Table of Contents
Page created on March 21, 2019. Last updated on December 18, 2024 at 16:57
Introduction
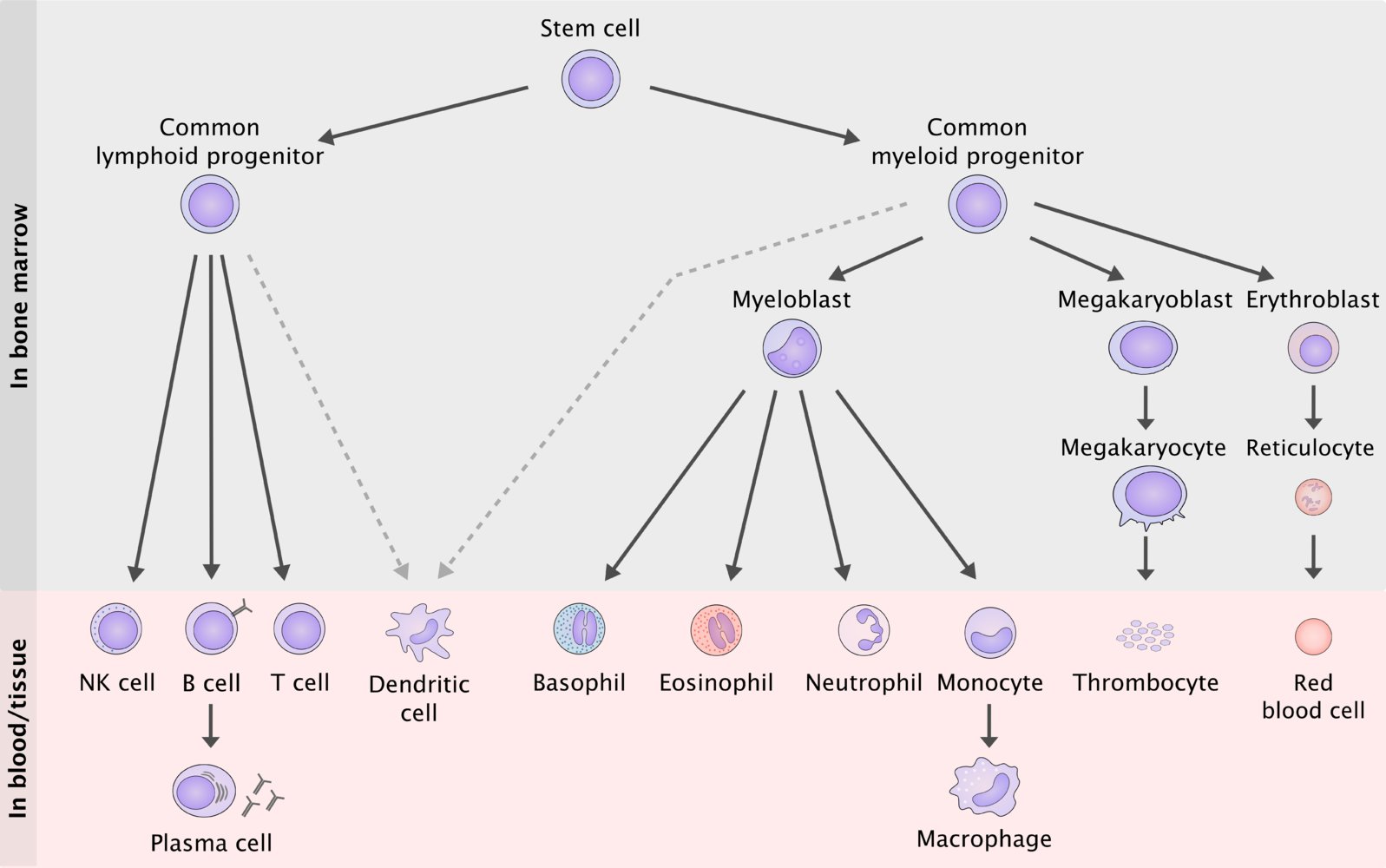
The myeloproliferative neoplasms (MPNs) are a group of disorders characterized by increased proliferation of neoplastic haematopoietic stem cells of the myeloid cell lineage. The excessive proliferation causes high blood counts of different blood cells. The neoplastic cells tend to seed to secondary haematopoietic organs like the spleen, liver and lymph nodes.
