Table of Contents
Page created on December 23, 2021. Last updated on December 18, 2024 at 16:57
CTG during labour
CTG was already described in topic B5, and this topic assumes you know the basics from there.
Introduction
CTG is often used during labour for intrapartum monitoring to monitor for interrupted foetal oxygenation. Intrapartum CTG has a low specificity but high sensitivity, and so is more suited as a screening tool for interrupted foetal oxygenation.
During normal labour, uterine contractions cause transient interruptions of the foetal oxygenation. This is tolerated by most foetuses, but not all. Intrapartum CTG aims to detect those who don’t.
Indications
Intrapartum CTG is normally not necessary in case of low-risk births but is recommended for births where maternal or foetal risk factors are present.
Method
During labour and after the rupture of membranes, the foetal electrode is placed on the foetal head through the vagina. This also allows for ST analysis.
Evaluation and interpretation
As with antenatal CTG, the baseline foetal heart rate, variability, and presence of decelerations, are all evaluated. Unlike antenatal CTG, the absence of accelerations is not significant. According to these features, the CTG is classified as either normal, suspicious, or pathological, as seen below:
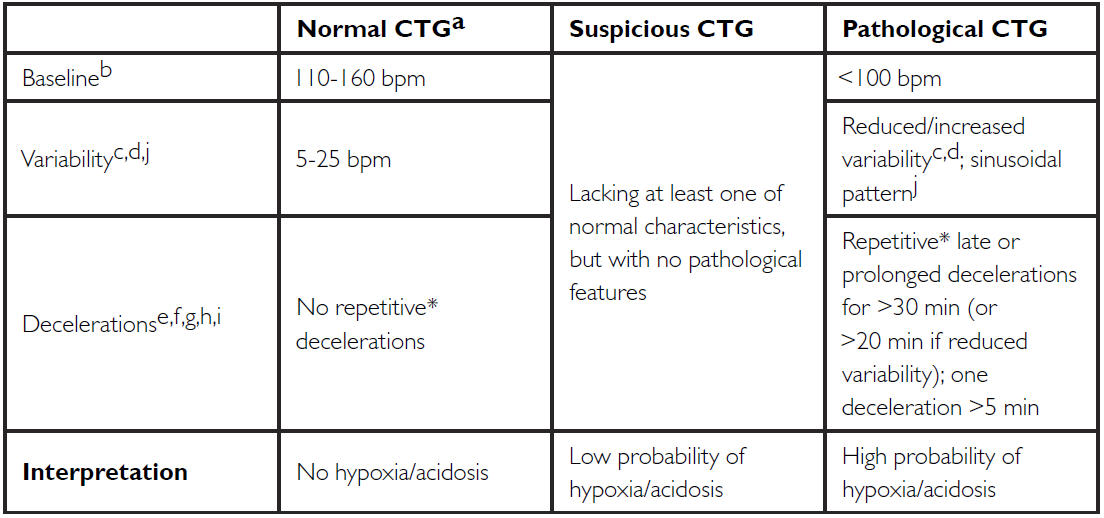
2015 FIGO classification of intrapartum CTG. From https://www.neoventa.com/2015/12/the-2015-figo-classification-of-intrapartum-cardiotocography-differences-to-the-stan-classification/
Management
A pathological CTG is an indication for intervention or further examination. Depending on the severity of the signs, there are multiple options:
- Reposition the mother onto left or right side (may relieve cord compression or improve perfusion)
- Give IV fluids
- Stop uterotonic/Give tocolytic (to decrease uterine contraction frequency)
- Perform scalp blood sampling (see below)
- Initiate operative delivery (C-section or operative vaginal delivery)
Foetal scalp blood sampling
Blood sampling of capillary blood from the foetal scalp may provide further information about the foetal status. This is indicated in case of pathological intrapartum CTG. pH and lactate levels in the capillary blood are measured, which gives information on the acid base status of the foetus. Acidosis is analogous to hypoxia, and usually an indication for operative delivery.
Samples can be repeated. This is especially useful if the first blood sample was normal, but the CTG is still pathological, in which case sampling should be repeated after 30 min/1 hour.
However, foetal scalp blood sampling often fails (up to 10% of cases), it’s difficult to perform, and there isn’t much evidence of it improving important endpoints (number of operative deliveries or long-term perinatal outcome). For these reasons, it’s not widely used.