Table of Contents
Page created on January 4, 2020. Last updated on December 18, 2024 at 16:57
Before you begin, keep one thing in mind: They will fail you instantly if you don’t know the FULL name of the organism which causes the infectious disease. People have failed because they’d forgotten what the “E” in E. Coli stands for, and for forgetting the name of the organism which causes cholera. Make sure you know all organism names in full.
1. Role of nutrition in prevention of cardiovascular diseases
- Cardiovascular disease = CVD
- Ischaemic heart disease
- Stroke
- Epidemiology of cardiovascular disease
- CVD is the leading cause of death in the world
- Risk factors for CVD
- Behavioural (modifiable)
- Behavioural risk factors are responsible for about 80% of CVD
- Unhealthy diet
- Physical inactivity
- Tobacco use
- Harmful use of alcohol
- Non-modifiable
- Family history
- Old age
- Behavioural (modifiable)
- 2018 study in British Medical Journal (BMJ):
- Healthy dietary patterns can decrease the effect of genetic factors that would otherwise predispose to obesity.
- Also, improved diet quality had a more significant effect on people with high genetic risk for obesity.
- 2012 Cochrane review:
- Reducing saturated fat in diet decreases risk for cardiovascular disease by 14%
- 2014 study in BMJ:
- Replacing saturated fat in diet with polyunsaturated fat did not decrease risk for cardiovascular disease (later studies contradict this, but those studies are not mentioned in the lecture)
- Oslo diet heart study:
- Diet low in saturated fat, cholesterol and high in polyunsaturated fat -> reduced serum cholesterol, reduced cardiovascular disease
- Lyon diet heart study:
- Diet low in saturated fat, high in unsaturated fat -> reduced cardiovascular mortality
- Stanford coronary risk intervention project (SCRIP):
- Low fat, saturated fat, cholesterol diet + exercise -> decreased dyslipidaemia, decreased cardiovascular disease
Cardiometabolic risk
- The risk for developing diabetes, heart disease or stroke (basically metabolic syndrome)
- The risk factors for atherosclerosis, obesity, and cardiovascular disease are all the same or very similar
- Risk factors:
- Hypertension
- Inflammation
- Age
- Race
- Gender
- Family history
- Dyslipidaemia
- Overweight
- Insulin resistance
- Smoking
- Physical inactivity
- Unhealthy eating
Benefits of fish oils:
- Fish oils contain omega-3 (n-3, ω-3) polyunsaturated fatty acids (PUFAs)
- DART trial: Men with cardiovascular disease who increased intake of fish or used fish oil tablets had reduced cardiovascular mortality
- GISSI trial: Men and women with cardiovascular disease who took 1 g omega-3 daily decreased the number of cardiovascular events
Other nutrients
- Nurses health study:
- Increased nut intake -> decreased risk for cardiovascular events
- PREDIMED study:
- Increased nut intake -> decreased cardiovascular mortality
- Zhaoli meta-analysis:
- Increased soy intake -> decreased cardiovascular risk
- Phytosterol-supplemented foods intake -> decreased LDL-cholesterol
- Increased intake of garlic -> decreased total cholesterol
Recent changes in the view of associated between diet and cardiovascular disease
- Dietary cholesterol is not the major determinant of blood cholesterol
- Individual nutrients may not be responsible for risk, but rather complex foods
- Example: Increased consumption of fish is better than omega-3 fat supplementation
Vitamin D
- High serum vitamin D concentration -> decreased cardiovascular events
- Hypovitaminosis D leads to:
- Decreased anti-inflammatory cytokines
- Increased pro-inflammatory cytokines
- Increased inflammation -> increased atherosclerosis
- Increased angiotensin II activity -> increased myocardial remodelling
- Increased insulin resistance
Therapeutic lifestyle changes (TLC) in LDL-lowering therapy:
| Nutrients | Recommended intake |
| Saturated fat | < 7% of total calories |
| Polyunsaturated fat | < 10% of total calories |
| Monounsaturated fat | < 20% of total calories |
| Total fat | 25 – 35% of total calories |
| Carbohydrate | 50 – 60% of total calories |
| Fibre | 20 – 30g daily |
| Protein | 15% of total calories |
| Cholesterol | < 200mg/day |
| Total calories | Balanced so that body weight is stable or reached desirable levels |
- TLC can reduce LDL levels by 20 – 30%
Summary:
- Reducing LDL levels is beneficial for preventing cardiovascular disease or events
- Decreased saturated fat intake
- Decreased total fat intake
- Decreased trans fat intake
- Increase unsaturated fat intake
- Increased fibre intake
- Sufficient vitamin D intake
- Increased fish consumption
- Decreased weight
- Increased intake of plant sterols
- Decreased dietary cholesterol
- Increased physical activtiy
- See also Mediterranean diet, DASH diet
2. Role of nutrition in prevention of cancers
- 35% of cancer cases are related to nutrition
- 30% of cancer cases are related to smoking
- 10% of cancer cases are related to infecitons
- Nutrition is the most important behavioural risk factor for cancer – more than smoking, infections
β-carotene supplementation and cancer:
- β-carotene can be either an antioxidant or a pro-oxidant, depending on these factors
- Concentration
- Presence of other pro-oxidant or antioxidant compounds
- Oxygen concentration
- It was thought that β-carotene supplementation in smokers could decrease risk of lung cancer, but it actually increased the risk
- ATBC – huge study in Finland -> daily β-carotene supplementation increased risk for lung cancer in smokers
- CARET – huge study in USA -> daily β-carotene supplementation increased risk for lung cancer in smokers
Tea and cancer
- Green tea consumption decreased risk of oesophageal cancer
- Study: People who drank hotter tea in Iran -> increased risk for oesophageal cancer
Energy intake and cancer
- Underfeeding (energy restriction) -> decreased risk of cancer
- Overfeeding (obesity) -> increased risk of cancer
- Possible mechanisms of increased cancer risk
- Increased insulin and IGF-1
- These hormones stimulate cell proliferation and inhibit apoptosis
- Increased oestrogen
- Increased leptin
- Increased inflammatory cytokines
- Increased oxidative stress
- Decreased DNA repair capacity
- Increased insulin and IGF-1
Fat intake and cancer
- Saturated fat, trans fat and omega-6 fats increase risk for cancer
- Omega-6 -> increased risk for prostate cancer, breast cancer
- Monounsaturated fat and omega-3 fats decrease risk for cancer
- Possible mechanisms of increased cancer risk
- Associated with high energy intake (see above)
- Presence of lipid soluble carcinogens
- Peroxidation of lipids
- Membrane composition of cells can be influenced by diet intake
- Prostaglandin synthesis
- Fatty acids are precursors to prostaglandins and prostacyclins
- Certain prostaglandins are pro-metastatic
- Fats can have direct cytotoxic effect
- Diacylglycerol is an intracellular second messenger -> activates protein kinase C
Other macronutrients and cancer
- Proteins probably don’t influence carcinogenesis
- Carbohydrates probably don’t directly influence carcinogenesis, but their increased intake means increased energy intake
Meat intake and cancer
- Saturated fat in red meat. Less in poultry
- Increased meat consumption -> increased colorectal carcinoma
- Increased meat consumption -> increased presence of N-nitroso compounds in stool
- N-nitroso compounds in cured and processed meats
- Heterocyclic amines in meat prepared at high temperature (especially grilling, frying)
Secondary bile acids and cancer
- Bile acids produced by the liver are primary. When these enter the intestines, bacteria will convert them into secondary bile acids
- Secondary bile acids are a risk for colorectal cancer
- Increased consumption of red meat and saturated fat have increased levels of secondary bile acids in the intestine, perhaps these foods change the microbiome of the intestines to bacteria that produce more secondary bile acids
Fibre intake and cancer
- Decreased fibre intake -> increased colorectal carcinoma
- Suggested intake: 30 g/day
- Types of fibre
- Water soluble (like pectin)
- Water insoluble (like cellulose, hemicellulose)
- Cancer preventative effects of fibre
- Takes more time to chew -> increased sense of fullness -> decreased energy intake
- Fibre binds carcinogenic substances and secondary bile acids
- Fibre decreases faecal transit time -> Intestines are less exposed to carcinogens
- Fibre dilute bowel content
- Fibre modifies the enteric bacterial flora, decreasing the production of secondary bile acids
Other dietary factors and cancer:
- Grilled, smoked, cured foods
- Hot foods and drinks
- Decreased vitamin D intake
- Inadequate fluid intake
- Contaminants
- Food additives, preservatives, artificial sweeteners
- Nitrites
- Nitrates
Phytochemicals and cancer
- Phytochemicals are chemical compounds of plant origin
- Mostly found in the peel or outer parts of fruits and vegetables
- Examples
- β-carotene
- Lycopene
- Lutein
- Glucosinolates
- Flavonoids
- Quercetin
- Mechanisms of cancer prevention
- Antioxidant effect
- Inhibit phase I biotransformation in liver
- Induce phase II biotransformation in liver
- Induction/inhibition of COX, LOX
- Anti-inflammatory effect
- Stimulate immune system
- Induce apoptosis
- Regulate intracellular signalling
- Arrest cells in the cell cycle
- Competitively inhibit oestrogen
- Inhibit DNA synthesis
- Inhibit angiogenesis
- Changes enteric bacterial flora
- Decrease expression of oncogenes
- Increase DNA repair
- Inhibit NF-κB
Alcohol consumption and cancer
- Pro: red wine contains phytochemicals (resveratrol)
- Cons:
- Irritation
- Fat soluble carcinogens in alcohol
- Alcohol itself is carcinogen
- Alcohol induces biotransformation enzymes
- Acetaldehyde is carcinogen
- Net effect of alcohol (even red wine) consumption: increased risk for cancer!
