Table of Contents
Page created on September 11, 2018. Last updated on December 18, 2024 at 16:57
Overview of drugs
| Prejunctionally-acting agents | Non-depolarizing neuromuscular blockers | Depolarizing neuromuscular blockers | Drugs for reversal of neuromuscular blocking |
| Botulinum toxin | (Cis)atracurium | Suxamethonium (succinylcholine) | Sugammadex |
| Hemicholinium | Mivacurium | ||
| Triethylcholine | Pancuronium | ||
| Vesamicol | Rocuronium | ||
| Tubocurarine | |||
| Vecuronium |
Sometimes, we need to use drugs to paralyze skeletal muscles. This type of drug is used during surgery to induce muscle paralysis and relaxation. These drugs to not cause anaesthesia, so anaesthetic drugs must be supplied as well. They’re supplied parenterally and act on all skeletal muscles, including the respiratory muscles. There are two types of neuromuscular blockers, non-depolarizing and depolarizing types.
All drugs in this topic are peripherally acting skeletal muscle relaxants. Centrally acting skeletal muscle relaxants are detailed in pharma 2.
So you forgot about the neuromuscular junction
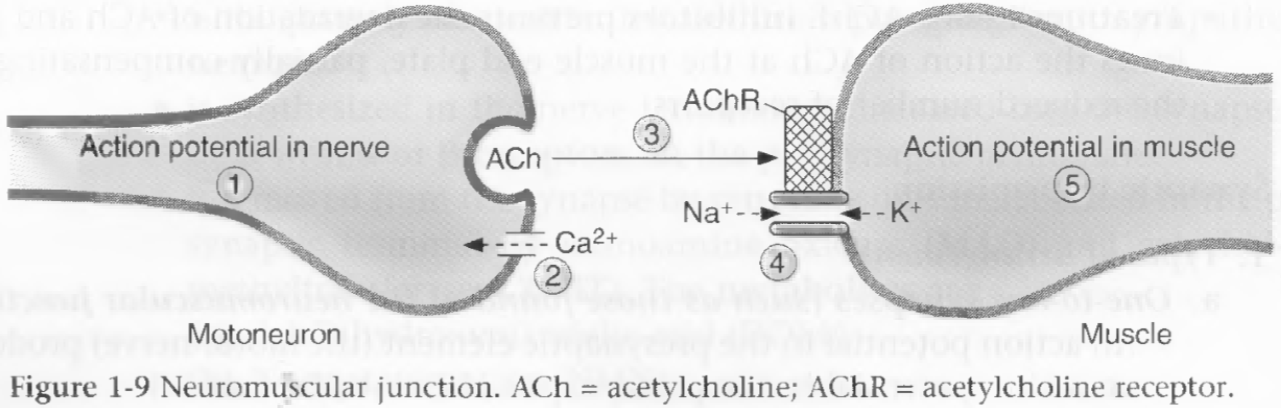
The neuromuscular junction is the synapse between the axons of motoneurons and the skeletal muscle. The presynaptic terminal is the end of the axon, the postsynaptic membrane is the membrane of the skeletal muscle. The synaptic cleft is the space in-between.
Action potentials are conducted down the motoneuron, which depolarizes the presynaptic terminal. This opens voltage-gates Ca2+-channels, causing the presynaptic terminal to take in Ca2+. The Ca2+ influx causes the presynaptic terminal to release pre-synthetized acetylcholine into the synaptic cleft by exocytosis. The molecules of acetylcholine diffuse to the nicotinic acetylcholine receptor on the postsynaptic membrane, which opens Na+ and K+ ion channels, which depolarizes the postsynaptic membrane.
Non-depolarizing neuromuscular blockers
Compounds
- Atracurium
- Cisatracurium
- Mivacurium
- Pancuronium
- Rocuronium
- Tubocurarine
- Vecuronium
Indications
Non-depolarizing neuromuscular blockers are usually used for long-term motor paralysis. The paralysis occurs within 1-5 minutes of parenteral administration. They last for 20-90 minutes, depending on the drug. They are all quaternary amines, meaning they are not well absorbed from the gut and they do not cross the blood-brain barrier.
The medical uses of neuromuscular blockers are the following:
The main medical use of neuromuscular blocker is to make endotracheal intubation easier and less risky. This is most frequently performed before induction of general anaesthesia, as general anaesthetics also stops the patient from breathing and protecting their own airways. They may also be used to make certain surgeries easier by reducing patient movement and muscle tone.
Tubocurarine is a plant poison and is the “prototype” for most non-depolarizing neuromuscular blockers. It has a long duration of action. It causes significant ganglion blockade and histamine release, which makes it unfit for clinical practice.
Mechanism of action
The non-depolarizing neuromuscular blockers are competitive antagonists of the postsynaptic nicotinic acetylcholine receptors in the neuromuscular junction. In other words, they bind to the postsynaptic receptors that acetylcholine usually binds to and prevent acetylcholine from binding to it. This does so that the signal from the motoneuron is unable to cross the synaptic cleft, which prevents the muscle from depolarizing. Hence, the name non-depolarizing.
The sequence of paralysis is the external eye muscles, then the facial muscles, then the pharyngeal muscles, then the extremities, then trunk, and finally the respiratory muscles. The paralysis subsides in the reverse order.
The effect of this type of drug is called curarization (after the prototype drug, tubocurarine), and the process of reversing the effect is called decurarization.
Reversal
Decurarization can be accomplished by reversible cholinesterase inhibitors like neostigmine. These cholinesterase inhibitors allow acetylcholine to remain longer in the synaptic cleft, which gives them a larger opportunity to compete with the blocker drugs and eventually outcompete them.
