Page created on March 7, 2018. Last updated on December 18, 2024 at 16:55
Activating the immune system eventually causes an inflammatory reaction, but how is it activated? Pathogens enters the body through an epithelial surface and are then taken up by blood or lymph. If taken up by blood, the blood will eventually reach the spleen, where erythrocytes meet leukocytes, so the leukocytes can recognize an antigen on the pathogen to start the immune reaction. If the pathogen is taken up by lymph, it will travel to a secondary lymphoid organ, most likely a lymph node, where it will also meet leukocytes.
After the naïve (not-yet activated) lymphocytes are activated, adaptive immune responses are initiated. These activated immune cells can then migrate to the site of infection and do their work to eliminate the pathogen.
When a piece of tissue gets damaged or infected, like by a cut, there will be a local inflammation. This is an immediate reaction whose role is to inhibit spreading of infection and further injury. It is characterized by redness, hotness, painfulness and swelling. It’s composed of 3 main events. Vasodilation occurs in minutes, increased capillary permeability gives oedema, and lastly, phagocytes will migrate to the tissue after a few hours.
Many molecules mediate inflammation. They can be divided into two groups: the ones found in blood plasma, and the ones produced by cells. Belonging to the first group are the acute-phase proteins, the kinin system, the fibrinolytic system and the complement system. Belonging to the second group are histamine, platelet-activating factor, inflammatory cytokines like IL-1, IL-6 and TNF-α, and other molecules like NO and reactive oxygen species.
When there is tissue damage, there is endothelial damage (vessels are everywhere). When vessels break, clots formed from fibrin are formed. The size of these clots is regulated by an enzyme called plasmin, which breaks down part of the fibrin clot should it become too large. The fragments of fibrin that are cut off help mediate the local inflammation. The endothelial damage also induces the production of a protein called bradykinin, a strong vasodilator, through the kinin system.
Macrophages
- Macrophages are present in most tissues. They are also important in case of local inflammation. Macrophages in the tissue are in the resting phase until activated by binding to LPS on the surface of a bacteria. They then enter the activated phase, where they phagocyte the bacteria, so they can present its antigens to CD4+ T-cells and other cells. The macrophages also increase the expression of MHCII to increase their antigen presentation. During the activated phase, the macrophages also produce inflammatory cytokines like IL-1, IL-6 and TNF-α. After the macrophage has received a signal consisting of IFN-γ, it will enter the hyperactivated stage. During this stage, MHCII expression will be reduced, because the need for antigen presenting has diminished, and the cell will instead focus on cytotoxicity. This is the classical activation pathway.
The inflammatory cytokines have different effects. They all contribute to fever systemically, but they all have both local and systemic effects. IL-1 activates the lymphocytes and endothelial cells locally, while increasing IL-6 production in the whole body. IL-6 also activates lymphocytes locally, but also increases antibody production. It also induces production of acute-phase proteins. TNF-α activates the endothelium and increases its permeability to allow cells to pass it. IL-1, TNF-α and a protein called C5a all cause nearby endothelium to express adhesion molecules called selectins, the reason for which we will see soon.
I mentioned the classical activation pathway of macrophages earlier. The alternative activation pathway is involved when the macrophage should be activated for duties not related to a pathogen, such as wound repair, fibrosis, and anti-inflammatory effects. Instead of being activated by IFN-γ, the macrophage gets activated by IL-13 and IL-14. This causes the macrophage to secrete IL-10 and TGF-β which have anti-inflammatory effects. The macrophage will also start wound repair and fibrosis.
Leukocyte migration to tissues
For the immune response to be effective, leukocytes must be able to migrate to both tissues, to negate the threat, and to secondary lymphoid tissues, to get activated. Each leukocyte circulates only 1 or 2 times each day, so being able to enter the infected tissue when the cell first passes it is very important.