Summary (recommendations by American institute for cancer research)
- Be as lean as possible without being underweight
- Be physically active for at least 30 minutes every day
- Avoid sugary drinks
- Limit consumption of energy-dense foods
- Especially processed foods with much added sugar or fat
- Eat a variety of vegetables, fruits, whole grains, legumes
- Limit consumption of red meats and avoid processed meat
- Alcohol shouldn’t be consumed, or at least limited to 2 units (men) or 1 unit (women) per day
- Limit consumption of salty foods and foods processed with salt
- Don’t use supplements to protect against cancer
- Cancer survivors should follow recommendations for cancer prevention
- Mothers should exclusively breast feed for 6 months, and only after that can they add other liquids and foods
3. Principles of healthy diet
Component of diet
- Nutrients
- Macronutrients
- Lipids
- Proteins
- Carbohydrates
- Micronutrients
- Vitamins
- Minerals
- Macronutrients
- Dietary fibre
- Bioactive components
- Alkaloids
- Flavonoids
- Carotenoids
- Food additives
- Spices
- Preservatives
- Colouring
- Sweeteners
- Thickeners
- Stabilizing agents
Macronutrients
- Proteins should be 12 – 15% of the total calorie intake
- Carbohydrates should be 55 – 60% of the total calorie intake
- Fat should be 25 – 30% of the total calorie intake
Calories
- Males 19-30 years – 2500 kcal/day
- Females 19-30 years – 1900 kcal/day
- Requirements increased with increased level of activity
Fats
- 25 – 30% of total calorie intake
- Trans fats – < 2 % of total calorie intake
- Types of fats and their sources
- Unsaturated fats
- Monounsaturated fats (oleic acid)
- Olive oil
- Almonds
- Butter
- Avocado
- Polyunsaturated fats
- Omega-3 (α-linoleic acid, DHA, EPA)
- Flax seeds
- Linseed oil
- Walnuts
- Olive oil
- Fish oil
- Omega-6 (linoleic acid)
- Grapeseed oil
- Corn oil
- Walnuts
- Soybean oil
- Margarine
- Omega-3 (α-linoleic acid, DHA, EPA)
- Monounsaturated fats (oleic acid)
- Saturated fat (palmitic acid)
- Butter
- Meat fat
- Palm oil
- Coconut oil
- Trans fatty acids
- Industrially produced
- Naturally in beef, lamb, diary
- Unsaturated fats
- Effects of lipids on health
- Lipid-free diet ->
- dermatitis, coagulopathy, avitaminosis of lipid soluble vitamins
- Excess lipids in diet ->
- obesity, atherosclerosis, hypertension
- Saturated fatty acid intake -> increased serum cholesterol
- Monounsaturated fatty acid intake -> no change in serum cholesterol
- Trans fats intake -> increased risk for cardiovascular disease, serum cholesterol and cancer
- Lipid-free diet ->
- Essential lipids are necessary in the diet
- Omega-6
- Linoleic acid
- Precursor for arachidonic acid
- Arachidonic acid is pro-inflammatory
- Omega-3
- α-linoleic acid
- Precursor for EPA and DHA
- EPA, DHA are anti-inflammatory
- Omega-6:Omega-3 ratio is important.
- Optimal is 4:1.
- Ratio in western diet: 15:1 (too much omega-6)
- Omega-6
Dietary cholesterol
- Found in egg yolk, milk fat, animal fat, meat
- Factors which influence the composition and concentrations of serum lipoproteins
- Dietary intake of cholesterol
- The composition of the diet, especially the fats
- Saturated fat intake -> increased LDL
- Monounsaturated fat intake -> no change in LDL
- Polyunsaturated fat intake -> small decrease in LDL, but they have other anti-atherosclerotic effects
- The energy balance
Proteins
- 12 – 15 % of total calorie intake
- 0,8 g/kg of bodyweight
- Increased need in:
- Childhood
- Old age
- Pregnancy, lactation
- Tissue regeneration (infection, burns, postoperative)
- Exercise
- Protein turnover occurs in all proteins in the body
- Around 300g of protein turnover occurs each day
- Essential amino acids are necessary in the diet
- Histidine, isoleucine, leucine, lysine, methionine, phenylalanine, threonine, tryptophan, valine
- “Complete proteins” – proteins containing essential amino acids in sufficient amounts
- Proteins of animal origin
- Soy protein
- “Incomplete proteins” – proteins not containing all essential amino acids, or containing all essential AAs but not in sufficient amount
- Most proteins of plant origin
- Biological value of protein = how much of ingested protein is incorporated into proteins in the body
- Determined by which essential amino acid is present in the lowest quantity
| Food | Biological value |
| Breast milk | 100% |
| Egg | 100% |
| Milk | 90% |
| Beef | 90% |
| Chicken | 80% |
| Potatoes | 70% |
| Rice | 60% |
Carbohydrates
- 55 – 60% of total calorie intake
- Low carb intake -> gluconeogenesis, lipid metabolism
- High carb intake -> obesity, diabetes mellitus type 2, caries
- Carbs taste good (high palatability) -> excessive calorie intake
- Empty calories – foods with many carbs usually don’t contain many nutrients
- Types
- Monosaccharides
- Glucose
- Fructose
- Galactose
- Disaccharides
- Sucrose
- Lactose
- Maltose
- Oligosaccharides
- Maltotriose
- Fructotriose
- Polysaccharides
- Starch
- Glycogen
- Cellulose
- Monosaccharides
- Glycaemic index (GI) = the increase in blood glucose in the 2 hours after ingestion, compared to glucose
- Diets high in carbs with high GI -> diabetes mellitus, dyslipidaemia
- Causes glucose spike and insulin spike after eating
- Dates
- Instant rice
- Corn flakes
- Whole wheat bread
- Diets high in carbs with low GI -> decreased cholesterol and triglyceride
- Peanuts
- Soymilk
- Apple, pear
- Long-grain rice
- Diets high in carbs with high GI -> diabetes mellitus, dyslipidaemia
- Simple carbohydrates
- Quickly broken down
- High glycaemic index
- Found in
- Fruits
- Milk
- Vegetables
- Complex carbohydrates
- Slowly broken down
- Low glycaemic index
- Found in
- Bread
- Legume
- Rice
- Pasta
Dietary fibres
- 25 – 35 g/day
- = Large and complex mixtures of polysaccharides that aren’t digested and absorbed
- Types
- Cellulose
- Gums
- Effect on health
- Increases satiety
- Slow down glucose absorption
- Increase stool mass
- Increase GI bacterial health
- Protects against CRC
- Protects against type 2 diabetes
4. Epidemiology of malnutrition and nutritional deficiencies
- Micronutrient deficiency is widespread in developing countries, affecting 2 billion people worldwide
- Deficiency affects the most vulnerable groups most commonly
- Most common deficiencies
- Iron
- Vitamin A
- Iodine
- Malnutrition = inadequate or excess intake of a nutrient, leading to infections and disorders
- Underweight malnutrition – large problem in the developing world
- Affects mainly children and women
- Malnutrition increases risk for children to die from malaria, meningitis, pneumonia, gastroenteritis
Epidemiology of malnutrition
- Epidemiology is the study of the distribution and determinants of diseases and other health outcomes in human populations
- Types of studies in nutritional epidemiology
- Descriptive studies – an observational study that describes the characteristics of a population
- Describes the nutritional state of a population
- National surveys are often used
- Ecological studies – an observational study that measures the incidence of a disease in a population
- Can compare how the incidence of a disease in a population changes over time
- Can study whether certain populations have higher incidence of disease (like certain ethnicities, religions)
- Can study immigrants to assess the contributions of genetic and environmental factors
- Case-control studies – a retrospective observational study that compares people with a disease and without a disease and looks for possible risk factors
- Cohort studies – a prospective study that compares two groups, one group with a risk factor and another group without and compares their incidence of disease
- Intervention trials – a double blind experimental study where random subjects are assigned into two groups. One group receives a treatment, the other not. Health outcomes are compared.
- Descriptive studies – an observational study that describes the characteristics of a population
Types of malnutrition
- Growth failure
- Acute malnutrition
- Kwashiorkor
- Severe protein malnutrition but without total calorie deficiency
- Symptoms
- Oedema
- Pigmentation changes of skin and hair
- Impaired growth and development
- Ascites
- Liver disease
- Marasmus
- Severe protein and calorie malnutrition
- Symptoms
- Growth retardation
- Wasting of subcutaneous fat, muscle
- Kwashiorkor
- Chronic malnutrition
- Shortness
- Cognitive dysfunction
- Acute malnutrition
- Micronutrient malnutrition
- Iron deficiency
- Most common nutritional disorder – 2 billion people worldwide
- Causes anaemia
- Very prevalent in pregnant women and preschool children in developing countries
- Aggravated by parasite infection, malaria, HIV, TB
- Health effects
- Fatigue
- Poor pregnancy outcome
- Impaired physical and cognitive development
- Increased morbidity in children
- Prevention
- Increase iron intake
- Control infection
- Improve nutritional status
- Vitamin A deficiency
- Major cause of blindness in Africa, south-east Asia
- Affects mostly children and pregnant women
- Prevention
- Supplementation
- Increased breastfeeding
- Promotion of vitamin A-rich diet
- Fortification of food
- Golden rice – a type of rice fortified with vitamin A
- Iodine deficiency
- Iron deficiency
Cachexia
- = a complex metabolic syndrome characterised by loss of muscle with or without loss of fat, due to an underlying illness
- Frequently seen in COPD, chronic kidney disease, cancer
- Causes weight loss
- Anorexia, inflammation, insulin resistance and protein catabolism as associated with cachexia
- Not the same as starvation!
