Table of Contents
Page created on January 5, 2019. Last updated on December 18, 2024 at 16:57
Respiratory pharmacology
Pharmacokinetics:
It’s preferable to administer anti-asthmatic medication by inhalation, because the drug directly reaches the site where it is needed -> onset is quicker and fewer systemic side effects. A particle size of around 1 µm is preferred. Oral treatment is more efficacous but has more side effects and is therefore reserved for severe cases where inhalatory treatment is insufficient.
Inhaler devices:
There are two inhaler devices which are most common in the treatment of respiratory diseases, the pressurized metered-dose inhaler and the dry powder inhaler.
The pressurized metered-dose inhaler (pMDI) contains a liquid formulation containing the active drug dissolved in a liquefied gas propellant. When the inhaler is activated the pressurized propellant will be broken into an aerosol which is then inhaled. The aerosol contains the drug in micron-sized particles which will reach the airways.
The dry powder inhaler (DPI) contains the drug in powder form without a propellant. The force of the patient inhaling will entrain powder from the inhaler and break the powder into micron-sized particles which will reach the airways.
Asthma
Bronchial asthma is a common chronic disease characterized by periodic, recurrent, reversible airway obstruction. These “asthma attacks” can be deadly and occur due to bronchospasm, swelling of the bronchial mucosa and formation of mucus plugs.
Classification:
Two types of asthma exist: extrinsic (allergic) asthma, where there is a type I hypersensitivity reaction, and intrinsic (non-allergic), where there is no hypersensitivity. Asthmatic attack in people with extrinsic asthma occurs when they inhale something they’re allergic to, like dust or pollen.
Asthmatic attack in people with intrinsic asthma can be provoked due to cold air, viruses, stress and other factors.
Pathophysiology:
Asthma is an inflammatory disease where there is non-specific bronchial hyperreactivity, meaning that the bronchial smooth muscle is very sensitive to various stimuli. This hyperreactivity occurs due to chronic airway inflammation.
In extrinsic asthma two things occur when the mast cells bind the antigen: in the immediate phase does bronchospasm occur, which causes the characteristic asthmatic attack. In the late phase will there be airway inflammation, together with lesser bronchospasm.
Treatment:
In 2019 the Global Initiative for Asthma (GINA) changed their recommendations on asthma treatment. This topic is changed to reflect these changes.
With the correct pharmacological treatment most patients can achieve good control of their asthma. The long-term goals of asthma management are to decrease the risk of asthma-related death and exacerbations while providing symptom control. The treatment can be divided into two:
A chronic treatment with anti-inflammatory drugs, also called a controller. These are drugs which the patient takes regularly to reduce the frequency and severity of asthma attacks. They decrease the chronic inflammation of the airways, thereby treating the underlying cause of asthma.
A symptomatic treatment with bronchodilators, also called a reliever. These are drugs which the patient takes only during asthma attacks, to decrease their duration and severity. They induce bronchodilation.
Older recommendations said that people with mild asthma should receive only bronchodilating treatment and no anti-inflammatory treatment. This has recently been shown to increase the risk of exacerbation and loss of lung function, and GINAs 2019 recommendations have therefore been changed to include anti-inflammatory drugs even for people with mild asthma.
The exact treatment should be tailored to the individual patient, but GINA provides recommendations on where to start. The recommendations are organized in “steps”. The patient should begin in step 1 and should step up if the condition doesn’t improve in 2 – 3 months.
The preferred controller is an inhalatory corticosteroid like budesonide in low dose, often in combination with a long-acting β2-agonist like formeterol. The combination is called “bud-form”.
The preferred relievers are bud-form or short-acting β2-agonists like salbutamol or terbutaline.
