Table of Contents
Page created on December 17, 2018. Last updated on December 18, 2024 at 16:56
Metabolic alkalosis
In metabolic alkalosis we have:
- pH above 7.45
- Elevated standard (and actual) serum bicarbonate
- Often a compensatory increase in pCO2
- Increased buffer base
- Positive base excess
Because it is a metabolic condition is the primary cause an increase in standard bicarbonate. This increases the 20:1 ratio. The lungs will start to retain more CO2, which increases the ratio toward 20:1 again.
It typically occurs because of loss of H+ ions but can also occur because of an increase in bicarbonate levels. If H+ is lost will this equilibrium be pushed toward the right:
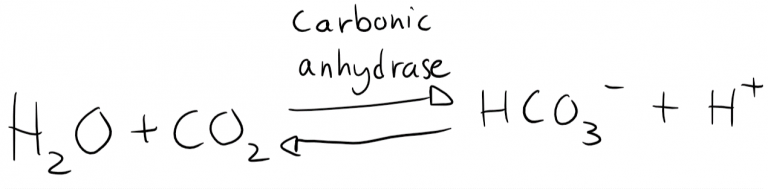
Pushing it to the right causes more HCO3– to be produced.
We can divide metabolic alkalosis into two types: chloride-responsive alkalosis and chloride-resistant alkalosis.
Chloride-responsive alkalosis
Chloride-responsive alkalosis always involves a loss of chloride (Cl–) and often involves hypovolaemia. The reason chloride is important in alkalosis is because chloride is exchanged for bicarbonate in the tubules. If chloride levels are low in the plasma will it be low in the filtrate as well. Because bicarbonate and chloride are exchanged in the tubules does this mean that the tubules can’t excrete as much bicarbonate, causing bicarbonate levels in the serum to rise.
It’s chloride-responsive because treatment with sodium chloride or potassium chloride solution will normalize chloride levels, which enables the kidney to excrete more bicarbonate.
Common causes are:
- Excessive vomiting
- Nasogastric suction tube
- Extracellular fluid volume contraction
- Congenital chloride diarrhoea
- Loop diuretics that inhibit chloride reabsorption
- Cystic fibrosis
Vomiting and nasogastric suction depletes the body of hydrochloric acid (HCl), meaning that the body loses both H+ and Cl–.
Extracellular fluid volume contraction means a loss of extracellular fluid that contains little bicarbonate and a lot of chloride. Because a lot of water is lost, but very little bicarbonate is lost will the bicarbonate concentration in the remaining extracellular fluid go up, causing alkalosis. This can occur in congenital chloride diarrhoea, a rare condition where chloride-containing diarrhoea occurs. It also occurs in administration of loop diuretics, where the urine contains a lot of chloride and water and very little bicarbonate.
Cystic fibrosis is a condition where a lot of chloride is lost while sweating.
Chloride-resistant alkalosis
In chloride-resistant alkalosis is there no extra loss of chloride, so chloride is normal. It’s associated with normovolaemia or hypervolaemia, depending on the cause.
Common causes are:
- Hyperaldosteronism
- Congenital adrenal hyperplasia (11-hydroxylase deficiency)
- Hypokalaemia
- Apparent mineralocorticoid excess (11β-hydroxysteroid dehydrogenase deficiency)
- Bicarbonate or antacid intake
Aldosterone stimulates H+ excretion, so any increased aldosterone activity will cause alkalosis. In Conn syndrome is more aldosterone produced. A Wilms tumor, a kidney tumor, may produce renin and therefore activate RAAS. Secondary hyperaldosteronism occurs when RAAS is activated due to hypovolaemia, often due to oedema.
11-hydroxylase deficiency is a form of Congenital adrenal hyperplasia where deoxycorticosterone DOC accumulates, which in high numbers can activate mineralcorticoid receptors mimicking aldosterone.
The serum potassium level is very interconnected with the H+ level, because cells exchange K+ for H+ and visa versa. When potassium in the serum is low will H+ enter the cell while K+ will leave it. This normalizes the potassium level slightly but decreases the H+ level, causing alkalosis.
Apparent mineralocorticoid excess syndrome is a condition where the enzyme 11β-hydroxysteroid dehydrogenase is deficient. This enzyme usually breaks down cortisol in the kidney to cortisone, which is less active. When the enzyme is deficient will this breakdown not occur, causing cortisol levels in the kidneys to be higher. Recall that cortisol can activate mineralocorticoid receptors. This makes cortisol have aldosterone-like effects on the kidney, causing H+ excretion.
Bicarbonate or antacid intake, often used to treat stomach ulcers, causes H+ levels to drop and bicarbonate levels to rise, causing metabolic alkalosis.
Consequences
- Hypokalaemia, due to the relationship between H+ and K+
- Hypocalcaemia. Plasma proteins will bind more free ionized Ca2+, meaning that the free Ca2+ levels in the serum decreases. This enhances neuromuscular excitability, potentially causing tetany. Tetanic spasm of the laryngeal muscles is especially dangerous as it would prevent breathing.
- The haemoglobin-oxygenation curve is shifted toward the left, meaning that the tissues receive less oxygen.
Compensation
For every 1 mmol/L increase in HCO3– will there be a 0.5 – 0.7 mmHg increase in pCO2. However, as noted before is the respiratory compensation in alkalosis limited, because a too large decrease in ventilation will cause hypoxia.
Treatment
When pH rises above 7.5 must the following be administered:
- NH4Cl
- Acids
- Potassium if necessary
- Aldosterone antagonists if appropriate
“11-hydroxylase deficiency is a form of Congenital adrenal hyperplasia where DOC accumulates”
What is a DOC?
Updated now (it’s not important tho)