- Increases morbidity
Intervention of malnutrition and nutritional deficiencies
- Determine etiology of malnutrition
- Parasite
- Infection
- Increased demand
- Poor diet
- Effective measures
- Improve water supply, sanitation, hygiene
- Improve access to adequate amounts of healthy food
- Supplementation
- When deficiency is severe
- Can be used as preventative measure in high-risk populations
- Cost-effective
- Fortification of foods (adding nutrients to foods)
- Not appropriate in severe deficiency
- Requires participation of the food industry
- Diversify the diet
- Introduce nutrient-rich foods in the diet
- Change dietary habits
- Change agricultural habits
5. Dietary guidelines
General dietary guidelines (according to the 2015-2020 American dietary guidelines)
- Increased intake of whole grain, vegetables and fruits
- Decreases weight gain
- Reduced intake of sugar-sweetened beverages
- These are a large source of calories while containing few essential nutrients
- Increased intake of 100% fruit juice
- Decrease alcohol intake
- Alcohol intake is associated with weight gain, cancer and liver disease
- Decrease total number of calories consumed
- Monitor food intake
- By monitoring intake of the various nutrients, individuals become more aware of what and how much they eat and drink
- Eat more meals at home rather than eating out
- Prepare and serve smaller portions
- People eat and drink less when the portions are smaller
- Eat a nutrient dense breakfast
- Limit screen time
- Screen time is associated with overweight
- Reduce sodium intake (< 2300 mg/day)
- Reduce cholesterol intake
- Dietary cholesterol intake alone is no longer believed to increase serum cholesterol, however foods high in cholesterol are often also high in saturated fats
- Reduce daily trans fat and saturated fat intake
- Saturated fats should be replaced by unsaturated fats, preferably polyunsaturated fats
- Increase intake of vegetables of different colours, especially dark green
Specific population groups
- Pregnant women
- Should consume more folic acid (400 µg daily)
- Should consume more iron
- Limit intake of tuna, shark and swordfish (due to methyl mercury content)
- Older individuals
- Should consume more B12
6. Special nutritional considerations: vegetarianism
Vegetarian diet
- No meat, poultry, fish or other seafood is consumed
- Animal products like milk and eggs can be consumed
- Not all plant products contain all essential nutrients. Thus, a vegetarian diet must be well-planned to meet the daily recommended intake of all nutrients
- The vegetarian diet contains more than enough of
- Vitamins B, E, C
- Minerals
- Dietary fibre
- Unsaturated fatty acids
- Carbohydrates
- Plant sterols
- The vegetarian diet often brings other health benefits with it
- Vegetarians are usually generally health conscious
- Have decreased consumption of tobacco, alcohol, drugs
- Live a physically active life
- Have decreased intake of sugar
- Have decreased intake of calories
- Consume more potassium than sodium -> decreased risk for hypertension
- Vegetarians are usually generally health conscious
Special types of vegetarianism
- Lacto vegetarian – allows consumption of milk
- Ovo vegetarian – allows consumption of eggs
- Lacto-ovo vegeterian – allows consumption of milk and eggs
- Pesciterian – allows consumption of fish
- Vegan – no consumption or use of any animal product
Special nutritional considerations
- Protein
- Many plant foods are poor sources of protein or are incomplete proteins
- Thus, multiple plant sources of protein should be consumed to ensure all essential amino acids are consumed
- Protein deficiency is usually not a problem though, as vegetarians consume different protein sources
- Soy itself is almost as complete as animal protein
- Sources of protein for vegetarians
- Soy
- Legumes
- Grains
- Iron
- Vegetarians tend to have smaller iron stores than meat eaters
- But they don’t appear to have more iron deficiency anaemia
- Plant foods contain iron in ion form and not in heme form (which is found in meat)
- The heme form has higher bioavailability
- Vitamin C enhances iron absorption
- Calcium and dairy decrease iron absorption
- Sources for vegetarians
- Eggs
- Pulses (beans, chickpeas)
- Dark green vegetables
- Vegetarians tend to have smaller iron stores than meat eaters
- B12
- Unless fortified, no plant foods contain significant B12
- B12-containing foods should be consumed regularly
- Sources for vegetarians
- Milk
- Cheese
- Eggs
- Sources for vegans
- Supplements
- Fortified cereals, plant milk
- Nutritional yeast
- Omega-3 fatty acids
- Are mostly found in oily fish and fortified eggs
- Sources for vegetarians
- Flaxseed oil
- Rapeseed oil
- Soya oil
- Walnuts
- Fortified eggs
- Vitamin A
- Preformed Vitamin A is only found in animal foods
- Vegans only get vitamin A from converting beta-carotene, which is less efficient
- High amounts of beta-carotene should be ingested daily
- Found in most orange/yellow fruits and vegetables
- Iodine
- Iodine is mostly found in dairy and seafood
- Iodized salt should be consumed by vegans
Well-planned vegetarian diet contains
- Dark green vegetables
- Red and orange vegetables
- Legumes (beans and peas)
- Starchy vegetables (potatoes)
- Whole grains
- Fruits
- Eggs
- Soy products
- Nuts
- Seeds
7. Special nutritional considerations: Mediterranean diet, DASH- (Dietary Approaches to Stop Hypertension) diet
Mediterranean diet
- Based of food patterns typical of Greece, Crete and southern Italy
- Not only a diet, rather a lifestyle
- Contains regular physical activity and enjoying meals with families and friends
- Lower rates of multiple conditions in the region, which can be attributed to the diet
- Obesity
- Diabetes mellitus type 2
- Cancer
- Characterised by
- Abundant plant foods (fruits, vegetables, breads, cereals, potatoes, beans, nuts, seeds)
- Olive oil as the principle source of fat
- Dairy products (mainly cheese and yoghurt)
- Low-moderate consumption of fish and poultry
- Low consumption of meat
- Low consumption of wine, often with meals
- The diet is low in saturated fat (< 7% of calories)
- Total fat 30% of calories
How to change to a Mediterranean diet
- Consume whole grains rather than non-whole grains
- Consume more nuts
- Switch out butter and margarine with olive oil
- Use herbs and spices rather than salt and fat
- Eat more fish
- Limit consumption of red meat to just a few times a month
- Consume more low-fat diary and less high-fat diary
DASH – Dietary Approaches to Stop Hypertension
- Been proven to reduce blood pressure, LDL cholesterol and therefore cardiovascular risk
- Focuses on limiting saturated fats and cholesterol, while increasing foods rich in nutrients which reduce blood pressure
- Potassium
- Potassium:sodium balance should be 3:1
- Calcium
- Fibre
- Protein
- Potassium
- Characterised by
- Eating more vegetables, fruits and whole grains
- Including fat-free or low-fat dairy products
- Eating more fish, poultry, nuts, beans and vegetable oils
- Limiting foods high in saturated fat, like fatty meats, full-fat dairy products and oils like coconut and palm oil
- Limiting sugar-sweetened beverages and sweets
- Limiting red meat
- Limiting sodium
- Limiting saturated and trans fats
8. Special nutritional considerations: trendy diets
Palaeolithic diet (paleo diet)
- Tries to replicate the diet of hunters and gatherers during the stone age
- Assumes that people in the stone age didn’t consume starchy carbohydrates like potatoes and grains
- Based on the premise that human genetics haven’t adapted to the change in agriculture, and so a diet similar to the cavemen is best
- However, recent studies have shown that genetics can and have changed in response to changes in agriculture
- Recent studies have also shown that people in the stone age did actually consume starchy carbohydrates
- Diet is characterised by eating
- Fish
- Grass-fed pasture-raised meats
- Eggs
- Vegetables
- Fruit
- Fungi
- Roots
- Nuts
- The following are not consumed
- Grains
- Legumes
- Dairy products
- Potatoes
- Refined salt
- Refined sugar
- Processed oils
- The diet is generally
- Low in calories
- Rich in micronutrients
- Rich in fruits and vegetables
- Low in salt
- Special nutritional considerations
- Calcium
- Lack of diary can lead to calcium deficiency and is commonly seen
- Iodine
- Lack of table salt and dairy products can lead to iodine deficiency
- Calcium
Atkins diet
- Characterised by:
- High protein
- Very high fat
- Very low carbohydrate
- Unrestricted calories
- Forbidden foods
- Grains
- Vegetables
- Fruit
- Promoted foods
- Meat
- Cheese
- Eggs
- Fats
- Disadvantages
- High saturated fat intake
- Low fruit and vegetable intake
- High meat intake
9. Assessment of nutritional status, nutritional screening
Tools in the assessment of nutritional status – anthropometric measurements
- Anthropometry
- = measurement of height, weight, and proportions of a person
- Especially used in infants, children, pregnant
- Advantages of anthropometry
- High specificity, high sensitivity
- Many variables are acquired and measured
- Data can be graded on charts and compared to healthy subjects
- Disadvantages of anthropometry
- Difference in measurements depending on the observer
- Gives limited information on specific nutritional state
- Anthropometry in children
- Used to evaluate the child’s growth relative to what’s normal for its gender and age
- Body mass index – BMI
- Defined as the weight (kg) divided by the height squared (m2)
- High BMI – associated with type 2 diabetes and mortality
- Classification
- BMI < 18.5 – underweight
- BMI 18.5 – 25 – normal range
- BMI 25 – 30 – overweight (pre-obesity)
- BMI 30 – 35 – obese (grade 1 obesity)
- BMI 35 – 40 – severely obese (grade 2 obesity)
- BMI > 40 – morbidly obese (grade 3 obesity)
- Proportion of obese vs non-obese people in the western world has increased the last decades
- Waist circumference
- Predicts mortality better than any other anthropometric measurement
- Can be used to assess obesity
- Measured at the level of the umbilicus, rounded to nearest 0.5 cm
- Two risk levels exist according to waist circumference
- Level 1 – males – circumference > 94 cm
- Level 2 – males – circumference > 102 cm
- Level 1 – females – circumference > 80 cm
- Level 2 – females – circumference > 88 cm
- Hip circumference
- Measured at the point of greatest circumference around the hips, rounded to nearest 0.5 cm
- Waist/hip ratio
- Waist circumference divided by hip circumference
- Defined as central obesity if ratio > 0.95 in males or > 0.80 in females
- Skin fold thickness
- A special tool measured the thickness of a fold of skin
- Can be used to estimate the body fat percentage
- Very cheap, not very accurate
- Common sites to measure skin fold thickness:
- Triceps
- Abdomen
- Frontal thigh
- Chest
- Hydrostatic weighing
- By lowering a person into a pool of water and measuring how much water is displaced, we can find out the volume and therefore the density of the person
- The density can be used to estimate the body fat percentage
- Expensive, time-consuming, but very accurate
- Bioelectrical impedance analysis
- A machine measures the resistance (impedance) of the body and estimates the body fat percentage
- Not time-consuming, relatively expensive but not very accurate
Biochemical methods of assessment of nutritional state
- Advantages of biochemical methods
- Can detect changes early, perhaps before clinical symptoms
- Accurate measurements
- Disadvantages of biochemical methods
- Time consuming
- Expensive
- Requires trained personnel
- Biomarkers of nutritional state
- Serum haemoglobin
- Decreased in anaemia, protein deficiency or mineral deficiency
- Stool examination
- Presence of intestinal parasites can be seen
- Urine dipstick
- Can detect blood, sugar, albumin
- Urinary levels of minerals like potassium, sodium, fluoride, chloride, iodide
- Reflects the recent intake of minerals
- Level of nutrients in RBCs, adipose tissue, nails, hair
- Reflects dietary intake over weeks or months
- Cholesterol esters in RBC membrane
- Reflect recent lipid intake
- Transferrin levels
- Reflect protein intake in last week
- HbA1c
- Reflects average blood glucose level last 3 months
- Serum haemoglobin
Clinical assessment of nutritional state
- Advantages of clinical assessment
- Simple, most practical method
- Non-invasive
- Disadvantages of clinical assessment
- Can’t detect early
- Detected signs aren’t specific to certain dietary component
- Examination of areas like
- Hair
- Abnormal in protein, zinc, vitamin A, vitamin C deficiency
- Nails
- Abnormal in iron, protein deficiency
- Skin
- Abnormal in iron, folate, vitamin C, vitamin B2, vitamin A, zinc deficiency
- Angle of mouth
- Abnormal in iron, vitamin B deficiency
- Gums
- Bleeding in vitamin C deficiency
- Tongue
- Eyes
- Thyroid gland
- Enlarged in iodine deficiency
- Muscles
- Bones
- Abnormal in vitamin D and vitamin C deficiency
- Hair
Dietary assessment of nutritional state
- Methods
- Dietary recall – subject is asked to list foods consumed during a certain period of time, usually in the last 24 hours
- Quick, simple
- Depends on short term memory
- Doesn’t represent usual intake
- Food diary – subject writes a record of their intake as they eat
- Needs cooperation of the individual
- Food frequency questionnaire – subject is given a questionnaire that ask how often they consume a certain food
- Example: How many times a week do you eat bread?
