Page created on September 18, 2019. Last updated on December 18, 2024 at 16:57
Introduction to β-lactam antibiotics
The beta lactam antibiotics is a class of antibiotics that all contain a so-called beta lactam ring, shown in red below.
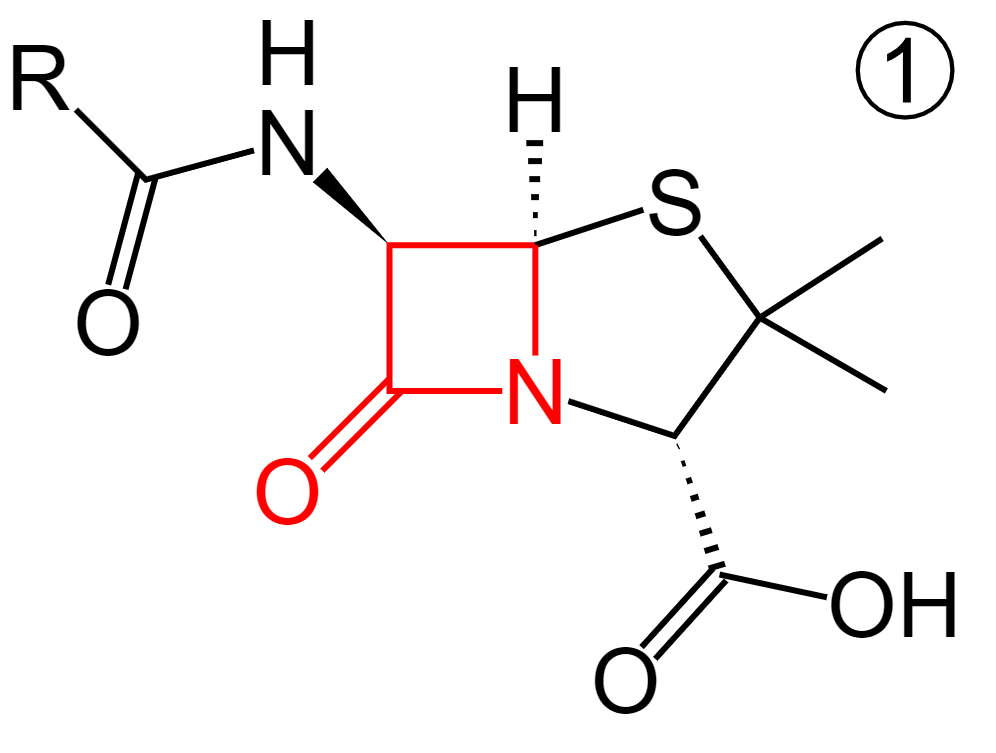
The structure of penicillin, with the beta lactam ring in red. From https://en.wikipedia.org/wiki/%CE%92-lactam_antibiotic
All beta lactam antibiotics interfere with the synthesis of the bacterial cell wall peptidoglycan. They bind covalently to a protein called penicillin-binding protein (PBP) and inhibits its function. PBP is an enzyme which is essential for the synthesis of peptidoglycans, by crosslinking peptidoglycans. This causes the cell wall to be weakened, eventually causing the cells to lyse.
Many bacteria produce beta-lactamases, a type of enzyme which cleaves the beta lactam ring of beta lactam antibiotics, thereby inactivating the antibiotic.
Four types of antibiotics are beta lactams, the penicillins, cephalosporins, carbapenems and monobactams.
Penicillins
The first penicillins (penicillin G and penicillin V) were isolated from a mould called penicillium (by Alexander Fleming), which produces the aforementioned penicillins. Penicillin G, also called benzylpenicillin, is poorly absorbed by the GI tract and is inactivated by bacterial beta-lactamases. Penicillin V has good oral bioavailability and can be given by mouth. Despite these drawbacks penicillin G and V still has some uses today.
Nowadays we have many other types of penicillin, all of them semisynthetic. These other types lack some of the drawbacks of the basic (natural) penicillins (G and V). The four main types of penicillins are:
- Basic penicillins
- Penicillin G
- Penicillin V
- Penicillinase resistant (antistaphylococcal) penicillins
- Methicillin
- Nafcillin
- Oxacillin
- Cloxacillin
- Dicloxacillin
- Flucloxacillin
- Aminopenicillins (broad spectrum penicillins)
- Ampicillin
- Amoxicillin
- Antipseudomonal (ultra-broad spectrum) penicillins
- Carboxypenicillins
- Carbenicillin
- Ticarcillin
- Ureidopenicillins
- Mezlocillin
- Piperacillin
- Carboxypenicillins
Methods of resistance:
Some bacteria produce penicillinase, a type of beta-lactamase which is specific for penicillins. This enzyme cleaves the beta lactam ring and inactivates the antibiotic.
Some bacteria have mutated penicillin-binding proteins which have lower affinity for penicillins than normal PBPs. This causes them to be resistant to penicillins.
Some Gram-negative bacteria have outer membrane proteins that prevent penicillins from entering the bacterial cell.
Penicillinase-resistant penicillins:
Like the name suggests these antibiotics are effective even against bacteria that produce penicillinase. Like the alternative name suggests (antistaphylococcal), these penicillins are often preferred for methicillin-sensitive staphylococcus aureus (MSSA). Methicillin was the first of this class but is no longer used as it caused interstitial nephritis. Its name is still remembered however as part of the methicillin resistant staphylococcus aureus (MRSA). In Europe cloxacillin, dicloxacillin and flucloxacillin are the most used.
