Table of Contents
Page created on November 15, 2019. Last updated on December 18, 2024 at 16:57
Personalized medicine
When studying the effect of a drug, we do it on populations with many hundred or thousand people. These clinical trials measure the average effect of the drug on many people. These trials don’t take into account the individual response of the drug. This is a problem, because while we study drug effects on large populations, physicians use the drugs to treat individual patients.
The same drug given in the same dose doesn’t necessarily produce the same response in different patients. There is substantial interindividual variation in pharmacodynamics and pharmacokinetics of a drug. Pharmacokinetic variation means the interindividual variation in absorption, distribution, metabolism or excretion of the drug. Pharmacodynamic variation means the interindividual variation in drug response, due to differences in the drug target or signalling pathways, for example.
Personalized medicine is a concept which involves individualizing drug therapy based on the genomic information of the patient. In theory it should be possible to use the patient’s genomic information to determine which drug should be chosen, which dose should be chosen and at which time the dose should be given. In reality, we’re not quite there yet. However, even today we can use some genetic tests to predict the drug response and tailor the drug treatment to the individual patient.
Interindividual drug response variation can sometimes cause serious problems. A major point of personalized medicine is to find the drug regimen which is most efficacious, but it is perhaps even more important is to find a drug regimen which doesn’t cause adverse effects in the patient. We’ll see some examples of how interindividual drug response can cause potentially deadly problems.
Not only genetic factors but lifestyle factors can influence drug response. Age, gender, diet and lifestyle can affect both pharmacodynamics and pharmacokinetics of a drug. The presence of diseases in the patient and any concomitant drug treatments can also alter the drug response.
Pharmacogenetics vs pharmacogenomics:
Pharmacogenetics is the study of interindividual drug response variations which are due to a few genes, usually only one or two. Variations in genes for proteins like transport proteins and metabolic enzymes can cause relatively predictable variations in drug response. For example, a person can have a mutant CYP2C9 which has reduced function compared to the wildtype. This can cause warfarin to have a larger effect, which can cause potentially deadly haemorrhage.
Pharmacogenomics is the study of variations due to differences in not just a few genes but rather the whole genome. While many people may have the same mutation in one gene, no two persons have the same genome. These interactions are very complex and can be difficult to study and to even apply to drug treatments.
Possible pharmacokinetic alterations:
Each of the enzymes which metabolize drugs can have mutations. These mutations can reduce or increase the speed of the metabolism. The effect of these mutations depends on whether the drug itself is active, or an inactive prodrug.
|
Metabolizer phenotype |
Drug type | |
|
Active drug |
Inactive prodrug |
|
| Absent function | No elimination
Significant risk for toxicity |
No activation No effect |
|
Poor/slow metabolizer |
Reduced elimination
Increased risk for toxicity |
Decreased activation
Decreased effect |
| Intermediate metabolizer | Increased risk for interactions
Possible increased risk for toxicity |
Increased risk for interactions Possible decreased effect |
|
Normal metabolizer |
Drug toxicity and effect are as expected | |
| Rapid/ultra-rapid metabolizer | Increased elimination
Reduced effect |
Increased activation Increased risk for toxicity |
Pharmacogenetics of CYP450 enzymes
Of the CYP450 enzymes only three isoenzymes have considerable genetic polymorphism: CYP2C9, CYP2C19 and CYP2D6. For the other isoenzymes there’s no significant variation in function in the population.
|
Gene |
Possible mutations | Substrates |
| CYP2C9 | Slow metabolizer |
Warfarin, losartan, phenytoin |
|
CYP2C19 |
Absent function | Ritonavir, nelfinavir, cyclophosphamide, proguanil, clopidogrel |
| CYP2D6 | Rapid metabolizer, slow metabolizer, absent function |
Codeine, tramadol, propranolol, clozapine, haloperidol, fluoxetine, amitriptyline |
Warfarin:
The therapeutic window of warfarin is very narrow, which is why routine control of the INR is necessary. Warfarin is metabolized by CYP2C9, and its pharmacodynamics depend on VKORC1. VKORC1 is the gene for Vitamin K epoxide reductase complex subunit 1, which is the protein warfarin inhibits to cause anticoagulation. Polymorphisms of VKORC1 exist which decreases its effect.
The effect of warfarin is dependant on polymorphisms of both CYP2C9 and VKORC1. For the wildtype CYP2C9 metabolizers with normal VKORC1 function the daily dose is approx. 6mg. For the slowest CYP2C9 metabolizers with reduced VKORC1 function the daily dose is approx. 1,5 mg, which is substantially lower.
Genetic testing of CYP2C9 and VKORC1 are required by FDA (according to the lecture. I can’t find anywhere else that the FDA requires it).
Clopidogrel:
Clopidogrel is a commonly used antiplatelet drug. It’s often prescribed to those who have or have had coronary artery disease. It’s a prodrug which is activated by CYP2C19. People with absent CYP2C19 function have significantly lower levels of the active metabolite of clopidogrel, and as a result they have much higher risk of major cardiovascular events, including thrombosis.