- It’s easy to forget or underreport certain food habits
- Diet histories – subject is simply asked open-ended questions regarding their usual food habits
- Time consuming
- It’s easy to forget or underreport certain food habits
- Observed food consumption
- Dietary recall – subject is asked to list foods consumed during a certain period of time, usually in the last 24 hours
- Interpreting results
- Quantitative interpretation – calculating the amount of energy and specific nutrients the patient consumes and compare it to the recommendations
- Time-consuming
- Qualitative interpretation – comparing the different food groups the patient eats with the food groups of a recommended diet
- Quantitative interpretation – calculating the amount of energy and specific nutrients the patient consumes and compare it to the recommendations
Indirect methods of nutritional assessment
- Ecological variables, like crop production
- Economic factors
- Income per capita
- Population density
- Social habits
- Vital health statistics
- Infant mortality
- Fertility index
10. Epidemiology of obesity
Obesity
- Epidemiology
- Worldwide obesity has more than doubled since 1980
- In 2014 more than 1.9 billion (39%) adults were overweight. 600 million (13%) were obese
- North Africa, the Middle East and Latin America are almost as overweight as Europe
- Obesity is growing in the developing world. Here the number of overweight adults has more than tripled since 1980
- In Europe
- Romania, Italy least obese
- Hungary, Great Britain most obese
- Definition of obesity – according to WHO
- BMI 25 – 30 – overweight (pre-obese)
- BMI 30 – 35 – Obese (type I obesity)
- BMI 35 – 40 – Severely obese (type II obesity)
- BMI > 40 – Morbidly obese (type III obesity)
- Other tools in measurement of obesity:
- Hip-waist ratio
- Skinfold thickness
- Waist and hip circumference
- Types of obesity
- Hyperplastic obesity – number of adipocytes is increased
- Often seen in prepubertal obese people and people who have been obese since a young age
- Often peripheral obesity
- Hypertrophic obesity – adipocytes are hypertrophic
- Often seen in people who become obese in adulthood
- Often central obesity
- Male type (“android”)
- Associated with cardiovascular disease, cancer
- Female type (“gynoid”)
- Associated with varicose veins, thrombosis
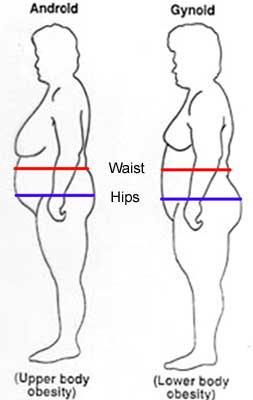
- Hyperplastic obesity – number of adipocytes is increased
- Central obesity
- Chronic inflammatory state
- Insulin resistance
- Dyslipidaemia
- Diabetes mellitus type 2
- Causes of obesity
- All cases of obesity are due to excessive energy intake compared to energy expenditure
- Genetic factors
- GLUT4
- IRS-1
- Adiponectin
- Leptin
- Genetic differences in metabolic rate
- Genetic differences in the reward of eating
- Excessive energy intake
- Physical inactivity
- Pregnancy
- Secondary obesity
- Certain drugs
- Hormonal imbalance
- Cushing syndrome
- Polycystic ovary syndrome
- Consequences of obesity
- Increased mortality
- Increased risk for diabetes mellitus type 2
- Obstructive sleep apnoea
- Metabolic syndrome
- Cardiovascular disease
- Arthritis
- Cancer
- Breast cancer
- Only postmenopausal
- Excess amount of oestrogen produced by adipose tissue
- Colorectal cancer
- Oesophageal cancer
- Endometrium
- Excess oestrogen
- Pancreas
- Renal cell cancer
- Breast cancer
- Mechanism of cancer development
- Increased level of hormones who stimulate cell proliferation
- Insulin
- Insulin-like growth factor
- Leptin
- Chronic inflammation
- Oxidative stress
- Activation of NF-κB
- Excess amount of oestrogen
- Increased level of hormones who stimulate cell proliferation
Obesity in childhood
- Tripled in last 30 years
- Lifelong lifestyle habits are established during childhood
- Much study time, television -> mild obesity -> too tired for sports or activity -> moderate obesity -> bullying causes obese child to eat comfort foods -> severe obesity
11. Dietary supplements and functional foods
Dietary supplementation
- Definition: A manufactured product intended to supplement the diet when taken by mouth as a pill, capsule, tablet or liquid
- Can provide natural or synthetic nutrients
- $37 billion industry in 2015
- 50% of Americans take dietary supplements
- Common types
- Multivitamins
- Sport nutrition supplements
- Calcium
- B-vitamins
- Vitamin C
- Glucosamine
- Fish oil
- Collagen
- Ginseng
- Glucosamine
- Probiotic
- Folic acid
- Medically indicated uses for dietary supplementation
- Changing diet to treat nutrient deficiencies is always preferred to dietary supplementation
- Folic acid in pregnancy
- Fish oil (omega-3 fatty acids have cardioprotective effect)
- In diseases with malabsorption (Crohn’s, chronic pancreatitis)
- Supplementing nutrients in patients who are not nutrient deficient has no effect!
- A balanced diet eliminates the need for dietary supplement! (which it’s required by law to be written on the nutritional label)
- Dietary supplements can’t make up for poor eating habits
- Food safety
- Most supplements are safe even in case of overdose, but some (like fat-soluble nutrients) are not
- Vitamin K supplementation can impair the function of blood thinners
- St. John’s wort speeds up the metabolism of many drugs, decreasing their effectiveness
- Antioxidants can reduce the effectiveness of chemotherapy
- Overdosing iron causes severe intestinal bleeding
- Overdosing vitamin A can cause birth defects
Functional foods
- Definition: Foods that have a potentially positive effect on health beyond providing nutrition
- Claimed to have health-promoting or disease-preventing effects
- Fruits and vegetables are functional foods as they contain molecules that are not nutrients but still beneficial
- Includes
- Fortified foods – foods with nutrients added to them
- Omega-3 added to butter
- Vitamin D added to milk
- Iodine added to salt
- Probiotics added to yoghurt
- Phytonutrients/phytochemicals = Molecules in fruits and vegetables that are not nutrients or vitamins
- Lycopene
- Anthocyanin
- β-carotene
- Lutein
- Wild fish
- Contains omega-3 fats
- Grains
- Contain dietary fibre
- Fortified foods – foods with nutrients added to them
12. Food additives
Food additives
- Definition: Substances added to food to preserve flavour or enhance its taste, appearance or other qualities
- Examples:
- Preserving foods with vinegar or salting
- Sweetening foods
- Adding taste enhancers like monosodium glutamate (MSG) – enhances umami taste
- Adding antioxidants to prevent oxidation of the food
- Adding nitrites to preserve the food longer
- Adding sulphur dioxide to wine to preserve it
- All food additives in Europe have a unique “E number”
- E100 – E199 – food colours
- E200 – E299 – preservatives
- E250 – sodium nitrite
- E300 – E399 – antioxidants, acidity regulators
- E400 – E499 – Thickeners, stabilizers, emulsifiers
- E500 – E599 – Acidity regulators, anti-caking agents
- E600 – E699 – flavour enhancers
- E700 – E799 – antibiotics
- E900 – E999 – Glazing agents, gases, sweeteners
- E1000 – E1599 – additional additives
- Approval of new food additives in the EU
- Takes 10+ years in total
- At least 5 years of safety testing
- Potential negative health effects
- Nitrites
- They are used to preserve cured meat
- They can react with amines in food in the acidic environment of the stomach to form nitrosamine, a known carcinogenic compound
- Some people have allergies to certain food additives
- Chinese restaurant syndrome – “allergy” to MSG
- Nitrites
13. Food safety, food safety testing
Food safety
- Definition: The scientific discipline describing handling, preparation and storage of food in ways that prevent food-borne illness
- Five key principles of food hygiene (according to WHO)
- Prevent contaminating food with pathogens
- Separate raw and cooked foods
- Cook foods for appropriate length of time and at appropriate temperature to kill pathogens
- Store food at the proper temperature
- Use safe water and safe raw materials
- Food-borne illness
- Bacteria
- Campylobacter jejuni
- Salmonella
- Enterohaemorrhagic E. coli
- Bacterial toxins
- Staphylococcus aureus toxin
- Clostridium botulinum toxin
- Bacillus cereus toxins
- Clostridium perfringens toxin
- Fungal toxins
- Aflatoxin
- Viruses
- Enterovirus
- Hepatitis A
- Norovirus
- Rotavirus
- Parasites
- Helminths (flatworms)
- Taenia solium/saginata
- Nematodes (roundworms)
- Trichinella
- Protozoa
- Helminths (flatworms)
- Bacteria
- In Hungary: National Food Chain Safety Office is responsible for national food safety
- Labelling
- “Best before” – a date after which the food may lose quality, but does not imply any serious health problems
- “Use by” – a date after which it’s no longer legal to sell the product due to serious risk of food-borne illness
- Taenia solium/saginata
- Pigs/cows eat eggs -> we eat pork/beef -> flatworms grow to multiple meters in the small intestine
- Trichinellosis – trichinella spiralis
- Hosts
- Pig
- Wild boar
- Trichinella adults invade intestinal wall of pig -> enter pig muscles -> lay larvae in the muscles -> pork is consumed by humans -> larvae grow to adults -> invade intestinal wall of human -> enter human muscles
- Symptoms:
- GI symptoms, myalgia, facial oedema.