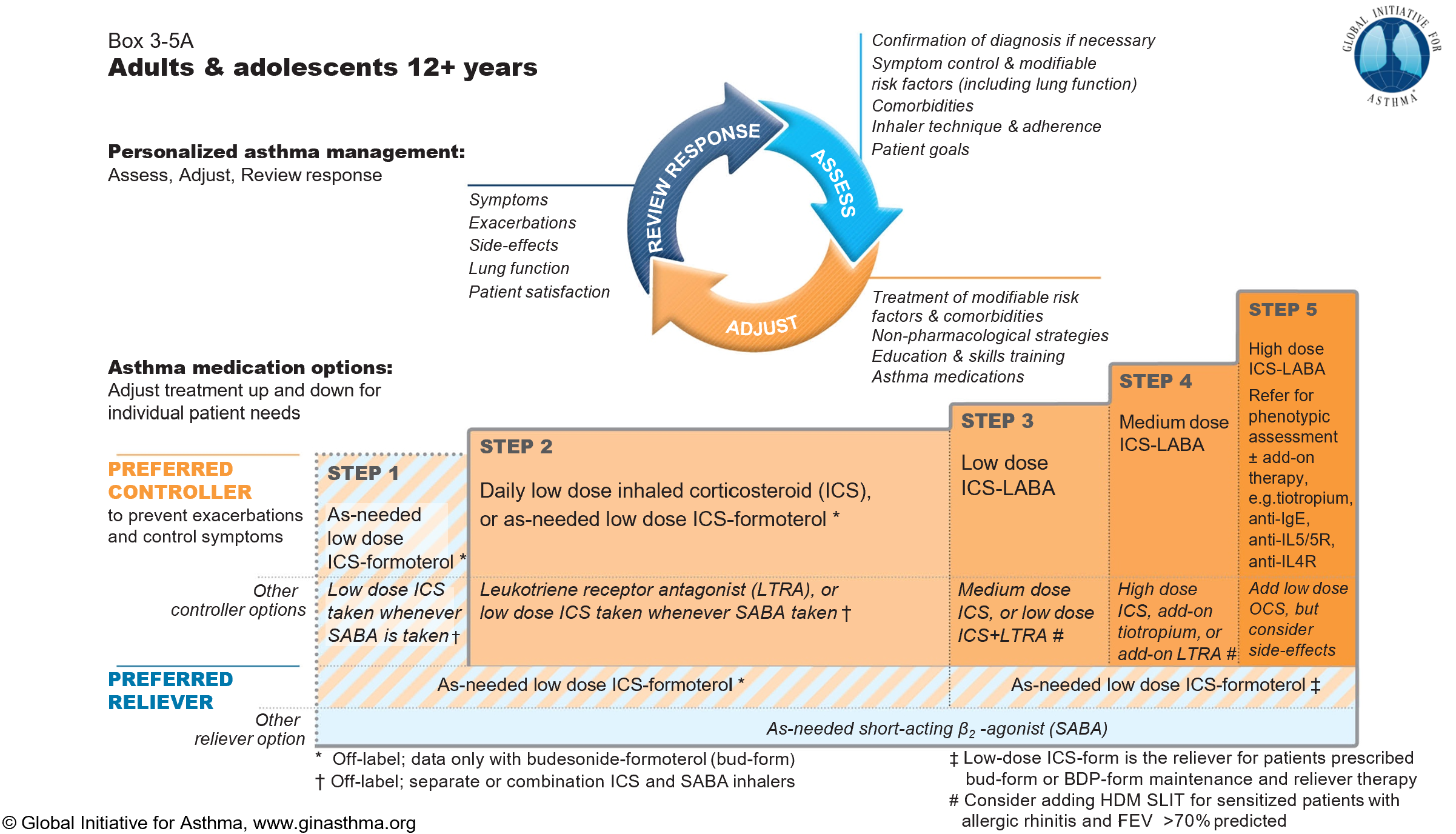
This is a normal treatment plan for asthma. Here you can see which treatments should be used for the different severities of asthma. SABA = short acting β2-agonist, LABA = long-acting β2-agonist
Bronchodilators
- β2-agonists
- Short-acting β2-agonists (SABA) (4 – 6 hours)
- Terbutaline
- Salbutamol/albuterol (Ventoline®)
- Long-acting β2-agonists (LABA) (6 – 12 hours)
- Formoterol
- Salmeterol
- Ultra long-acting β2-agonists (ultra-LABA) (12 – 24 hours)
- Vilanterol
- Short-acting β2-agonists (SABA) (4 – 6 hours)
- Muscarinic antagonists
- Ipratropium (short-acting) (Atrovent®)
- Tiotropium (long-acting)
- Theophylline
Indications:
SABAs are used as relievers in all steps of asthma treatment.
