Table of Contents
Page created on October 24, 2019. Last updated on December 18, 2024 at 16:57
For Norwegians this and this are good sources of some relevant information. This is a good source in English.
ABO testing
See here for general info on blood groups.
See here for details on the Coombs test.
Reaction conditions for ABO test:
- Temperature – 20°C
- Antigen-antibody ratio – 10% suspension of RBCs
- Medium of reaction (ionic strength) – physiological saline
- Reaction time
- Forward test – 5 minutes
- Reverse test – 10 minutes
Control contains patient’s serum + patient’s RBCs. It must be negative for the test to be valid.
Anti-A and anti-B antibodies are IgM.
Forward typing and reverse typing:
In the forward typing the test plate contains anti-A and anti-B antibodies. The patient’s blood will be applied to the test plate, which will or will not react with the antibodies on the test plate. The forward typing detects the presence (or absence) of A and/or B antigens on the patient’s RBCs.
In the reverse typing the test plate contains type A and type B red blood cells. The patient’s serum will be applied to the test plate, which will or will not react with the antigens on the test plate. The reverse typing detects the presence (or absence) of anti-A or anti-B antibodies in the patient’s plasma. The reverse typing is used to confirm the forward typing, at the two tests should show the same result (they should indicate the same blood type).
Rh testing
Reaction conditions for Rh test:
- Temperature – 20°C
- Antigen-antibody ratio – 50% suspension of RBCs
- Medium of reaction (ionic strength) – serum
- Reaction time – 5 minutes
Control contains anti-D control + patient’s RBCs. It must be negative for the test to be valid.
Anti-D antibodies are IgG.
Transfusion compatibility
RBC transfusion:
For transfusion of RBC products, the antigens on the RBCs of the donor blood product are important. The recipient can only receive RBC antigens which the recipient doesn’t have antibodies against. O is the universal donor because O-type RBC’s don’t have any ABO antigens.
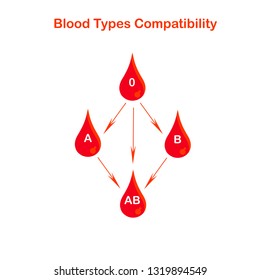
Plasma transfusion:
For transfusion of plasma without RBCs (FFP, cryoprecipitate), the antibodies of the donor plasma are important. The recipient can only receive plasma which doesn’t contain antibodies against the recipient’s own RBC antigens. AB is the universal donor for plasma because plasma from a person with blood type AB doesn’t contain any ABO antibodies.
Preservation of blood
During storage the:
- Lactate concentration increases
- Extracellular potassium increases
- Ammonia concentration increases
- Glucose concentration decreases
- pH decreases
- 2,3-DPG decreases
- ATP decreases
Blood needs to be preserved correctly to keep the blood viable for transfusion without damaging the blood and while keeping it sterile. There are two types:
- Use of blood preservative solutions
- Anticoagulant preservative solutions – to prevent coagulation and preserve viability
- Storage time 28 days
- ACD
- Anticoagulant citrate, dextrose
- CPD (most commonly used)
- Citrate – chelates calcium -> prevents coagulation
- Phosphate – helps ATP production, maintains pH
- Dextrose – energy for RBCs
- (Adenine) – improves ATP availability for RBCs, but can cause hypotension
- Additive solutions
- Gives storage time of 35 days
- For packed RBCs
- Lowers the viscosity of packed RBCs
- Provides nutrients for RBCs after plasma is removed (plasma usually contains nutrients)
- SAGM
- Saline
- Adenine
- Glucose
- Mannitol
- Anticoagulant preservative solutions – to prevent coagulation and preserve viability
- Deep freezing (cryopreservation)
- Additives must be added to prevent freezing-induced damage
- Glycerol
- DMSO
- Blood product is first washed repeatedly, then frozen
- Advantages
- Long-term storage
- Disadvantages
- High RBC loss during washing
- Expensive
- Additives must be added to prevent freezing-induced damage
WBCs in blood:
WBCs in blood products can cause many complications:
- Non-haemolytic febrile transfusion reactions
- Transfusion-associated graft versus host disease
- Virus transmission (CMV, EBV, …)
- HLA alloimmunization – formation of antibodies against HLA
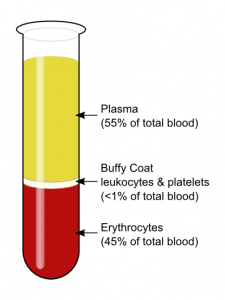
Methods of leucodepletion/leucoreduction (removing WBCs):
- Buffy coat removal – removes only 80% of WBCs
- Washing – removing the noncellular fluid in RBC and platelet products and replacing it with saline – removes 70 – 90% of WBCs
- Filtration – removes 99,995% of all WBCs
Irradiation – kills all WBCs but doesn’t remove them. Useful if the function of WBCs is the problem and not the presence (i.e., antigens on them) is the problem, like in transfusion-associated graft-versus-host disease.