- Symptoms resolve after 4 – 7 weeks
- Prevention
- Trichinoscope – a special device for detecting trichinella larvae in meat
- Appropriate heating of food – 20-30 min at 60℃
- Hosts
- Aflatoxin
- Produced by Aspergillus species
- Causes cirrhosis and hepatocellular carcinoma
- Only produced in warm, humid environments
14. Chemoprevention
- Chemoprevention refers to the use of natural compounds to try to reduce the risk of or delay the development or recurrence of cancer
- However, some chemopreventative agents turned out to be carcinogenic
- Vitamin E supplements actually increase the risk for prostate cancer
- Beta-carotene supplement increases the risk of lung cancer in smokers
- Recent research has determined several potentially chemopreventative natural compounds
- See also topic 2
Potentially chemopreventative natural compounds
- Most of these have proven effect in vitro but not in vivo
- Many of these are phytochemicals, chemical compounds of plant origin that are not nutrients, but which have other health effects
- Most phytochemicals are found in the peel or outer parts of the fruit/vegetable
- Many of the pigments found in fruits and vegetables are phytochemicals
- Ensure that you consume fruits and vegetables of different colours
- Types
- Carotenoids
- β-carotene
- Found in carrots
- Lutein
- Found in spinach
- Lycopene
- Found in tomatoes
- β-carotene
- Glucosinolates
- Found in brussel sprouts, broccoli, etc.
- Flavonoids
- Alkaloids
- Resveratrol
- Found in red wine, grapes, blueberries
- Curcumin
- Green tea
- Black tea
- Carotenoids
- Possible modes of action
- Antioxidant effect
- Inhibits reactive oxygen species (ROS)
- Inhibit phase I biotransformation enzymes
- Activate phase II biotransformation enzymes
- Anti-inflammatory effect
- Upregulation of NF-κB and COX-2 is common in many cancers
- In vitro studies have shown that phytochemicals inhibit the expression of these pro-inflammatory proteins
- Activation of MAPK
- MAP kinase is involved in differentiation and apoptosis
- Induction of apoptosis
- Anti-angiogenesis
- Phytochemicals can reduce VEGF and VEGF receptor expression
- Regulation of intracellular signalling pathways
- Phytochemicals can inhibit the Akt pathway
- Inhibit tumour invasion
- Tumours use MMPs to invade through basement membranes
- Phytochemicals can reduce the expression of MMP and increase expression of MMP inhibitors
- Antioxidant effect
15. Genetically modified organisms
Genetically modified organisms – GMO
- Definition: An organism whose genetic material has been altered using genetic engineering techniques
- Not necessarily with advanced machines and stuff
- Selective breeding is also a form of GMO
- Genes can have been transferred within the same species, across different species and even across biological kingdoms.
- New genes can be introduced, or endogenous genes can be enhanced, altered or disabled
- Examples
- Spider goat
- A GMO goat that received a spider-silk producing gene.
- They produced spider silk in their milk
- Crops
- Crops are genetically modified to
- Give higher yields
- Need fewer antibiotics
- Be more resistant to infections or drought
- Almost all crops in the western world today is genetically engineered in some way
- Especially corn, soy, potato, rice
- Crops are genetically modified to
- E. coli
- E.coli are genetically modified to produce insulin and growth hormone for pharmaceutical companies
- Oxitec
- Oxitec is a company that produced GMO mosquito that bred with natural mosquito, but their offspring died due to a lethal gene
- This could decrease the population of mosquitoes
- AquAdvantage salmon
- A GMO salmon with different growth hormone gene
- This salmon grows the whole year, not just during spring and summer
- Golden rice
- Rice plants genetically modified to produce rice with more β-carotene
- Invented to reduce vitamin A deficiency is deficient populations
- Spider goat
- Recombinant vaccines
- Certain vaccines are recombinant, i.e. the DNA for an antigen is inserted into a bacterium
- This produces many copies of the antigen, which can be used in a vaccine
- Edible vaccines
- Crops like potatoes can be genetically engineered to produce (non-harmful) antigens from infections, which the immune system can create immunity against
Potential harmful effects
- Eosinophilia-myalgia syndrome
- A condition that affected many people who took GMO-produced tryptophan supplements
- The tryptophan supplements were contaminated with an unknown toxin, causing eosinophilia and myalgia
- Bt toxin
- Many crops are genetically engineered to produce Bt toxin, a toxin that kills insects that feast on the crops
- This is used to decrease the amounts of pesticides necessary to maintain a crop
- Bt toxin may be toxic to humans
- May damage intestinal cells
- May promote growth of H. pylori
- Glyphosate
- Almost 80% of the world’s crops are GMO’d to tolerate glyphosate
- Glyphosate is a herbicide which might cause kidney damage in humans
- The use of glyphosate has skyrocketed after GMO-ing crops to tolerate it became possible
Labelling of GMO
- In USA – GMO does not have to be labelled
- In EU
- All intentional GMO must be labelled
- Unintentional GMO is not labelled, unless it affects for more than 0.9% of the food
Horizontal gene transfer
- Exchange of genetic material between organisms without producing a new offspring
- Examples
- The 2016 World Food Prize – genes were horizontally transferred from a bacterium to the genome of a sweet potato
- Amflora – a GMO potato which produced only amylopectin and no amylose, unlike normal potatoes
- It also contains a gene for antibiotic resistance.
- If consumed, bacteria in our gut could acquire these resistance gene by horizontal gene transfer
16. Interaction of environmental and genetical factors in disease development
- Most diseases are due to a combination of genetic and environmental factors
- We cannot change the genetic factors but we can change environmental factors
- Certain genes can increase the risk of disease after exposure to certain environmental factors
- Exposure + susceptible genotype -> high risk
- Exposure + not susceptible genotype -> moderate risk
- No exposure + susceptible genotype -> low risk
- No exposure + not susceptible genotype -> low risk
- Gene-environment interaction studies
- Describe how genetic and environmental factors influence the risk of developing disease
- The exposome = all the environmental exposures of a person
- The phenome
- = the phenotype of all cells in a person
- = the sum of the exposome and the genome
- Concept is demonstrated by an epidemiological study of oven workers
- Oven workers at a steel company are exposed to PAH emissions from the ovens. The amount of exposure depends on where they work
- Result of study: workers who smoked on their free time had more chromosomal damage as a result of oven emission exposure
- Conclusion: Smoking reduced DNA repair capacity, increasing the susceptibility to PAH
- Single nucleotide polymorphisms (SNPs)
- = point mutations in a single nucleotide
- Basically means small variations in genes between individuals
- Certain SNPs are associated with increased risk of diseases
- SNPs of GSTM1 – increased risk for colorectal cancer
- SNPs of XRCC1 – increased risk for colorectal cancer
- SNPs of NAT2 – increased risk for colorectal cancer
- SNPs of p53 – increased risk for colorectal cancer
- A1 variant of DRD2 – increased risk for cervical cancer and head and neck cancer
- See also topic 28 (molecular epidemiology) in public health 1 + 2
17. Genomics and epigenetics in public health. Nutrigenomics
- Most diseases with a genetic component can not be traced back to a single gene but rather multiple
- Exceptions: Cystic fibrosis, Huntington disease
- Genomics = the interactions of all genes and their combined influence on the organism
- Genetics = the study of heredity. The effect of single gene mutations on the organism
- Genomics in public health – Using genome-based discoveries for health benefits of the population
- Genomics are important in
- Determining why exposure only causes the disease in some people
- Determining why prognostic factors have different importance in different people
- Determining why treatment only works in some people
- How to start:
- Candidate gene studies
- A gene is suspected for having a role in disease
- Identify differences in one gene in patients and controls
- Genome-wide association studies
- No prior gene candidate is needed
- Identify genetic differences in the whole genome of patients and controls
- Can find alleles of a gene which increases susceptibility
- Candidate gene studies
- Personalized medicine
- Use genetic testing to find screening, treatment, and other preventative measures that are best suited for the patient
- Will prevent overdiagnosis and overtreatment
- Examples
- Genetic information of nicotine metabolism can be used to personalize smoking cessation
- Genetic information can give indication for screening, if high-risk genotypes are present
- Genetic information can tell us upfront which treatments will be most effective
Epigenetics
- Definition: Instructions for the cell on how and when to read DNA
- Epigenetics changes gene expression
- Genetically identical organisms can have different phenotype due to different epigenetics
- Types
- Acetylation of histones
- Methylation of DNA
- Presence of miRNA
- Chromatin remodelling
- Environmental factors can change epigenetics of an individual, and therefore the expression of the DNA
- Folic acid necessary for DNA methylation -> deficiency could theoretically cause hypomethylation and carcinogenesis
- MicroRNA profiles in blood could be used as biomarkers
- Already used for CRC
- Drugs affecting epigenetics = epigenetic drugs
- Used as chemotherapeutic agents against cancer
- Epigenetic alterations are reversible and can be reversed by these drugs
- Unlike genetic mutations
- They demethylate DNA or acetylate histones
- This can reactivate silenced tumor suppressors, repress activated oncogenes, etc.