Sugammadex is a drug that can bind to vecuronium and rocuronium in plasma to inhibit their effect, thereby decurarizing without the administration of cholinesterase inhibitors, making muscle relaxant reversal simpler. Sugammadex is expensive, however, and so is not widely used everywhere yet.
Side effects
Because nicotinic receptors are found on autonomic ganglia as well (both parasympathetic and sympathetic), some of these drugs like pancuronium can have ganglion-blocking effects as well, causing side-effects like hypotension and tachycardia.
Some drugs belonging to this class are also highly basic (alkaline), which triggers histamine release, causing side-effects like bronchospasm, itching and hypotension. This is true for atracurium and mivacurium. Cisatracurium is similar to atracurium but doesn’t cause histamine release.
Vecuronium and rocuronium have fewest side effects.
Interactions
The effect of non-depolarizing muscle relaxants is increased by general anaesthetics, aminoglycosides and tetracycline, two classes of antibiotics. It is also increased in myasthenia gravis patients, as they have a lower number of functional nicotinic receptors.
The effect is decreased by cholinesterase inhibitors and by upper motoneuron lesions, as these cause the postsynaptic membrane to have more nicotinic receptors.
Pharmacokinetics
Most of these drugs are quaternary ammonium compounds and therefore poorly absorbed. Most are excreted by the kidneys.
- Short duration of action and fast onset
- Mivacurium
- Intermediate duration of action and intermediate onset
- (Cis)atracurium
- Vecuronium
- Long duration of action and slow onset
- Pancuronium
- Tubocurarine
Mivacurium and atracurium are mostly eliminated by enzymatic hydrolysis, mivacurium by butyrylcholinesterase in the plasma. Atracurium is broken down by spontaneous non-enzymatic hydrolysis in plasma, called Hofmann elimination.
Depolarizing neuromuscular blockers
Compounds
Only one drug belongs to this category, suxamethonium (or succinylcholine). It works in a very different manner than the non-depolarizing type.
Indications
Suxamethonium has the fastest onset of action, and the shortest duration of action (5-10 minutes). This makes it the best fit for so-called rapid sequence intubation, where intubation must occur quickly. It’s not often used for maintenance of muscle relaxation during surgery.
Mechanism of action
Suxamethonium is also called succinylcholine, and is, as the name implies, structurally similar to acetylcholine. This drug is actually a nicotinic receptor agonist, which causes the skeletal muscle to depolarize when it binds to the receptor. However, unlike acetylcholine, suxamethonium cannot be hydrolysed by acetylcholinesterase, only by butyrylcholinesterase, meaning that when it binds to a receptor, it will stay bound for a long time.
By staying bound to the nicotinic receptor, the muscle cell will stay depolarized (-50mV membrane potential). This causes the voltage-gated Na+ channels to be unable to go back to the resting state, which makes the postsynaptic membrane unable to be excited, and the muscle unable to contract, causing paralysis! This is called the phase I block. This wave of depolarisation is visible on the patient as fasciculations, followed by flaccid paralysis.
If cholinesterase inhibitor were to be administered during the phase I block, the strength of the block will be increased, because succinylcholine will stay even longer.
There is also a phase II block, which only occurs when the suxamethonium treatment has lasted for a certain amount of time. The postsynaptic membrane slowly repolarizes as suxamethonium is unbound from the receptors and hydrolysed; however, the nicotinic receptors are now severely desensitized because the drug has been bound to them for so long. Densensitization means that the cell has removed many receptors from the membrane surface, so that very few receptors are now present. There are so few present that even if acetylcholine binds to the receptors is it not enough to cause depolarization.
In contrast to in phase I, administration of cholinesterase inhibitors will reverse the phase II block, because the inhibitors allow endogenous acetylcholine to stay for longer. When Ach can stay longer they compensate for the low number of receptors and cause depolarization.
Pharmacokinetics
Succinylcholine is hydrophilic, meaning it is poorly absorbed from the gut and does not enter the brain. The effect of succinylcholine is prolonged in people with genetic cholinesterase deficiency, in infants, in patients with liver damage, by cholinesterase inhibitors and by other drugs that are metabolized by butyrylcholinesterase.
Adverse effects
The excessive depolarization of muscles causes large efflux of potassium ions, potentially causing hyperkalaemia. Malignant hyperthermia, increased intragastric pressure and vomiting (caused by depolarization of muscles of the abdominal wall can also occur.
Malignant hyperthermia is a genetic condition where the patient has a certain mutation in the gene for the ryanodine receptor, which causes enormous Ca2+ release from the sarcoplasmic reticulum in response to succinylcholine or inhaled general anaesthetics. It causes isotonic muscle contractions of all muscles in the body, which increases heat production. The increased energy need will cause a switch to anaerobic metabolism and therefore cause lactic acidosis. The muscle fibres can degenerate (rhabdomyolysis) which releases myoglobin into the blood, which can cause acute renal failure.
It is treated with dantrolene, a ryanodine receptor blocker, bicarbonate for the acidosis and physical cooling to prevent damage from the hyperthermia.
Prejunctionally acting agents
Some drugs don’t directly affect the postsynaptic nicotinic receptors but instead the presynaptic release of acetylcholine. These include hemicholinium, triethylcholine and vesamicol, none of which have clinical relevance and probably aren’t important.
Botulinum toxin is used in cosmetic surgery, blepharospasm, strabismus, spasticity, hyperhidrosis and overactive bladder. The effect lasts for several months.