Table of Contents
Page created on September 7, 2018. Last updated on December 18, 2024 at 16:57
Effects of muscarinic receptor antagonists
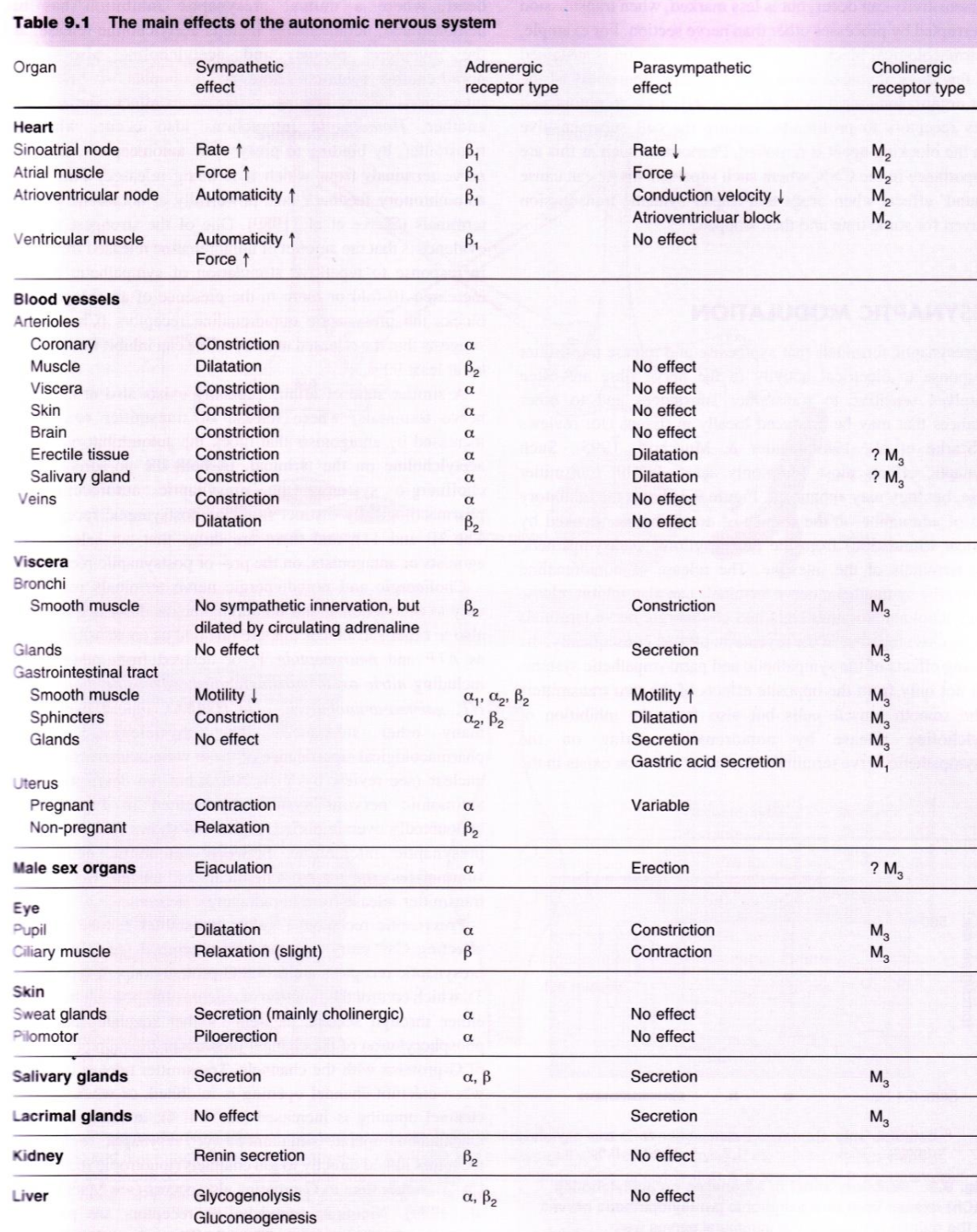
The muscarinic receptor antagonists have the following effects (mostly the opposite of the parasympathetic system):
- Mydriasis, increased intraocular pressure, cycloplegia (they block accommodation), decreased tear secretion, photophobia
- Tachycardia
- Bronchodilation, decreased bronchial secretion
- Decreased gastrointestinal secretion, decreased motility and peristalsis, constriction of sphincters
- Relaxation of detrusor muscle
- Decreased sweating, hyperthermia in high doses (due to the decreased sweating)
Generally speaking, parietal cells and CNS innervated by M1, heart is innervated by M2, while M3 innervates the rest, e.g. the eye, GI tract, bronchial smooth muscle and salivary gland secretion.
Muscarinic antagonists
This class of drugs are competitive antagonists of muscarinic receptors, so they decrease parasympathetic activation. Because of this they are called anticholinergics, and sometimes parasympatholytics or cholinolytics. They are mostly non-selective (meaning they act on all muscarinic receptor subtypes, not just one subtype), but a few are selective.