Nutrigenomics
- Definition: The relationship between nutrition and genomics
- Basically how what you eat can change epigenetics
- Deficiency of certain nutrients (folate, B12, C, E) can cause DNA changes similar to those seen after radiation
- Folate
- Folate is required for DNA methylation
- Folate deficiency -> DNA hypomethylation -> carcinogenesis
- Methyl-donating nutrients
- Diets high in methyl-donating nutrients can alter gene expression
- Especially during early development
- Examples
- Methionine
- Folate
- B12
- Maternal nutrition
- Maternal nutritional status during early pregnancy can cause permanent epigenetic changes in the foetus
18. Molecular basics of carcinogenesis
- DNA damage to normal cell -> mutations in genome -> altered gene product -> Tumor suppressors ↓ or oncogenes ↑
- Protective mechanisms against carcinogenesis
- DNA repair enzymes
- Tumor suppressors
- Characteristics of cancer cells
- Inhibition of apoptosis + lack of response to inhibitory factors -> capable of self-maintained replication, long survival
- Mutagenic agents/defective DNA repair -> genetic instability -> more mutations
- Capable of angiogenesis
- Capable of invasion and metastasis
- Theories of carcinogenesis
- Somatic mutation theory (classic theory): cancer results from accumulation of mutations in susceptible cells
- Process
- Chemical, radiation, virus, etc. exposure to the cell causes mutations
- Mutations causes activation of proto-oncogenes and inactivation of tumour suppressor genes
- Cell transforms from healthy -> pre-cancerous -> cancerous
- Counterarguments
- 1: the stroma of the cancer is not mutated but highly influences tumor development, either positively or negatively
- Healthy cells transplanted to certain cancer stromas will become cancerous
- Cancer cells transplanted to other cancer stromas will not become more malignant
- 2: Many cancers acquire mutations first after they become cancerous
- Process
- Cancer stem cell theory
- Cancer cells arise from stem cells that accumulate damage as they divide
- Somatic mutation theory (classic theory): cancer results from accumulation of mutations in susceptible cells
- Gene dysfunction is not necessarily due to gene mutation – it can also be due to epigenetic malfunction
- Epigenetic malfunctions are reversible
- “Epigenetic drugs” reverse these malfunctions
- Tumour types can be subclassified according to their gene expression
- These subtypes have different biological properties and diagnosis
- Examples
- HER2 positive and negative breast cancer
- ALK positive and negative lung cancer
19. Primary and secondary factors of epidemic process (virulence, source of infection, means of transmission, susceptible host)
Basics of infectious disease
- Terminology
- Colonization = an organism is replicating in a host but causes no disease
- Sporadic case = case not connected to other cases
- Outbreak = a greater-than-expected number of cases
- Endemic = high occurence of a disease within a given geographical area or population
- Example: Malaria is endemic to sub-Saharan Africa
- Epidemic = outbreak of a disease within a region in a country, or multiple countries
- COVID-19 while it was yet to spread out from China
- Pandemic = global disease outbreak
- COVID-19 after it had spread to the whole world
- Endemic = high occurence of a disease within a given geographical area or population
- Phases of infectious disease
- Infection
- Incubation period
- Prodromal phase
- Symptomatic phase
- Healing/reconvalescence/death
- Levels of infection
- Colonization
- E.g. S. aureus in nasopharynx
- Subclinical infection
- Before symptoms occur
- The disease may be contagious at this stage
- Latent infection
- After initial symptoms has occured, but before they recur
- The disease may be contagious at this stage
- E.g. Latent stage of herpes simplex virus
- Manifest (clinical) infection
- Colonization
- Seasonality of infections
- = some diseases have increased number of cases regularly in a certain season
- Influenza in the winter
- Diphtheria in the autumn
- Cyclicity of infections
- = some diseases have increased number of cases regularly at longer intervals
- Pandemic flu every 30 – 40 years
- Diphtheria every 12 years
Epidemic process
- Epidemic process = the process of spreading of infectious diseases among people
- Characteristics of infectious diseases
- Caused by infectious agent
- Has a well-defined incubation period
- Has an acute course
- After resolution the immune system has developed immunity
- Factors of the epidemic process
- Primary (direct) factors
- Sources of infection
- Possible routes of transmission
- Susceptible human persons
- Secondary (indirect) factors
- Natural factors
- Social factors
- Primary (direct) factors
- Primary (direct) factors of epidemic process
- = Those factors that directly influence the spreading of the disease
- The source of the infection
- The reservoir is the habitat in which the infectious agent normally lives, grows and multiplies
- Can be humans, animals or the environment
- Anthroponosis = an infectious disease that is transmissible from human to human
- Zoonosis = An infectious disease that is transmissible from vertebrate animals to humans
- The reservoir may or may not be the source from which an agent is transferred to the host (it may be reservoir -> environment/animal -> human)
- Source = the location from which the infectious agent is immediately transmitted to the host (not the same as reservoir)
- Environmental reservoirs
- Plants, soil, water
- Many fungal agents have reservoir in soil
- Legionella pneumophila has reservoir in stale waters
- Carriers = a person with inapparent infection who can transmit the infectious agent to others
- Asymptomatic/healthy carrier
- = carrier who never experience symptoms themselves
- Incubatory carrier
- = carrier who can transmit the agent during the incubation period before the clinical symptoms begin
- Convalescent carrier
- = carrier who has recovered from the illness but can still transmit the infectious agent
- Asymptomatic/healthy carrier
- Carriage may be
- Transient
- = organism can be transmitted only for a short period of time
- Intermittent
- = organism can be transmitted sporadically
- Chronic
- = organism can be transmitted for a long time
- Hepatitis B, salmonella typhi
- Transient
- The reservoir is the habitat in which the infectious agent normally lives, grows and multiplies
- The route of transmission
- Direct transmission
- Contact
- Sexually
- Transplacental
- Transplantation
- Respiratory droplets (> 5µm)
- Indirect transmission
- Airborne
- Droplets (< 5µm)
- May be suspended in air for a long time and can travel great distances
- Waterborne
- Through drinking water, bathwater
- Water can be contaminated with human/animal discharge, sewage
- Foodborne
- Food can be infected by improper handling
- Microorganisms can multiply in food
- Soil
- Personal objects
- Bed
- Clothes
- Door handle
- Insect-borne (vectors)
- Mosquitoes, fleas, ticks
- Infectious agent can be carried on the inside of or outside of the insect
- Airborne
- Direct transmission
- The susceptible population
- Susceptibility
- = a feature of a person that makes it possible for an infectious agent to cause illness in him
- Individual susceptibility – depends on the immune system of the individual
- Population susceptibility – depends on the proportion of susceptible and non-susceptible individuals
- Susceptibility
- Secondary (indirect) factors of epidemic process
- = Those factors that help the spreading of infections and affect the spread and duration of epidemics
- Living and working environment
- Weather
- Nutritional status
- Social factors
- Status of health care
Virulence
- Infectivity
- = out of 100 people exposed to a certain infectious agent, how many will be infected?
- Pathogenicity
- = out of 100 people exposed to a certain infectious agent, how many will not only be infected but also sick?
- Measles, varicella – close to 100%
- Diphtheria – 30%
- Poliomyelitis – 1%
- Lethality
- = out of 100 people who got the disease, how many died?
20. Nosocomial infections. Sterilization, disinfection
- See the comments
- Definitions
- Nosocomial disease = disease which is the result of treatment in a hospital
- Nosocomial infection (hospital-acquired infection) = infection which is the result of treatment in a hospital
- Nosocomial epidemic = nosocomial infection that affects two or more patients, and there is a connection between the cases
- Commensal bacteria
- Bacteria which are normally present, but can cause disease in compromised humans
- Problems with nosocomial infections
- Many people in small area
- Hospitalized people often have impaired immunity or condition
- Microorganisms in the hospital often have increased resistance to antibiotics
- Microorganisms in the hospital are often more virulent than microorganisms in the community
- The primary factors of epidemic process for nosocomial infections
- Source of nosocomial infection
- The patients themselves
- From commensal bacteria
- Other patients
- Staff
- Visitors
- Medical equipment
- Bedsheets
- The patients themselves
- Route of transmission
- Direct contact
- Indirect
- Airborne
- Waterborne
- Foodborne
- Objects, instruments
- Clothing
- Bedsheets
- Susceptible population
- High number of susceptible people
- Infants
- Elderly
- Immunocompromised
- Diabetes
- Cancer
- Polytrauma
- Surgical patients
- Secondary factors
- Crowded rooms
- Insufficient number of cleaning and nursing staff
- Lack of medical staff’s preventive approach
- Source of nosocomial infection
- Pathogens
- Bacteria
- Staph. saprophyticus, Staph. epidermidis
- E. coli
- A commensal bacterium
- May colonize surgical sites, needles, catheters
- Can be highly antibiotic resistant
- Clostridium
- Causes gangrene
- Staph. aureus, MRSA
- A commensal bacterium
- Pseudomonas
- Likes wet and damp areas
- Viruses
- Hepatitis B, C
- Transfusions, dialysis, injections, endoscopy
- RSV, rotavirus, enterovirus
- Faecal-oral or hand-to-mouth
- Hepatitis B, C
- Parasites
- Giardia lamblia
- Scabies
- Fungi
- Often cause infections in immunosuppressed patients
- Candida albicans
- Aspergillus
- Cryptococcus
- Cryptosporidium
- Bacteria
- Diseases
- Pneumonia
- 20 – 50% mortality rate of healthcare-associated pneumonia
- S. aureus
- Pseudomonas
- Klebsiella
- Risk
- Intubation
- Artificial ventilation
- UTI
- 35% of nosocomial diseases
- 0,1% mortality
- E. coli (endogenous)
- Risk: Catheter
- Surgical site infections
- S. aureus
- E. coli
- Sepsis
- 23% mortality
- Risk: Infusion/injection
- Pneumonia
- Most commonly affected wards
- Surgery
- ICU
- Paediatrics
- Respiratory tract infections and sepsis are the most common cause of mortality in hospitals
- Catheters, surgical wounds, intubation, artificial ventilation are common foci where infection can originate
Preventing nosocomial infections
- Risk stratification
- Reducing person-to-person transmission
- Disinfection of hands