LABAs and ultra-LABAs are used in combination with inhaled corticosteroids as controllers. The use of LABA without corticosteroids is associated with severe adverse outcomes, so they should always be combined. Salmeterol has a slow onset of action (30 min) and can therefore not relieve acute attacks.
Muscarinic antagonists are used as add-on relievers in higher steps.
Theophylline is very rarely used anymore. This is because:
- It has a narrow margin of safety
- It cannot be given as inhalation to prevent systemic side effects
- Clearance differs considerably between persons
- It has multiple drug interactions
- It is cardiotoxic and neurotoxic
Other bronchodilators have none of these drawbacks.
Mechanisms of action:
β2-agonists activate the β2 adrenergic receptor on bronchial smooth muscle, which causes smooth muscle relaxation and therefore bronchodilation. Muscarinic antagonists block muscarinic M3 receptors on bronchial smooth muscle, causing relaxation and bronchodilation.
Theophylline is a non-specific phosphodiesterase inhibitor and adenosine receptor antagonist. By inhibiting PDE theophylline increases intracellular cAMP and cGMP in bronchial smooth muscle, causing relaxation. However, theophylline doesn’t inhibit PDE at the therapeutic range of plasma concentrations so we’re not exactly sure how it works.
Pharmacokinetics:
Theophylline is given orally and is well absorbed. It’s metabolized by CYP enzymes in the liver and is therefore prone to interactions with many drugs. This is important because theophylline has a narrow therapeutic window, so any drug interaction can be severe.
Adverse effects:
- β2-agonists
- Tachycardia
- Tremor
- Muscarinic antagonists
- Dry mouth
- Theophylline
- Insomnia
- Nervoussness
- Arrhythmia
- Seizures
Anti-inflammatory drugs
- Corticosteroids
- Inhaled
- Budesonide
- Beclometasone
- Fluticasone
- Oral
- Prednisone
- Prednisolone
- Methylprednisolone
- Inhaled
- Leukotriene antagonists
- Montelukast
- Zafirlukast
- Biological therapy
- Anti-IgE – omalizumab
- Anti-IL4R – dupilumab
- Anti-IL5 – mepolizumab
- Anti-IL5R – benralizumab
Indications:
All asthmatics should take an anti-inflammatory, either together with a reliever during attacks (step 1) or as a controller daily (steps 2 – 5).
The first choice is inhaled corticosteroids. Oral corticosteroids, leukotriene antagonists and biological therapy are secondary options. Biological therapy is expensive and should be reserved for severe cases.
Mechanism of action:
Corticosteroids have many inflammatory actions. The one which is most relevant for asthma is that they reduce the transcription of IL-2, a cytokine which stimulates Th2 cells, which are important in asthma. Steroids also decrease the formation of cytokines which reqruit eosinophils and promote IgE production. They also upregulate β2 receptors, thereby increasing the effect of LABAs and SABAs.
Recall from topic 23 that leukotrienes cause bronchoconstriction, bronchial swelling and increased mucus secretion, so inhibiting their action will obviously have a beneficial effect on asthma. Leukotrienes also attract neutrophils, so inhibiting them will reduce inflammation as well. Zafirlukast and montelukast are competitive antagonists for the CysLT1 leukotriene receptor.
The biological agents bind to and inactivate various cytokines and receptors which are involved in the pathogenesis of asthma.
Pharmacokinetics:
Leukotriene antagonists are taken orally. Biological agents are injected subcutaneously.
Adverse effects:
Serious adverse effects are uncommon with inhaled steroids. Side effects like oral fungal infection can be prevented by rinsing the mouth with water after inhalation.