These antibiotics have less antimicrobial activity than the basic penicillins and should therefore only be used when there is resistance against the basic ones.
Aminopenicillins:
Aminopenicillins themselves are sensitive to penicillinase, but they’re almost always combined with so-called beta-lactamase inhibitors. Ampicillin is combined with the beta-lactamase inhibitor sulbactam while amoxicillin is combined with clavulanate (clavulanic acid). The combination amoxicillin+clavulanate is called Augmentin®.
The aminopenicillins have a broader antimicrobial spectrum than the basic and penicillinase-resistant penicillins.
Antipseudomonal penicillins:
Like the name suggests these penicillins are effective against pseudomonas aeruginosa. Only piperacillin and ticarcillin are in widespread use.
These drugs are sensitive to penicillinase and are therefore, like aminopenicillins, often combined with beta-lactamase inhibitors. Ticarcillin is combined with clavulanate and piperacillin is combined with tazobactam.
Pharmacokinetics and dosing:
Penicillin G and piperacillin are acid labile and therefore only available as parenteral preparations, mostly IV. Penicillin G is also available as a slow-release intramuscular injection, given once per day. The dosing for penicillin G should be 5 – 20 million international units (IU) per day.
Penicillin V, oxacillin, cloxacillin, dicloxacillin, flucloxacillin, ampicillin and amoxicillin are all acid stable and therefore available as oral preparations.
Penicillins are well distributed in the extracellular space but penetrate poorly into the intracellular space, prostate and eyes. It penetrates very poorly into the CNS, except during meningitis, which is the only case where we can reach therapeutic concentrations in the CSF.
Most penicillins are eliminated unchanged by tubular secretion. Broad spectrum penicillins are partially excreted in the bile, too.
Penicillins have a short half-life, around 0,5 – 1 hour so for maximum effect they should be administered at 6-hour intervals, four times a day.
Side effects:
The most important side effect of penicillins is hypersensitivity; penicillin allergy is common. Penicillins can act as haptens and induce anaphylaxis, bronchospasm, interstitial nephritis etc. High doses can cause convulsions.
As is common for most antibiotics are gastrointestinal symptoms like diarrhoea and nausea common. Skin rashes and fever are also common.
Antibiotic spectrum:
The following list is not exhaustive and merely shows which bacteria the antibiotics are first choices.
- Penicillin G/V
- Neisseria meningitidis
- Clostridia
- Treponema pallidum
- Streptococcus pyogenes
- Penicillinase-resistant penicillins
- Methicillin-sensitive staphylococcus aureus
- Aminopenicillins
- Streptococcus pneumoniae
- Salmonella
- Shigella
- Enterococci
- Antipseudomonal penicillins
- Gram negatives
- Pseudomonas aeruginosa
- Klebsiella
Cephalosporins
Cephalosporins are beta lactam antibiotics originally derived from the fungus cephalosporium. Most cephalosporins are semisynthetic compounds. These drugs have the same mechanism of action as penicillins. They’re divided into generations from 1 – 5 and whether they’re used parenterally or orally. The following are the most important ones.
|
1. generation |
2. generation | 3. generation | 4. generation |
5. generation |
|
| Parenteral |
Cefalotin Cefazoline |
Cefuroxime | Cefotaxime
Ceftazidime Ceftriaxone |
Cefepime |
Ceftaroline Ceftobiprol |
| Oral |
Cefalexin |
Cefaclor |
Cefixime |
Methods of resistance:
Almost all Gram-negative bacteria produce a beta-lactamase which inactivates many cephalosporins (but not penicillins). Resistance can also develop due to outer membrane proteins that prevent cephalosporins from entering the bacterial cell.
Pharmacokinetics:
The first and second generation don’t penetrate the CNS well, but the other generations do.
Most cephalosporins are eliminated unchanged via tubular secretion in the kidneys. Their half-life is 1 – 2 hours.
Ceftriaxone stands out for these reasons:
- it is excreted into bile
- it binds strongly to albumin and can therefore displace other drugs which do the same.
- it has a half-life of 6 – 8 hours.
Side effects:
As with penicillins hypersensitivity reactions can develop. In 5 – 7% of cases there is cross-sensitivity between them, meaning that 5 – 7% of people with penicillin allergy will be allergic to cephalosporins as well.
Gastrointestinal symptoms are common. If given together with aminoglycosides they can cause nephrotoxicity. Some cephalosporins (none of the most widely used, though) have a disulfiram-like effect and can cause symptoms when taken with alcohol. Some have a coumarin-like effect.
Clinical uses:
1. generation: Cefazoline is used as perioperative prophylaxis.
2. generation: Upper and lower respiratory tract infections.
3. generation: Urinary tract and respiratory tract infections (including nosocomial), meningitis, gonorrhoea, pseudomonas
4. generation: Same as for 3. generation, used in case of severe infections or resistance to 3. generation.
5. generation: MRSA.
Hey!
Just wanted to say that I’m not sure the part about beta-lactamase production as the mechanism of resistance for cephalosporins is correct.
According to sketchy, beta-lactamases are ineffective against cephalosporins and according to Wikipedia the mechanism of resistance is “either reduced affinity of existing PBP components or the acquisition of a supplementary β-lactam-insensitive PBP.”
Good luck with the continued studying and as always, thanks for the work you do! 😀
Your theory contradicts both the book and the seminar.