- Before, during and after patient contact
- Disinfection = reduce the number of microorganisms, killing most harmful microorganisms
- Sterilization = kill all microorganisms
- Personal hygiene
- Protective equipment
- Disinfection of hands
- Preventing transmission from the environment
- Asepsis, antisepsis, isolation of patients
- Sterilization of equipment
- Limit overuse of antibiotics
- Education and training of medical staff
Multi-resistant bacteria
- MRSA
- Infects skin, wounds, urinary tract, respiratory tract
- ESBL – extended spectrum beta lactamase
- Resistant to cephalosporins, penicillins and aztreonam
- Treatment: carbapenems
- Often in E. coli or Klebsiella pneumoniae
21. Infectious diseases worldwide
- Epidemiology
- Lower respiratory tract infections is the fourth most common cause of death globally
- Diarrhoeal disease and tuberculosis are number 9 and 10
- Communicable diseases are a much larger problem in developing regions (Africa, Middle East) than in developed regions
- Types
- Seasonal outbreaks – outbreaks in a certain season
- Influenza – winter
- Diphtheria – autumn
- Cyclic outbreaks – outbreaks at a certain interval
- Pandemic flu – every 30 – 40 years
- Diphtheria – every 12 years
- Seasonal outbreaks – outbreaks in a certain season
Important worldwide diseases
- Influenza
- Pertussis
- Tuberculosis
- Neisseria meningitidis
- HIV
Recently emerging pathogens
- Vancomycin-resistant S. aureus (VRSA)
- SARS, COVID-19 – coronavirus
- Carbapenem-resistant Klebsiella
22. Prevention of infectious diseases: vaccination, chemoprophylaxis
- Vaccination prevents 2-3 million deaths every year
- An additional 1.5 million deaths could be avoided with further vaccination
- Immunogenicity
- = the ability of a vaccine to provoke an immune response
- Can be measured by measuring circulating antibodies
- Protectivity
- = how well the vaccine protects against the disease
- Must be measured with long-term observational studies
- Reactogenicity
- = how many adverse reactions the vaccine produces
- Complications of vaccines
- = serious side effects
- Very rare
- Most commonly severe allergic reactions
- Staff is trained to handle it
- The Hempt-vaccine against rabies was used until ’89, but was stopped because it caused demyelination
- Accidents related to vaccination
- Misdosage
- Inappropriate administration technique
- Using expired vaccines
- Not following the correct schedule
- Using contaminated vaccines
- “Ideal” vaccine
- 100% efficiency for all ages
- Only needs a single administration
- Does not cause side effects
- Stable under various environmental conditions
- Easily administrated (preferably oral)
- Low price
- Obviously doesn’t exist
Types of vaccines
- Live, attenuated vaccine
- The pathogen is attenuated, meaning that it is manipulated to become much less pathogenic
- The attenuated pathogen has limited ability to reproduce in humans
- Advantages
- The closest vaccine to a natural infection
- Provokes both humoral and cellular immune response
- Long-term effective protection with only one or two doses
- Disadvantages
- Can’t be given to immune compromised patients
- Need to be continuously refrigerated
- Small risk of the pathogen turning virulent
- Currently very hard to make for bacteria
- Examples
- MMR
- Chickenpox (varicella)
- BCG (Tuberculosis)
- OPV (oral polio vaccine, Sabin)
- Inactivated vaccine (= killed vaccine)
- The pathogen is killed with chemicals, heat or radiation
- Advantages
- No risk of the pathogen turning virulent (as it is dead)
- No refrigeration needed (as it is dead)
- Disadvantages
- Stimulates weaker immune response
- Several doses and booster shots are necessary, requiring regular access to healthcare
- Examples
- IPV (Salk polio vaccine)
- HAV (Hep A)
- Rabies
- Influenza
- Toxoid vaccine
- Can be made for bacteria who produce toxins
- Toxin is extracted from the bacterium and inactivated with formalin, so that it is no longer pathogenic -> now called a toxoid
- Used when the illness is caused by the toxin and not the bacterium itself
- Advantage
- Rarely causes side effects
- Stable, doesn’t require refrigeration
- No risk of acquiring the disease
- Disadvantage
- Several doses may be needed
- Stimulates weak immune response
- Do not give herd immunity
- Examples
- Diphtheria
- Tetanus
- Subunit vaccine
- Instead of giving the entire microbe as a vaccine, certain subunits (antigens) are given instead
- Examples
- Hepatitis B (HBsAg)
- Acellular pertussis (aP)
- Conjugate vaccine
- For bacteria protected by a polysaccharide capsule
- Polysaccharides are weak antigens, meaning that they stimulate weak immune responses
- The polysaccharide antigen of a bacterium is conjugated (attached to) a highly immunogenic protein antigen
- This stimulates a strong immune response against both the polysaccharide antigen and the protein antigen
- Advantages
- Give a strong immune response with long-term protection
- Disadvantages
- Multiple shots or booster shots may be necessary
- Example
- Haemophilus influenzae type b
- Meningococcus (Neisseria meningitidis)
- DNA vaccine
- Only in experimental stages
- Genes for antigens are inserted into bacteria, which produce plasmids (circular DNA) of these antigen genes
- Plasmids are inserted into the body. Cells of the body will take up the plasmids and start synthesizing the antigen from the plasmid
- The immune system recognizes the antigen produced as foreign and triggers immune response
- Recombinant vector vaccines
- Only in experimental stages
- Genes for antigens are inserted into bacteria, which synthesize large amounts of the antigen
- Antigen is then purified and given as a vaccine
Who gets vaccines:
- Age-specific compulsory vaccines
- BCG
- Haemophilus influenzas type b
- DTaP (diphtheria, tetanus, acellular pertussis)
- IPV (Salk polio)
- MMR (measles, mumps, rubella)
- Hepatitis B
- Pneumococcus
- HPV
- Compulsory vaccines for at-risk groups
- Tetanus
- Rabies
- Hepatitis A
- Non-compulsory vaccines for at-risk groups
- Influenza
- Job-related vaccines
- Rabies
- Meningococcus
- Tick-borne encephalitis
- Travel-related vaccines
- Yellow fever
- Cholera
- Typhoid fever
- Japanese encephalitis
Chemoprophylaxis
- Definition: Administering drugs for the purpose of preventing disease or infection
- Can be given
- Preexposure – before the exposure to the pathogen
- Postexposure – after the exposure to the pathogen but before symptoms develop
- Examples
- Giving antiretroviral drugs to people at high risk for HIV right after being exposed to HIV
- Like health care workers who come in contact with HIV
- Giving antimalaria drugs to people before, during and after travelling to malaria-prone areas
- Giving antibiotics to people who travel to areas where Traveller’s diarrhoea (ETEC) is common
- Giving antibiotics to people who have been exposed to bacillus anthracis
- Giving antibiotics to people who have been exposed to Neisseria meningitidis
- Giving antiretroviral drugs to people at high risk for HIV right after being exposed to HIV
23. Epidemiology and prevention of vaccine-preventable diseases, mandatory immunisation for children
Dr. Katalin Szendi said in the seminar that you don’t have to learn the vaccination program for Hungary – you can learn the one for your home country. They’re all mostly similar anyway.
Epidemiology of vaccine-preventable diseases
- Immunization prevents 2 – 3 million deaths every year
- An additional 1,5 million deaths could be prevented by additional immunization
- 20 million infants worldwide are missing out on basic vaccines
Prevention of vaccine-preventable diseases
- Surveillance
- Observing, predicting, and minimizing outbreaks, epidemics and pandemics
- 3 steps for improving worldwide immunization
- Integrating immunization with other health services, like postnatal care
- Strengthening health system so that vaccines continue to be given even in times of crisis
- Ensuring that everyone has access to and can afford vaccines
Vaccination program for Norway (as of 2017)
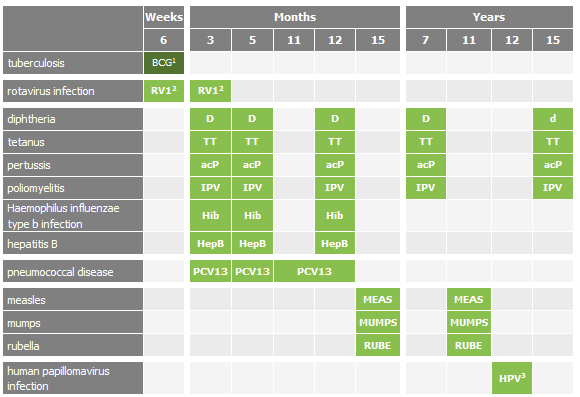
| Age | Vaccination against |
| Infancy (only for children with parents from high-risk countries) | Tuberculosis (BCG) |
| 6 weeks | Rotavirus |
| 3 months | RotavirusDiphtheria, tetanus, pertussis, poliomyelitis, Haemophilus influenzae-type B- and hepatitis B (DTP-IPV-Hib-Hep B)
Pneumococcus (PCV) |
| 5 months | DTP-IPV-Hib-Hep B and PCV |
| 12 months | DTP-IPV-Hib-Hep B and PCV |
| 15 months | Measles, Mumps, Rubella (MMR) |
| 7 years | DTP-IPV |
| 11 years | MMR |
| 12 years | Human papillomavirus (HPV), 2 doses |
| 15 years | dTP-IPV |
24. Epidemiology and prevention of airborne bacterial infections
Airborne infections:
- Inhalation of organisms suspended in the air on water droplets or dust particles
- Prevention:
- Handwashing
- Keep distance from sick people
- Sick people should keep distance from healthy people
- Vaccines
Bacterial airborne infections:
- Tuberculosis
- Diphtheria
- Pertussis
- Neisseria meningitidis (meningococcus)
- Haemophilus influenzae
- Streptococcus pneumoniae (pneumococcus)
- Legionnaire disease
Tuberculosis
- Mycobacterium tuberculosis hominis/bovis
- Epidemiology
- 9th leading cause of death worldwide
- 27 000 new cases every day
- Leading cause of death in HIV-positive
- Incidence and mortality dropping in the last 20 years
- Globally the incidence decreases by 2% each year
- 95% of TB-related deaths occur in low- and middle-income countries
- Incidence of multidrug and extensively drug resistant TB increases
- Risk factors for severe TB
- HIV (or other immune suppression)
- Severe disease (DM, renal failure)
- TNF alpha inhibitors
- TB is most prevalent among
- Migrants
- Homeless
- Poor people
- Drug abusers
- Treatment
- Childhood TB is generally treatable
- Adult TB is less treatable
- Prevention
- Isolation of TB patients
- Disinfection by UV light or tuberculocidial disinfectants
- Special air filters
- Routine TB testing for high-risks
- BCG vaccine
- Live attenuated Mycobacterium bovis
- Unchanged since 1921
- Only 50% effective against TB
- Good protection against childhood TB meningitis and miliary TB
- Poor protection against adult pulmonary TB
- Intradermal injection in the deltoid
- If given subcutaneously -> can form abscess
Diphtheria
- Corynebacterium diphtheriae
- Epidemiology
- Global reported cases down since vaccine was introduced in the 80s
- Very rare in countries with high coverage with vaccine
- Clinical features
- Short incubation period
- Produces pseudomembrane in the pharynx
- Makes breathing and swallowing difficult
- Produces diphtheria toxin
- Myocarditis
- Peripheral neuropathy
- Nephritis
- Vaccine
- Toxoid vaccine – toxin is inactivated with formalin
- DTaP vaccine at 3, 5 and 12 months, 7, 15 years (in Norway) + booster (Tdap) every 10 years
- Vaccine lasts 10 years
- Intramuscular vaccine
- Because vaccine doesn’t protect against the infection itself, only the (toxin-mediated) disease, there is no herd immunity!