Compounds
Tertiary muscarinic antagonists (good oral bioavailability and CNS penetration):
- Muscarinic antagonists with multiple uses
- Atropine
- Drugs for motion sickness
- Scopolamine
- Opthalmological drugs
- Cyclopentolate
- Homatropine
- Tropicamide
- Drugs for overactive bladder
- Oxybutinin
- Tolterodine
SolifenacinDarifenacin
- Drugs for Parkinson disease
- Benztropine
- Biperiden
Quaternary muscarinic antagonists (poor oral bioavailability and CNS penetration):
- Drugs for bronchial asthma and COPD
- Ipratropium bromide (Atrovent®)
- Tiotropium bromide
- Drugs used as spasmolytics
Butylscopolamine
- Drugs used as premedication before intubation
Glycopyrrolate
- Drugs used to treat peptic ulcers
- Pirenzepine (rarely used)
Atropine and scopolamine are natural compounds from the plant Atropa Belladonna.
The drugs in strikethrough were not covered in lecture and you won’t need to know them for the exam, but I’ve included them because you will encounter them in clinical practice.
Indications
Atropine has many uses:
- Sinus bradycardia
- Cholinergic poisoning
- Premedication before intubation (decreases salivary and respiratory secretions)
- Uveitis
- Induce mydriasis for diagnostic purposes
Scopolamine is used to treat motion sickness, often administered as a transdermal patch.
Cyclopentolate, homatropine, and tropicamide are used to treat uveitis and to induce pupil dilation and cycloplegia (paralysis of the ciliary muscle) for diagnostic purposes.
Oxybutinin, tolterodine, solifenacin, and darifenacin are used to treat urinary incontinence due to overactive bladder.
Benztropine and biperiden can be used to treat Parkinson disease.
Ipratropium and tiotropium are used as bronchodilators to treat COPD and bronchial asthma. They are given as inhalation.
Butylscopolamine is related to scopolamine but does not cross the BBB and therefore only acts peripherally. It relaxes smooth muscle and is used to treat colicky pain, like biliary colic, ureteric colic, and intestinal colic.
Glycopyrrolate is used to decrease respiratory and gastrointestinal secretions ahead of surgery, to prevent these secretions from interfering with intubation. It’s given as a premedication.
Pirenzepine is unique in that it is a selective muscarinic subtype 1 (M1) antagonist. It inhibits gastric secretions and may be used to treat peptic ulcers. It is very rarely used nowadays so I don’t think it’s worth learning.
Pharmacokinetics
The quaternary amine drugs are hydrophilic and therefore poorly absorbed and unable to cross the blood-brain barrier to have any effects on the CNS. These drugs are administered parenterally, as IV, as inhalation, etc.
Drugs with the tertiary ammonium group are lipophilic and can cross the BBB and will have CNS effects. Tertiary ammonium drugs can be absorbed through the GI tract, unlike quaternary drugs. Scopolamine can even be absorbed transdermally.
Atropine has a short half-life of only 2 hours, except when used in eyedrops, where the half-life is 72 hours.
Side effects
It’s important to know the side effects of anticholinergics well. The side effects are basically opposite of the parasympathetic effects of the body.
- Ophthalmological side effects
- Dry eyes
- Mydriasis
- Gastrointestinal side effects
- Dry mouth
- Constipation
- Cardiovascular side effects
- Tachycardia
- Urinary system side effects
- Urinary retention
- CNS side effects
- Confusion, disorientation
- Excitement, agitation
- Hallucination
- Delirium
- Coma
CNS side effects occur only with tertiary compounds, and mostly in elderly.
Contraindications
The CNS side effects of anticholergic drugs may be quite severe, and so drugs with anticholinergic effects should often be avoided in elderly.
Proper contraindications of anticholinergics are those conditions where anticholinergic side effects would worsen the condition, for example:
- Obstruction of the GI tract (ileus)
- Obstruction of the urinary tract
- Glaucoma
- Myasthenia gravis
Atropine poisoning
The symptoms of atropine poisoning/anticholinergic overdose are similar to the side effects of anticholinergics except more severe:
- Hot, dry, red skin
- Hyperthermia
- Urinary retention
- Confusion, hallucination, convulsion
- Dry mouth
- Mydriasis
- Tachycardia
Atropine intoxication is treated with physostigmine, diazepam (a benzodiazepine sedative (Valium®)), and cooling.
Other drugs with anticholergic effect
Some other drugs block muscarinic receptors (in addition to the receptors they target for their intended effect). These drugs may also cause anticholergic side effects. These include:
- Tricyclic antidepressants
- First-generation antipsychotics
- First-generation antihistamines
Dear Abu Greek,
“Mirabegron is special because it is a selective muscarinic subtype 3 (M3) antagonist”
Isn’t it a selective Beta-3 adrenergic receptor agonist ?
Thank you …Great work 🙂
Yeah, I mixed it up. Thanks.
Hello! Was just wondering, should it not be spinchter constriction in the GI, on the effect of cholinergic antagonists? I see you have written relaxation of spinchters!
(Love your notes!!)
Hello, yes. good catch! Thanks!