The FDA recommends genetic testing of CYP2C19 (once again, according to the lecture. I can’t find this recommendation).
Codeine and tramadol:
Codeine and tramadol a opioid prodrugs which are metabolized into active metabolites by CYP2D6. People with reduced CYP2D6 activity will have decreased analgesic effect. Rapid CYP2D6 metabolizers are at risk for opioid overdose due to toxic systemic concentrations of the active metabolite.
SSRIs and SNRIs:
The SSRIs and SNRIs are the most prescribed antidepressants. Only about half of people who take antidepressants will respond, and 55% experience at least one bothersome adverse effect. Many SSRIs and other antidepressants are metabolized by CYP450 enzymes. The most important is CYP2D6, which metabolizes paroxetine, fluoxetine, venlafaxine and all tricyclic antidepressants. Polymorphisms in the serotonin transporter (SLC6A4), which is responsible for serotonin reuptake, also influence the efficacy of these drugs.
Nowadays physicians can test CYP2D6 and other antidepressant-metabolizing enzymes before choosing the appropriate antidepressant for the patient.
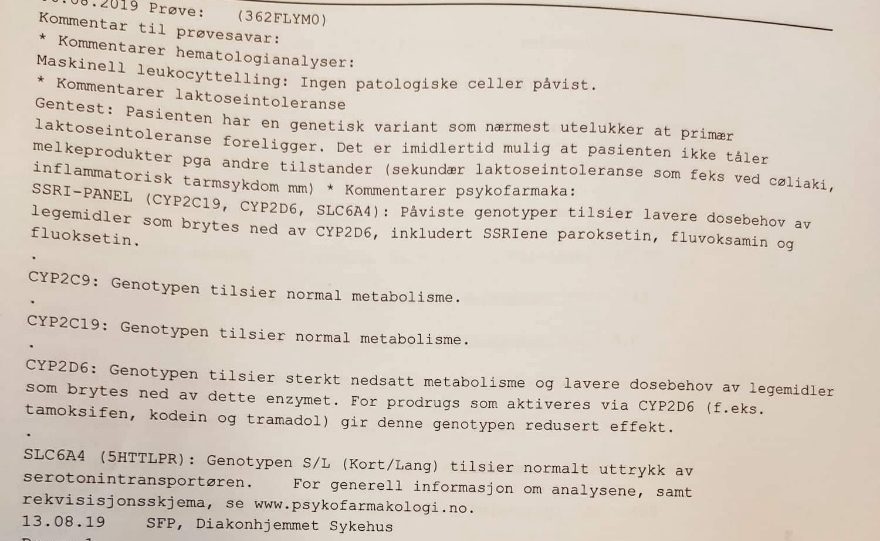
A so-called SSRI panel, which screens for polymorphisms in the most common antidepressant-metabolizing enzymes. It’s in Norwegian, but this patient has severely decreased function of CYP2D6.
N-acetyltransferase type 2
N-acetyltransferase type 2 (NAT2) is a hepatic phase II enzyme. This enzyme acetylates many commonly used drugs, like isoniazid, hydralazine and procainamide. People with wildtype NAT2 are called fast acetylators. People with mutant NAT2 which decreases its activity are called slow acetylators. In the Caucasian population approx. 50% are slow acetylators.
Slow acetylators have increased risk of toxicity when taking these drugs, like:
- Isoniazid
- Polyneuropathy
- Hepatotoxicity
- Hydralazine/procainamide
- Drug-induced lupus
HLA
The effects of some drugs depend on the HLA variant.
Abacavir is a highly effective antiretroviral drug. Its use has been limited by severe adverse effects, most importantly severe rashes. Studies have determined that the development of this adverse effect is closely linked to a certain HLA variant, HLAB*5701. Genetic testing for this variant is considered standard of care before abacavir treatment.
Carbamazepine is an anticonvulsant. It can cause life-threatening hypersensitivity reactions, including Stevens-Johnson syndrome and toxic epidermal necrolysis. These adverse effects are closely linked to another HLA variant, HLAB*1502, which occurs more commonly in certain ethnic groups. Screening for this variant in ethnic groups where it is common is worthwhile. People with this variant can develop hypersensitivity against phenytoin as well.
Targeted drugs
Some drugs are only efficacious in specific subpopulations. These people are called responders, while those who don’t have any effect of the drug are called non-responders. These are pharmacodynamic variations due to the presence of certain proteins inside or on cells.
Trastuzumab is a monoclonal antibody which targets HER2. HER2 is over-expressed in 30% of breast cancers, and so trastuzumab is only efficacious against these breast cancers. Testing for HER2 overexpression is mandatory before trastuzumab treatment, as the treatment would be wasted otherwise.
Gefitinib is a small-molecule EGFR inhibitor. Mutated EGFR, which causes constitutive activation of the receptor, is found in a large percentage of non-small cell lung carcinomas. Testing the patient for these mutations is mandatory before gefitinib treatment.
Pharmacodynamic variations due to diseases
Some diseases cause pharmacodynamic variation in drug response.