Whole blood
Contains whole, unchanged blood.
Preserved with CPD.
Indications:
Rarely used except for significant blood loss.
Packed red blood cells/erythrocyte concentrate
Blood which contains only RBCs and very little plasma. It’s produced by centrifuging blood and removing most of the plasma. Leukocytes are filtered out.
Each unit of packed RBCs increases the Hb by approx. 1,0 g/dL.
Preserved with CPD-A.
Indications:
Most commonly used transfusion product for anaemia. Acute haemorrhage, hypovolaemic shock, symptomatic anaemia.
Indicated in acute anaemia with Hb < 9,0 g/dL. Indicated in chronic anaemia with Hb < 7,0 g/dL. These limits are not absolute; the clinical picture must be taken into account.
These values are slightly wrong according to uptodate, but they will ask them in the exam.
People with chronic anaemia develop compensatory mechanisms, which is why they can function with lower Hb.
Compatibility:
ABO and rhesus must be tested.
Washed RBC concentrate
RBCs which have had the plasma, platelets and WBCs removed and replaced with saline.
SAGM is used as additive.
Indications:
- People with IgA deficiency and anti-IgA antibodies
- People at risk for allergic reactions
- People with previous allergic reactions to blood products
Washing reduces risk for allergic reactions by removing all IgA or other proteins in the plasma of the blood product which the recipient could have an allergic reaction to.
Irradiated blood
Irradiation is the gamma irradiation of cellular blood products. It reduces the risk for transfusion-associated graft-versus-host disease (TA-GVHD) by destroying all WBCs. See the section on transfusion complications for more information.
Irradiated RBCs last 14 days.
Indications:
- Blood transfusion of relatives
- Congenital or acquired immunosuppressed conditions
Fresh frozen plasma (FFP)
Plasma with all cells removed. Pure plasma.
To lower the risk of transmitting viruses the plasma harvested from a person is stored and unused for 4 months, and the donor has to repeatedly test negative for HIV and HCV for these 4 months. If always negative the FFP can be given.
Indications:
- Warfarin overdose
- Clotting factor deficiency
- Cirrhosis
- DIC
- Congenital coagulation factor deficiency
- Massive transfusion
Compatibility:
ABO must be tested. Rhesus not necessary to test.
Cryoprecipitate
Contains clotting factors. Fibrinogen, factor VIII, factor XIII, vWF and fibronectin. Produced by centrifugation of FFP.
Indications:
- Similar as for FFP, but better if large transfusion volumes are undesirable
- Fibrinogen supplementation
- Factor VIII supplementation
- Coagulation factor deficiency
- Cirrhosis
- DIC
Platelet concentrate
Indications:
Thrombocytopaenia.
White blood cell products
Indications:
- Severe bacterial infection
- Neonatal sepsis
Complications:
- Frequent!
- Anaphylaxis
- Respiratory distress syndrome
- etc
Storage of blood products
| Storage temperature | Blood product | Storage time |
|---|---|---|
| 22°C | Platelets | 5 days |
| 22°C | Granulocytes | 24 hours |
| 4 °C | Packed RBCs | 35 days |
| 4 °C | Washed RBCs | 24 – 48 hours |
| 4 °C | Irradiated RBCs | 14 days |
| -18 – -25 °C | FFP | 3 months |
| < -30 °C | FFP | 2 years |
Transfusion reactions
Most commonly caused by clerical errors, like giving the blood to the wrong patient, drawing the wrong blood specimen, failing proper patient identification, wrong labelling, performing the ABO test wrong, etc.
