Table of Contents
Page created on November 2, 2018. Last updated on December 18, 2024 at 16:56
Coronary artery disease/ischaemic heart disease
Coronary artery disease (CAD) or ischaemic heart disease (IHD) is a group of diseases that is caused by a mismatch between myocardial oxygen supply and oxygen demand, which causes ischaemia of the myocardium. In almost all cases it’s caused by atherosclerosis in the coronaries.
The following conditions are considered coronary artery diseases:
- Stable angina
- Silent myocardial ischaemia
- Chronic ischaemic heart disease
- Acute coronary syndromes
- Acute myocardial infarction (AMI)
- ST-elevated myocardial infarction (STEMI)
- Non-ST-elevated myocardial infarction (NSTEMI)
- Unstable angina
- Sudden cardiac death
- Acute myocardial infarction (AMI)
Coronary artery disease is by far the most common cause for these conditions, but they’re not the only cause for them. For example can a myocardial infarction be caused by coronary spasm or coronary dissection as well, however these are rare occurrences.
The risk factors for coronary artery disease are the same as for atherosclerosis.
Acute coronary syndrome
Acute coronary syndrome (ACS) is an umbrella term for three conditions: ST-elevated myocardial infarction (STEMI), non-ST-elevated myocardial infarction (NSTEMI) and unstable angina. As the name implies they’re acute diseases caused by abnormalities of the coronaries.
The differential diagnosis of acute coronary syndrome is simple. They all present with the special chest pain called angina pectoris. Angina pectoris is a pressing or strangling type of chest pain. If troponin levels in the blood increases has an infarction occurred. The infarct can occur either with or without ST elevation. If there was angina pectoris pain but the troponin levels are normal has an episode of unstable angina occurred.
The most common cause of ACS is coronary artery disease.
Acute myocardial infarction and unstable angina
Acute myocardial infarction (AMI) usually develops after an atherosclerotic plaque ruptures or breaks open. The exposed inner surface of the plaque is highly thrombogenic, meaning that platelets very easily bind to it and form a thrombus. The growing thrombus can partially or completely occlude the artery, which causes ischaemia of the supplied part of the myocardium.
A rupturing plaque is the most common cause for AMI, however other causes exist. Any state where the myocardial oxygen demand is much higher than the oxygen supply can cause an infarct, like anaemia, hyperthyroidism, coronary spasm or coronary embolism.
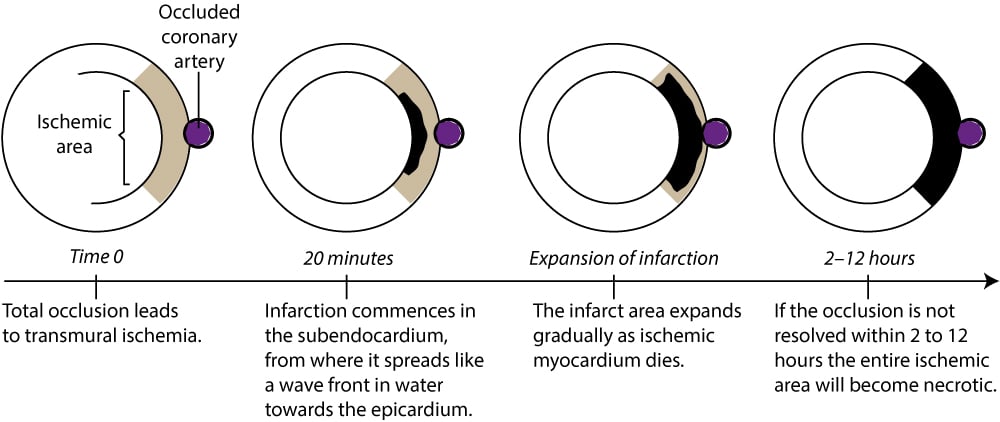
The subendocardial part of the myocardium is the least perfused part of the myocardium. This is because the coronary artery supply lies on the epicardium, meaning that the subendocardial myocardium is farthest away from the blood supply.
If the occlusion was complete will the necrosis not only affect the subendocardium but the whole wall, making the ischaemia transmural. This causes ST-elevated infarcts (STEMIs).
If the coronary artery is only partially occluded (but more than 70%) will the ischaemia occur only in the least perfused part, the subendocardial part. This is what leads to non-ST-elevated infarcts (NSTEMIs) and unstable anginas.
The difference between unstable angina and NSTEMIs is that there is no necrosis in unstable angina, just ischaemia. This is because in case of unstable angina will the occlusion resolve before the ischaemia has had time to cause irreversible injury to the myocardium. It takes approximately 25-30 minutes of ischaemia to cause infarction.
Diagnosis of myocardial infarct is based on multiple criteria. In addition to elevated troponin levels in the blood can ECG changes, changes in the motion of the heart wall or finding a thrombus in the coronaries with an angiogram be seen.
The risk for developing acute coronary syndrome increases in the morning. It probably has a connection to how the sympathetic nervous system activates in the morning, which can increase the blood pressure and increase the forces that can rupture a plaque. Coagulability is also higher in the morning, which may also play a role.
Consequences of myocardial ischaemia
Angina pectoris occurs around 30 seconds after ischaemia has occurred. If coronary flow isn’t restored in 25-30 minutes the myocardial infarction will start. The infarct starts in the subendocardium and moves like a wave front as the it spreads from the subendocardium toward the subepicardium.
The surface of injured myocardial fibres is more (electrically) negative than the healthy fibres. This creates a so-called current of injury which is what causes the ST changes on the ECG. It also sets the stage for electrical dysfunctions like re-entry, arrhythmias and ventricular fibrillation.
The myocardium that is affected by ischaemia is doesn’t contract correctly or at all. The areas around the affected myocardium can partly compensate for this.
While we can prove that irreversible damage occurs after 25-30 minutes of ischaemia can we not see any histological signs of damage until a few hours after.
After 45 minutes will a quarter of the wall be necrotized, after 3 hours half of the wall, after 6 hours three quarters and within 24 hours will the whole wall be necrotized.
The damaged cells release potassium, causing a local hyperkalaemia. This hyperkalaemia gives rise to the peaked tall T-wave on the ECG. Enzymes and myocardial components are also released from the damaged cells, like creatine kinase, troponin T, troponin C and myoglobin. The presence of troponins in the blood is diagnostic for acute myocardial infarction.
Acute myocardial infarction has many potentially lethal complications:
- Ventricular fibrillation
- Cardiogenic shock
- Ventricular wall rupture leading to cardiac tamponade
- Papillary muscle rupture
- Ventricular wall thrombus
Treatment of acute coronary syndrome
The gold standard for treating acute coronary syndrome is a procedure called Percutaneous Coronary Intervention (PCI). It’s a non-invasive procedure where a balloon catheter is inserted into the femoral or radial artery and guided to the coronaries. When the physician has identified the occluded artery by angiogram can they inflate the balloon to dilate the vessel. Stents can be placed in the artery to keep it open after the procedure.
Thrombolytic therapy can also be performed to break up the blood clot that occludes the coronary.