Glucose 6-phosphate dehydrogenase deficiency (G6PDD) causes reduced synthesis of NADPH, which again reduces the production of glutathione. This makes them susceptible to drugs which produces oxidative stress, like dapsone or primaquine. Taking these drugs can cause severe oxidative damage to RBC membranes, causing severe haemolysis.
Malignant hyperthermia occurs when people with mutated ryanodine receptor are administered suxamethonium or volatile general anaesthetics. This is due to a mutation in the ryanodine receptor.
Porphyrias are diseases involving the biosynthesis pathway of haem, causing haem precursors to accumulate. Acute intermittent porphyria is the most common form. Some drugs may induce enzymes involved in the biosynthesis of haem, thereby increasing the amount of haem precursors. This most notably occurs with barbiturates.
Effect of age on drug efficacy
Young (<14 years) patients:
Neonates have reduced absorption. Young patients have relatively lower levels of albumin, which increases the effect of drugs which are highly plasma protein binding.
The total body water and extracellular water volumes are relatively higher in young than in adults. The amount of body fat is relatively lower than in adults. These factors alter the distribution of drugs in young patients.
Young patients have higher permeability through the blood brain barrier, the mucous membranes and the skin.
Neonates have decreased activity of phase II biotransformation enzymes in the liver. This results in slower elimination of bilirubin and certain drugs like morphine and chloramphenicol (which causes grey baby syndrome).
In neonates younger than half a year the GFR and tubular excretion capacity is reduced.
Elderly (>65 years) patients:
Elderly have reduced gastric motility and intestinal blood flow. This results in delayed (but still complete) oral absorption.
Like young patients, elderly patients have relatively lower levels of albumin, which increases the effect of drugs which are highly plasma protein binding.
The total body water volume is relatively smaller in elderly than in adults. This causes the volume of distribution (Vd) of hydrophilic drugs to decrease, leading to higher plasma concentration and increased acute effects. On the other hand, the amount of body fat is relatively higher, which leads to increased volume of distribution for lipophilic drugs. This leads to lower plasma concentration of lipophilic drugs.
The function of phase I reactions (like CYP450) is reduced in elderly. They also have decreased hepatic blood flow. This slows down hepatic metabolism, which increases oral bioavailability of drugs which are highly metabolized by the liver during the first pass effect.
Like neonates, elderly have decreased GFR and tubular excretion capacity.
The β adrenergic receptors of elderly have decreased affinity to drugs. Adverse effects of benzodiazepines are more common in elderly, due to decreased hepatic metabolism and increased Vd of lipophilic drugs.
Effect of diet on drug action
Effects on absorption:
Simultaneous consumption of milk reduces the absorption of tetracyclines and fluoroquinolones due to chelate formation.
Consumption of tyramine-rich foods like cheese and red wine can lead to the “cheese reaction” in people taking MAO-A inhibitors.
High fat diet can increase the absorption of lipophilic drugs. However, a high fat diet decreases gastric emptying, which can reduce the absorption of certain drugs.
Effects on distribution:
Severe protein malnutrition can cause hypoalbuminaemia, which influences plasma protein binding drugs.
Effects on metabolism:
Consumption of certain foods can induce hepatic biotransformation enzymes, like broccoli, cabbage, brussels sprouts, ethanol and foods grilled over charcoal. Grapefruit juice on the other hand, inhibits biotransformation enzymes.
Effects on excretion:
Fasting-induced ketosis leads to acidification of the urine, which reduces the renal excretion of weak acid drugs.
Effects on pharmacodynamics:
Certain vegetables, especially leafy green vegetables, are rich in vitamin K and can decrease the effect of coumarins.
Effect of disease on drug action
|
Disease |
Mechanism | Drug effect |
| Pyloric stenosis | Slower gastric emptying, slower intestinal absorption |
Delayed, decreased |
|
Gastric disease |
Decreased production of IF | Decreased B12 absorption |
| Duodenal disease | – |
Decreased iron absorption |
|
Jejunal diseases |
– | Decreased folic acid absorption |
| Ileal diseases | – |
Decreased B12 absorption, decreased enterohepatic circulation of oestrogens |
|
Cholestasis |
– | Reduced absorption of lipid soluble vitamins |
| Congestive heart failure | Backward, forward failure |
Decreased oral absorption, decreased hepatic clearance, decreased hepatic first pass effect |
|
Liver disease, nephrotic syndrome |
Hypoalbuminaemia | Increased effect of plasma protein binding drugs |
| Ascites | Increased Vd |
Decreased effect of hydrophilic drugs |
|
Liver disease |
Decreased metabolism | Decreased hepatic clearance, decreased hepatic first pass effect |
| Kidney disease | Decreased excretion |
Decreased excretion of renally excreted drugs |
|
Hyperthyroidism |
Sensitization of β receptors | Increased effect of catecholamines |
| Myasthenia gravis | Down-regulation of nicotinic acetylcholine receptors |
Increased effect of non-depolarizing muscle relaxants |
Hey man how does the High fat diet reduces the bioavailability of lipophilic drugs?
Fixed that part. This seminar contradicts the pharma 1 seminar on absorption, so it’s kind of confusing. I think it’s fixed now, though.