- Immune-related complications
- Antigen-antibody-mediated reactions
- Acute haemolytic transfusion reaction
- Delayed haemolytic transfusion reaction
- Post-transfusion purpura
- Transfusion-related acute lung injury (TRALI)
- Anaphylaxis
- Immune cell-mediated reactions
- Transfusion-associated graft-versus-host disease (TA-GVHD)
- Transfusion-related immunomodulation (TRIM)
- Antigen-antibody-mediated reactions
- Non-immune-related complications
- Transfusion-related circulatory overload (TACO)
- Transfusion of infected blood – sepsis
- Hypothermia due to cold blood transfusion
- Massive transfusion syndrome
- Transfusion of haemolytic blood
- Air embolism
- Citrate intoxication – hypocalcaemia
- Transfusion of hyperkalaemic blood
- Haemosiderosis
- Thromboembolism
According to timeline:
- Immediate complications (0 – 15 minutes)
- Acute haemolytic transfusion reaction
- Anaphylaxis
- Air embolism
- Early complications (15 minutes – 24 hours)
- Transfusion-related circulatory overload (TACO)
- Citrate intoxication – hypocalcaemia
- Transfusion of infected blood – sepsis
- Hypothermia due to cold blood transfusion
- Thromboembolism
- Late complications (1 – 7 days after transfusion)
- Transfusion-associated graft-versus-host disease (TA-GVHD)
- Delayed haemolytic transfusion reaction
- Very late complications (weeks, months, years after transfusion)
- Haemosiderosis
- Transmission of pathogens
- Hepatitis
- Herpes viruses
- HIV
- Syphilis
- Malaria
Acute haemolytic transfusion reaction
Etiology:
- ABO incompatibility (most common)
- Incompatibility of other blood groups (rare)
- Kidd incompatibility
- Rh incompatibility
- Kell incompatibility
- etc.
Pathophysiology:
- Recipient antibodies binding to A or B antigens on donor RBCs -> complement activation, phagocyte activation -> haemolysis of donor RBCs
- Activation of bradykinin (kallikrein-kinin system) -> vasodilation, hypotension, increased capillary permeability
- Hypotension -> release of catecholamines (neuroendocrine response) -> vasoconstriction in organs rich in vascular alpha-adrenergic receptors, such as kidneys, lung, gastrointestinal tract, and skin -> tissue hypoxia, kidney damage
- Complement activation -> cytokine release, granulocyte degranulation -> fever, hypotension, bronchospasm
- Activation of factor XII -> DIC
Clinical features:
- Rapid onset after transfusion
- Fever
- Chills
- Suffocation
- Burning pain at IV site
- Back pain, chest pain
- Patients in coma or general anaesthesia
- Bleeding in surgical area (wounds, punctures)
- Hypotension
Complications:
- Acute kidney injury
- DIC
- Jaundice
- Shock
Treatment:
- Stop transfusion immediately if any suspicion -> confirm diagnosis with direct Coombs test and re-do compatibility testing
- Supportive treatment
- Fluids
- Electrolyte correction
- etc
Delayed haemolytic transfusion reaction
Etiology:
Patients who were previously sensitized to (and therefore have antibodies against) certain RBC antigens like KIDD or D antigens. Sensitization can occur during transfusion, pregnancy or transplantation.
Pathophysiology:
Antibodies bind to donor RBCs -> complement and phagocyte-mediated haemolysis.
Clinical features:
- Weeks after transfusion
- Similar as acute haemolytic transfusion reaction but less severe
- Can even be asymptomatic
Diagnosis:
Positive direct Coombs.
Treatment:
Not necessary unless there is renal impairment, just monitoring. Rarely fatal.
Non-haemolytic febrile transfusion reactions
Common complication! 0,5 – 6% of cases.
Etiology:
Cytokines (pyrogens) produced by WBCs and released from RBCs during storage cause fever. Or, the recipient has antibodies against granulocytes or platelets, lysing them and releasing cytokines.
Clinical features:
- Fever
- Flushing
- Chills
Treatment:
Stop transfusion. Give paracetamol.
Prevention:
Leukoreduction.
Post-transfusion purpura
Etiology:
The recipient has anti-platelet antibodies, mostly anti-HPA-1a (human platelet antigen 1a), which will destroy both recipient and donor platelets upon transfusion.