The classic MPNs are:
- Chronic myeloid leukaemia
- Polycythaemia vera
- Primary myelofibrosis
- Essential thrombocythaemia
The main difference between CML and the other classic MPNs is that the BCR-ABL1 (Philadelphia chromosome) translocation only occurs in CML. The others are associated with mutations in JAK2 or other genes.
All MPNs can progress into acute myeloid leukaemia or secondary myelofibrosis leading to bone marrow failure.
Chronic myeloid leukaemia
Introduction and epidemiology
Chronic myeloid leukaemia (CML) is a myeloproliferative neoplasm characterised by proliferation of the granulocyte lineage. It’s also characterised by the BCR-ABL1 translocation, also known as the Philadelphia chromosome.
It most frequently affects elderly.
The clinical picture involves non-specific symptoms like fatigue, weakness and weight loss. Extreme leukocytosis, even above 100 000/µL can occur, which is more than 20 times the normal value. Thrombocytosis and anaemia may also occur. Splenomegaly, sometimes extreme, is characteristic.
Pathology
CML has three phases:
- Chronic phase – slow proliferation of myeloid cells, often asymptomatic, may have B symptoms and splenomegaly, may last for years
- Accelerated phase – rapid proliferation of myeloid cells, causes extreme splenomegaly
- Blast crisis – end-stage of CML, at this stage it behaves similarly as acute leukaemia
Virtually all cases of chronic myeloid leukaemia are due to an acquired reciprocal translocation between chromosome 9 and 22 which fuses the BCR and ABL1 genes, forming a BCR-ABL1 protein. This is also called the Philadelphia chromosome, and the translocation is written as t(9;22). The BCR-ABL1 fusion protein is a non-receptor tyrosine kinase that is constitutively active, which mimics the effects of continuous growth factor receptor activation. This translocation increases the survival and proliferation of the cells without inhibiting their differentiation.
Nowadays there exists drugs that inhibit the BCR-ABL1 protein. These drugs have dramatically improved the prognosis of CML.
Polycythaemia vera
Introduction and epidemiology
Polycythaemia vera (PV) is an MPN characterised by trilinear proliferation, i.e. growth of erythroid, granulocytic, and megakaryocytic cell lines, causing elevation of all three types of blood cells in the blood.
Pathology
The erythrocytosis causes haemoglobin and haematocrit levels to be elevated compared to normal, sometimes to significant levels. There is mild leukocytosis and thrombocytosis. The erythrocytosis causes the blood to become more viscous. Hyperviscocity increases the risk for thrombosis and vascular stasis. The increased RBC count causes splenomegaly. The serum level of EPO is low and can be used to differentiate PV from other causes of polycythaemia.
It’s caused by an acquired gain-of-function mutation in the JAK2 gene which makes myeloid cells proliferate independently of stimulation by the hormone EPO.
Primary myelofibrosis
Introduction and epidemiology
Primary myelofibrosis (PMF), previously known as osteomyelofibrosis, is a myeloproliferative neoplasm characterised by proliferation of granulocyte and megakaryocyte lineages, as well as eventual deposition of fibrous connective tissue in the bone marrow.
PMF has two phases. In the prefibrotic phase, the bone marrow is hypercellular, while in the fibrotic phase, the bone marrow undergoes fibrosis.
Pathology
Fibroblasts in the bone marrow are not neoplastic but are stimulated by growth factors secreted from neoplastic megakaryocytes. Mutations of JAK2 (50% of cases) or other driver mutations are involved in the pathogenesis. The neoplastic megakaryocytes produce more thrombocytes than normal and therefore cause thrombocytosis.
Following myelofibrosis, extramedullar haematopoiesis occurs.
Essential thrombocythaemia
Introduction and epidemiology
Essential thrombocythaemia (ET) is a myeloproliferative neoplasm characterised by proliferation of the megakaryocyte lineage only.
Pathology
Mutations of JAK2 (50% of cases) or other driver mutations are involved in the pathogenesis. The neoplastic megakaryocytes produce more thrombocytes than normal and therefore cause thrombocytosis.
Histiocytic neoplasms
These neoplasms don’t have their own topic and are therefore just mentioned here.
Histiocytic neoplasms originate from dendritic cells or macrophages. They’re very rare and therefore not important to know any details of. The most common type is Langerhans cell histiocytosis.