- Oral corticosteroids
- Glaucoma
- Cataract
- Hypertension
- Osteoporosis
- Diabetes
- Leukotriene antagonists
- Elevated liver function tests
- Biological therapy
- Few side effects
Treatment of acute asthma attacks
- Mild attack
- Inhaled SABA
- Terbutaline
- Salbutamol
- Inhaled SABA
- Moderate attack
- Inhaled SABA
- Corticosteroid p.o. or i.v.
- Prednisolone
- Methylprednisolone
- Severe attack
- Inhaled oxygen
- Inhaled SABA + ipratropium
- Corticosteroid i.v.
Treatment of COPD
Chronic obstructive pulmonary disorder (COPD) is characterised by chronic obstruction and acute exacerbations.
People with COPD is classified into different patient groups according to the GOLD system, where GOLD A has the fewest symptoms and exacerbations and GOLD D has the most. The treatment depends on the GOLD group the patient is in.
The following drugs are important in the treatment of COPD:
- β2-agonists
- Short-acting β2-agonists
- Salbutamol
- Fenoterol
- Long-acting β2-agonists
- Salmeterol
- Formoterol
- Short-acting β2-agonists
- Muscarinic antagonists
- Tiotropium (long-acting)
- Ipratropium (short-acting)
- Corticosteroids
- Inhaled
- Budesonide
- Fluticasone
- Oral
- Prednisone
- Prednisolone
- Methylprednisolone
- Inhaled
- PDE4 inhibitors
- Roflumilast
- Antibiotics
- Penicillin G
- Ampicillin
Indications:
Short-acting bronchodilators like SABAs and ipratropium are used to treat acute exacerbations. Oral or IV steroids are used in severe cases. Antibiotics should be given if there are signs of infections and should cover Haemophilus influenzae and Streptococcus pneumoniae.
Long-acting bronchodilators are used in the maintanence treatment of COPD. An inhaled corticosteroid may be added if GOLD C or GOLD D.
Roflumilast is a new drug which is given orally and can be used in GOLD D.
Mechanism of action:
Roflumilast is a PDE4 inhibitor. It decreases the inflammation associated with COPD.
Nikolas, This article you have written has saved my life. I’ve had periodic bronchial asthma for years and had been prescribed all sorts of asthma medication. It was confusing which ones to use when and did not understand it until you spelled it out in this article. I have been coughing almost non stop for a month. I was taking Ipratropium Bromide with Albuterol sulfate in a nebulizer treatment 3 – 4 x daily. I finally asked my dr for Advair ( fluticasone and salmeterol) but still was not having success in controlling my coughing. I also had Azelastine for a nose spray. Everytime I talked I coughed. I coughed when I slept. I am 63 and after a month of this I felt I was tired and losing this battle. I have been so afraid of getting Covid that I only did telemedicine with my family dr, I couldn’t get in to see a pulmonologist until mid June. I goggled medication for Bronchial asthma and found your article. I stopped the nose spray ( it made me gag) and asked my dr if I could add tiotropium ( Spiriva) that I already had in my arsenal of medications. He said yes, and I have enjoyed the relief of not coughing constantly. It’s only because of your great article that I found the right combination. I want to print out your article . Can you email it to me in a pdf file? I want keep it for a reference because I know I’ll forget some of it. I want to sincerely thank you for giving me my life back. I’m sleeping better and gaining my energy back. Thank you Nikolas.
Dear Marilyn
I’m glad you’re feeling much better. I’m sorry that you had to do your own research to find a working combination, that should obviously have been your physicians job.
You can convert any webpage to pdf by right clicking anywhere on the webpage, selecting “print” and then selecting “print to pdf”. A pdf version of the page will be made.
I wish you good health!
Nice read, I just passed this onto a colleague who was doing some research on that. And he just bought me lunch since I found it for him smile Therefore let me rephrase that: Thank you for lunch!
Glad that drugs used to treat bronchial asthma provided you lunch
hi nick ,
is it budenoside or budesonide?
It’s fixed