Page created on October 22, 2018. Last updated on October 18, 2021 at 18:31
Oedema is fluid accumulations within the interstitial spaces or anatomical body cavities.
We distinguish between two types based on their content. Transudate is a protein-poor oedema, similar to interstitial fluid and appears to e.g. increased hydrostatic pressure. Exudate is however a protein-rich oedema that comes with inflammation.
When talking about oedema, it’s important to have the nomenclature right.
- Anasarca – severe subcutaneous oedema
- Effusion – excessive fluid in body cavity
- Hydrothorax – Pleural effusion
- Hydropericardium – Pericardial effusion
- Ascites – Peritoneal effusion
- Hydrokele – excessive fluid between layers of tunica vaginalis
- Hydrosalpinx – Fluid in fallopian tube
- Hydronephrosis – Fluid accumulation in renal pelvis
- Hydrops vesicae felleae – Fluid in gallbladder
- Myxooedema – dermal and subcutaneous oedema
Pathomechanism
The Starling’s Equation shows us the relationship between the forces which holds the fluid inside the capillaries. We studied this in physiology as well, so it’s a good thing that it’s not completely new.
![]()
where
- Jv = fluid movement. If bigger than 0, the fluid will enter interstitum.
- Kf = Capillary permeability coefficient
- Pc = Capillary hydrostatic pressure. It tries to push the fluid out of the capillary
- Pi = Interstitial hydrostatic pressure. Pushes against the fluid in the capillary.
- πc = Capillary oncotic/colloid pressure. Holds back the fluid in the capillary.
- πi = Interstitial oncotic/colloid pressure. Pulls out the fluid from the capillary.
- σ = Reflection coefficient. Specific to a certain capillary’s permeability to a certain solute
To make it easier, the capillary and interstitial spaces are governed by two opposing forces, the capillary hydrostatic pressure (P) and the oncotic pressure (π). The oncotic pressure is produced by plasma proteins. Less protein in plasma accounts for less forces that tries to hold back the fluid in the capillaries.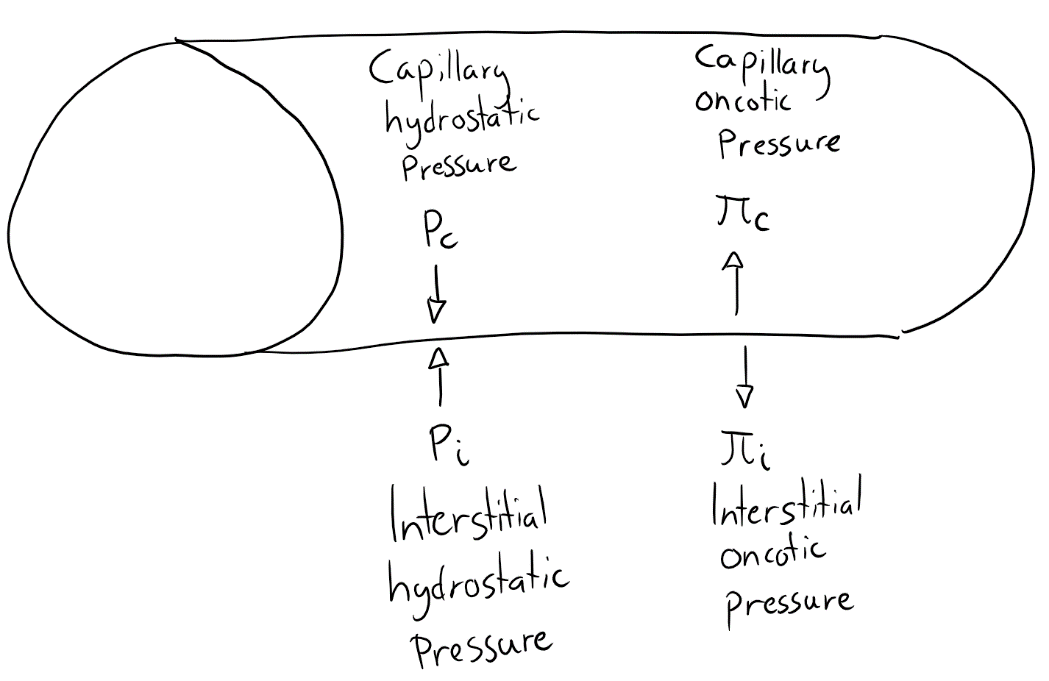
These forces are normally balanced, with a slightly elevated hydrostatic pressure at the arteriolar ends, making some fluid leak out of the capillaries, and a slightly elevated oncotic pressure at the venular end, sucking in some of the leaked fluid. The little amount left is then removed by lymphatic drainage. However, if the leakage is too big, the capacity of the lymphatic drainage exceeds, and the result will be an oedema.
