolapse topic. He didn’t exactly mention the name but only the benefits.
For the record, I had the cervical incompetence topic on my final exam last week. When mentioning this pre-pregnancy anterior resection thingy she bluntly stated that “I’ve never even heard about that. The only surgical intervention we do in cervical incompetence is cerclage”. So yeah.. typical pote bull
Hello!
Congrats 🙂
¨Q: Which rotational-year-subjects would you recommend to do in Pecs vs in our home-country? From both experience or what you have heard from previous students.
Thank you!
It’s difficult to say. I only have one practice in Pécs, and it’s very low quality compared to those I had in Norway. However, no one cares whether you show up or not, or whether you leave early, so you have that option, which will provide you with much more personal time and time for studying. That’s not always the case for practices done in other countries, and studying after 6 – 8+ hours of proper practice can be tiring.
In general, the practical education during 4th and 5th are so bad that I feel like it’s really beneficial to have good practices in 6th to make up for it. Ideally, you’d have all practices somewhere you actually learn something. Personally, I think it’s important to know your way around internal medicine, surgery, and gynaecology from a practical standpoint, as you’ll learn stuff which is ubiquitously useful there. Of course, knowing psychiatry and neurology is also important, but maybe less so. Paediatrics and emergency medicine are probably the practices which I consider the “least” important to be good in in general, but if you’re going to be a GP, paediatrics might be very useful. So it really depends on you. But “proper” 6th year practices (abroad) can be very tiring, especially considering the travelling back and forth. I wasn’t prepared for that, but maybe you can be.
Congratssss
R u gonna write Peds note ?
Thank you.
No, I won’t unfortunately
🤬🤬🤬 I’m crying
Stop crying