Clinical features:
- 5 – 10 days after transfusion
- Thrombocytopaenia
- Purpura
- Fever
Treatment:
- IVIG (intravenous immunoglobulin)
- Highly purified immunoglobulins from a donor
- Regulates immune system
- Plasmapheresis
- Steroid
Transfusion-related acute lung injury (TRALI)
Etiology:
Anti-HLA or anti-HNA antibodies in donor product activates the recipient’s granulocytes.
Clinical features:
- Within 6 hours
- Dyspnoea
- Hypoxia
- Cyanosis
- Hypotension
- Bilateral pulmonary oedema
Treatment:
- Mechanical ventilation
- Steroids
Anaphylaxis, allergy
Etiology:
- People with IgA deficiency
- Allergens inside transfused product (drugs etc)
- IgE inside transfused product
Pathophysiology:
People with congenital IgA deficiency can have anti-IgA antibodies. These antibodies bind to IgA in the donor plasma and initiate allergic reaction.
Clinical features:
- Allergy (mild reaction)
- Malaise
- Itching
- Urticaria
- Fever
- Anaphylaxis
- Laryngeal oedema
- Anaphylactic shock
Treatment:
- Fluid replacement
- Antihistamines
- Steroids
- Epinephrine
- Airway stabilization
Prophylaxis:
- IgA-free blood (washed blood) to IgA deficient patients and patients who previously had allergic reaction to transfusion
Transfusion-associated graft versus host disease (TA-GVHD)
Etiology:
- Blood transfusion from relatives
- Severely impaired immunity
Pathophysiology:
Donor lymphocytes are usually identified as foreign and destroyed by the recipient’s immune system, but when the donor and recipient HLA type is similar (relatives) the recipient’s immune system cannot recognize and destroy the donor lymphocytes. Immunodeficient persons also cannot destroy the donor lymphocytes. Donor T cells engraft in the recipient and recognize the recipient’s cells as foreign and mounts an immune response against recipient tissues.
Clinical features:
- Days or weeks after transfusion
- Fever
- Rash
- Liver dysfunction
- Pancytopaenia
Mortality > 90%
Treatment:
Largely ineffective. Immunosuppressive therapy?
Prevention:
Giving irradiated blood products to patients at risk for TA-GVHD.
Transfusion-related immunomodulation
Etiology:
Not well known.
Clinical features:
- Transient immunosuppression occurring after allogenic blood transfusion
Prophylaxis:
Leukodepletion of blood products.
Transfusion-related circulatory overload (TACO)
Etiology:
Large transfusion volume, too fast infusion, cardiovascular or renal disease.
Clinical features:
- Hypervolaemia
- Dyspnoea
- Headache
- Hypertension
- Pulmonary oedema
Therapy:
Stop transfusion. Upright position, diuretics, oxygen.
Prevention:
Slow infusion.
Massive transfusion
Massive transfusion is the treatment of patient with severe shock. It can be lifesaving but can cause problems.
Clinical features:
DIC, tissue hypoxia, bleeding.
Treatment:
Fluid replacement, blood transfusion, cardiac support.
Cold blood transfusion
Etiology:
Transfusion of too much unheated blood.
Clinical features:
- Decrease in tissue oxygenation
- Bleeding
- Arrhythmias
- Exacerbates symptoms of hypokalaemia and hyperkalaemia
Prevention:
Use of blood warmer.
Transfusion of infected blood
Etiology:
Infection source
- Poor venepuncture technique
- Inappropriate blood storage
- Incorrect handling
Clinical features:
- Severe shock
- Intravascular haemolysis
Treatment:
Stop transfusion. Supportive therapy for shock. IV broad spectrum antibiotics.
Haemosiderosis
Etiology:
50 – 100 units of RBC transfusion.
Clinical features:
Bronze skin, cirrhosis, heart failure.
Treatment:
Iron chelation, phlebotomy.
Pathogens in blood
- In plasma
- Hepatitis viruses
- HIV
- Parvovirus B19
- Treponema pallidum
- In RBCs
- Plasmodium (malaria)
- Babesia microti
- In WBCs
- HIV
- EBV
- CMV
- Toxoplasma gondii
Hi thank you for your hard work.
I cannot see the link of general info of blood group and coombs test.
I’ve fixed both links now. Thanks for telling me
hello greek.doctor
your note + lecture , is it enough for the exam or I should also read the link you put at the beginning of the blood tranfusion ?
many thanks.
Notes + lectures is more than enough.
Perfect!! Thank you so much