Let’s look at some causes for this
Increased hydrostatic pressure can result from impaired venous return and congestive heart failure. The heart failure will result in reduced cardiac output, that will activate the renin-angiotensin-aldosterone system because the kidneys think the blood pressure is low. RAAS will, as we know, lead to sodium and water retention, making the blood volume increase, but since the heart is failing, it really can’t improve the cardiac output. This increase in blood volume will result in an increased hydrostatic pressure and oedema.
Also, local impaired venous return due to a thrombosis can cause oedema.
Reduced oncotic pressure in plasma can also lead to oedema. Albumin accounts almost for the half of the total plasma proteins, and conditions where albumin is either lost or not synthetized enough leads to oedema. This happens in:
- Nephrotic syndrome where glomerular capillaries allow proteins to pass, leading to proteinuria (protein in urine).
- Protein malnutrition
- Severe liver diseases as cirrhosis where no albumin is produced
Impaired lymphatic drainage and lymphoedema results often from local obstruction either caused by infections or neoplastic conditions (cancer). Filariasis is an infection that causes big oedemas of the lower extremities and external genitalia. Breast cancer can give an oedema of the overlying skin.
Elephantiasis is the known condition of elephant legs and is a severe form of lymphoedema.
Renal failure will lead to an increased salt and water retention, as discussed earlier. This condition will also increase the hydrostatic pressure.
Inflammation increases the permeability of capillaries by increasing the Kf (permeability coefficient).
Clinical forms
(see also pathophysiology topic 10. Pathophysiology of the lymphatic circulation)
1. Cardiac oedema
Often due to congestive heart failure.
This often leads to a type of subcutaneous oedema called pitting oedema. Pitting oedema is when you press on the oedema with one finger and there will be a finger-shaped depression. Another subcutaneous oedema is anasarca. However, cardiac condition can also lead to pleural effusions, ascites and pulmonary oedema. The latter one is often due to left ventricular failure but can also occur in renal failure.
2. Pulmonary oedema
Lungs fills up with fluid causing them to be 2-3 heavier than their normal weight.
3. Renal oedema
Like in nephrotic syndrome, there will be a loss to proteins because of proteinuria, as discussed earlier. This type of oedema manifests first in loose connective tissue, like the eyelids, giving preorbital oedema.
4. Hepatic oedema
As discussed earlier, hypoproteinaemia due to impaired albumin synthesis. Also, hepatic hypertension may lead to increased hydrostatic pressure.
5. Protein losing enteropathies
Malabsorption as in Celiac disease (gluten is a protein y’all), Crohn’s Disease (S/O to Greek doctors’ bowels) leads to hypoproteinaemia.
Menetrier’s disease is a condition where the mucosal wall of the stomach is thickened, and less stomach acid is produced, leading to decreased absorption of proteins.
6. Lymphoedema
Also discussed earlier but happens also after operations and irradiation. It happens in particular after mammectomy, because in this procedure lymph nodes are also removed, which impairs the lymphatic filtration.
7. Inflammatory oedema
Allergic reactions causing a rapid oedema of dermis, subcutis and mucosa. Inflammatory mediators such as bradykinin will lead to vasodilation and increased permeability.
8. Cerebral oedema
This type of oedema is life threatening and can lead to herniations. There are three types of cerebral oedema.
-
- Cytotoxic oedema where the cells swell.
- Vasogenic oedema where the blood-brain barrier is damaged.
- Interstitial oedema where the CSF is leaking into the tissue.
Types of herniations:
-
- Cingular herniation where the falx compresses cingulate gyrus.
- Uncal herniation where tentorium compresses the uncus of temporal lobe
- Tonsillar herniation where foramen magnum compresses cerebellar tonsils and brain stem.
Hello greek!
What does the sigma(?) mean in the equation? As a few sources online don’t mention it
Added an explanation (probably not important for exam)
Du er pus <3
hello mithir