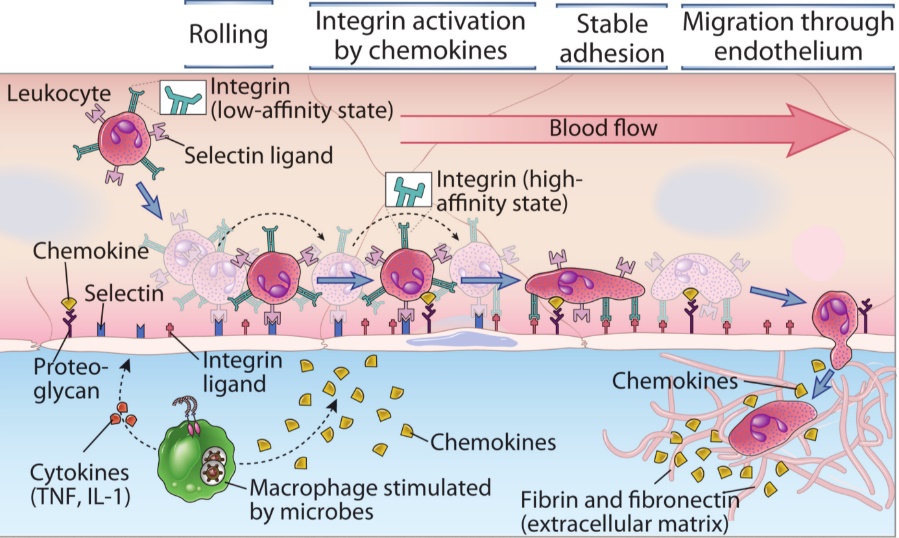
After a leukocyte targeting the infected tissue has entered a blood vessel close to the tissue, it will start “rolling” on the endothelial surface. This rolling happens because the leukocytes have ligands on their cell surface that bind loosely to selectin receptors on the endothelium. However, since the binding is loose, they’re not kept in place but allowed to roll, like rolling something on Velcro (google it).
After rolling some distance, they are exposed to molecules called chemokines secreted by macrophages in the infected tissue. The chemokines activate the integrin-receptors on the leukocytes from a low-affinity state to a high-affinity state. These integrin receptors bind to ligands on the endothelium more strongly than the selectin-receptors, which allows the leukocyte to stop rolling and stay in place.
Now that they are in place, the cytoskeleton of the leukocyte begins to change the shape of it from round to flat. They then pass through the small gaps between endothelial cells with the help of PECAM proteins on both the leukocyte and endothelial cell surface that effectively “pull” the leukocyte through the gap. The leukocyte then breaks through the basement membrane by unknown mechanisms, before it finds itself in the extracellular space.
The acute phase reaction (= systemic inflammation)
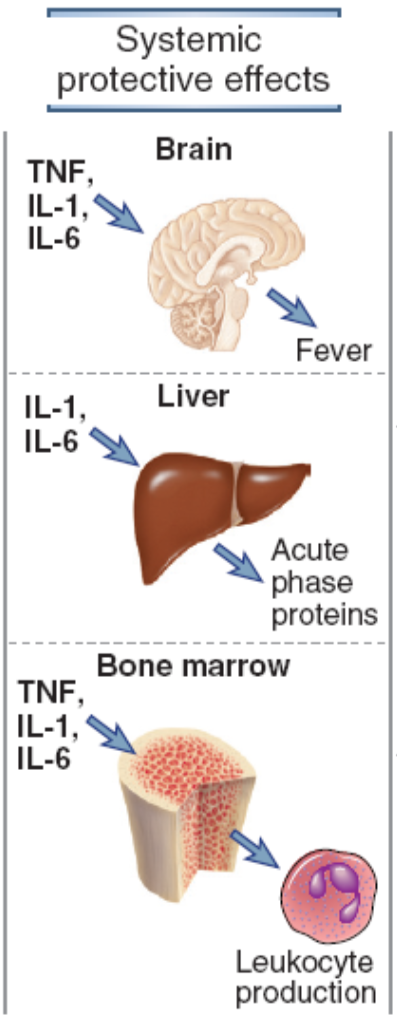
We all know the symptoms of systemic inflammation: it’s the feeling of sickness. The systemic acute inflammation is a cascade started by the production of cytokines like TNF-α, IL-1 and IL-6 by the macrophages and dendritic cells in the locally inflamed tissue where infection or injury started.. These cytokines signal the brain to produce prostaglandins which increase body temperature (fever), and to decrease appetite (anorexia). They also signal to the bone marrow to increase production of certain leukocytes, depending on the infection. If it’s a viral infection, there will be lymphocytosis (increased lymphocytes). If there is a bacterial infection, there will be neutrophilia (increased number of neutrophils). If there’s an allergic reaction, there will be eosinophilia. Some of the cytokines produced, especially IL-6, will cause the liver to start synthesizing certain proteins.
These acute phase proteins are C-reactive protein (CRP), serum amyloid A, fibrinogen, mannose binding lectin and complement system components. CRP opsonizes bacteria by binding to phosphocholine on their surface. Serum amyloid A recruits immune cells to inflammatory sites and induces enzymes that breaks down ECM. Mannose binding lectin activates the complement system through the lectin pathway, a topic for later. The increase of proteins in the blood will increase the erythrocyte sedimentation rate, which can be used for diagnostics.
Hello. I see that you don’t update your page too often. I know that writing content is time consuming and boring.
But did you know that there is a tool that allows you to create new articles using existing content
(from article directories or other blogs from your niche)? And
it does it very well. The new articles are unique
and pass the copyscape test. Search in google and try: [REMOVED]
tools
nice