Pertussis
- Bordetella pertussis
- Epidemiology
- Important cause of infant death worldwide
- It’s a public health concern even in countries with high vaccination coverage
- Produces pertussis toxin
- Clinical features
- Whooping cough – paroxysmal coughing
- Pneumonia
- Apnoea
- Vaccine
- Acellular pertussis (DTaP)
- Given at 3, 5 and 12 months, 7, 15 years (in Norway) + booster (Tdap) every 10 years
Streptococcus pneumoniae (pneumococcus)
- Epidemiology
- Often in fall, winter
- Clinical features
- Common cause of community-acquired pneumonia, bacterial meningitis
- Bacteraemia
- Otitis media
- Colonizes nasopharynx
- Vaccine
- Conjugate vaccine
- Given at 3, 5 and 12 months
Haemophilus influenzae
- Colonizes nasopharynx
- Causes otitis media, meningitis, epiglottitis, sinusitis
- Vaccine
- Conjugate vaccine
- Only for H. flu type b – the only type with a capsule and therefore only pathogenic type
- 3, 5 and 12 months
Legionellosis
- Legionella pneumophila
- Epidemiology
- Mostly affects older males
- Risk factors
- Smoking
- Lung disease
- Recent intubation
- Inhalation of contaminated aerosol
- Two forms
- Non-pneumonic form – causes Pontiac disease (influenza-like illness)
- Pneumonic form – causes Legionnaire disease – severe pneumonia
- -> respiratory failure -> death in 5%
- No vaccine available
Neisseria meningitidis
- Epidemiology
- Mostly occurs in sub-Saharan Africa
- Epidemics during winter, spring
- Serotype B and C account for most cases in western world
- Serotype A accounts for most cases in Africa
- No animal reservoir – only human
- Clinical features
- Lethality 10% when treated, 50% when untreated
- Mainly affects children and infants
- Causes bacterial meningitis
- Asymptomatically colonizes nasopharynx in 10 – 30% of healthy
- Vaccine
- Polysaccharide vaccine used during outbreaks
- Conjugate vaccine used for prevention
- Chemoprophylaxis
- Antibiotic prophylaxis for people in close contact to infected
25. Epidemiology and prevention of airborne viral infections
Airborne viral infections
- Influenza
- Measles
- Mumps
- Rubella
- Varicella zoster
- Parainfluenza
- Varicella
- Epstein Barr virus
Measles
- Measles virus, a paramyxovirus
- Also called morbillivirus
- Highly contagious, serious disease
- Contagiosity index 95-99%
- Epidemiology
- Used to be a leading cause of infant death, blindness and disability
- Most commonly affects children < 12 months
- Vaccination caused an 80% drop in cases from 2000 to 2017
- During this time 21 million deaths have been prevented
- This has made the measles vaccine one of the best buys in public health
- Recently, measles has begun to bounce back
- Because of anti-vaxxers (pro-diseasers)
- Spread by coughing and sneezing
- Clinical features
- 1-3 deaths per 1000 in developed countries
- 150 deaths per 1000 in developing countries
- Due to these children being malnourished and having worse immunity
- Maculopapular rash
- Blindness
- Severe diarrhoea
- Otitis media (due to bacterial superinfection)
- Pneumonia (due to bacterial superinfection)
- Encephalitis
- Subacute sclerosing panencephalitis
- No specific treatment
- MMR vaccine
Rubella
- Rubella virus, a togavirus
- Epidemiology
- 100 000 are born with congenital rubella syndrome every year
- Clinical features
- Generally mild illness
- Part of TORCH (congenital rubella syndrome)
- Serious for pregnant women
- Causes deafness, blindness, in infants
- No specific treatment
- MMR vaccine
Influenza
- Type A and B exists – type A is most pathogenic
- Very hard to vaccinate against – antigens change constantly
- Antigenic drift – point mutations in the Haemagglutinin (H) and neuraminidase (N) genes
- Antigenic shift – two different strains combine to form a new strain with different surface antigens
- Pandemics in history
- Spanish flu (1918)
- Asian flu (1957)
- Hong Kong flu (1968)
- Swine flu (2009)
- Seasonal epidemics during winter
- Can cause severe illness in high risk populations
- Small children
- Elderly
- Pregnant women
- Chronically ill
- Vaccination
- Contains killed virus
- Recommended for at-risk populations
- Healthcare workers
- Children up to 5
- Elderly
- Pregnant
- COPD
- The serotype of the influenza virus changes all the time -> WHO must try to predict which serotype will cause epidemic every year and produce vaccine against that type
- For every year the vaccine is taken the more efficient it becomes
- Preventative measures
- Hand hygiene
- Covering mouth and nose when sneezing, use tissues
- Self-isolation when symptoms occur
- Avoid close contact with sick people
Mumps
- Mumps virus
- Clinical features
- Meningitis
- Pancreatitis
- Encephalitis
- Orchitis – male infertility
- MMR vaccine
26. Characteristics, types, occurrence and prevention of enteric infections
Gastrointestinal infections
- Caused by viruses, bacteria, protozoa and helminths
- Symptoms can be caused by the organisms themselves or by toxins they produce
- If small intestine is affected:
- Watery diarrhoea
- Abdominal cramps
- Vomiting
- If large intestine is affected
- Bloody diarrhoea
- Lower abdominal pain
- Fever
- Infection acquired from contaminated food or drinking water, or from person-to-person as a result of poor hygiene
Diarrhoeal disease
- Epidemiology
- Diarrhoeal disease is the second leading cause of death in children under five
- Kills 500 000 children yearly
- Very common in developing countries
- Causes
- Non-inflammatory diarrhoea
- Norovirus
- Rotavirus
- Food intoxication
- S. aureus
- B. cereus
- C. perfringens
- Foodborne infection
- ETEC
- Vibrio cholerae
- Protozoal
- Giardia lamblia
- Cryptosporidum
- Inflammatory diarrhoea
- EHEC
- EIEC
- Clostridium difficile
- Shigella
- Salmonella
- Campylobacter
- Yersinia enterocolitica
- Entamoeba histolytica
- Non-inflammatory diarrhoea
- Prevention
- Exclusive breastfeeding
- Vaccines
- Clean water
- Correct food handling
- Hygiene
- Treatment:
- Clean water
- Salt
- Sugar
- Zinc tablets
- Risk factors
- Children
- Elderly
- Pregnant
- Malnutrition
- Immunosuppression
- Working with infected people
- Socioeconomic risk factors
- Poverty
- Overcrowding
- Poor sanitation
- Water contamination
- Poor food hygiene
Types of foodborne illness
- Intoxication
- Ingestion of a toxin which causes the illness
- S. aureus
- B. cereus
- Toxico-infection
- Ingestion of a microorganism which produces toxin in the human body
- The toxin causes the illness
- Clostridium perfringens
- Clostridium botulinum
- Infection
- Ingestion of a microorganism which itself causes illness
- Salmonella
- Shigella
- Hepatitis A
- Enteric parasites
- Trichinella
- Taenia
Prevention of foodborne illness
- Most foodborne illness is caused by food being improperly prepared or handled at home
- Sick people should not handle food
- Vegetables and fruits should be rinsed under water
- Five keys to safer foods
- Keep hands, surfaces and equipment clean. Wash hands before handling food
- Separate raw and cooked foods – don’t use same equipment for both
- Cook thoroughly – especially meat, eggs and seafood
- Keep food at safe temperatures
- Don’t leave cooked food in room temperature for more than 2 hours
- Refrigerate cooked food as soon as possible
- Do not store food too long
- Do not thaw frozen food at room temperature, rather in the fridge
- Use safe water and raw materials
27. Epidemiology and prevention of enteric bacterial infections
Enteric bacterial infections
- Non-inflammatory diarrhoea (often watery)
- Preformed toxin
- Staphylococcus aureus
- Bacillus cereus
- Bacteria that produce toxin in the intestines
- Enterotoxigenic E. coli (ETEC)
- Vibrio cholerae
- Clostridium botulinum
- Clostridium perfringens
- Preformed toxin
- Inflammatory diarrhoea (often bloody)
- Bacteria that produce cytotoxins
- Enterohaemorrhagic E. coli (EHEC)
- Clostridium difficile
- Bacteria that invade the mucosa
- Shigella
- Salmonella
- Campylobacter
- Enteroinvasive E. coli
- Yersinia enterocolitica
- Bacteria that produce cytotoxins
Clostridium botulinum
- Causes botulism
- Bacteria proliferates and produces toxin in improperly canned foods, preserved meat
- Clinical features
- Descending, flaccid paralysis
- Toxin inhibits release of acetylcholine in the neuromuscular junction
- Prevention
- Proper heating of food before
Staphylococcus aureus
- Bacterium enters food from the nasal discharge or skin of food handlers
- Lives in salads, ham, eggs, dairy products
- Produces toxin which is ingested
- Clinical features
- Diarrhoea
- Vomiting
Clostridium perfringens
- Toxin is found in meat which is not sufficiently cooked
- Clinical features
- Diarrhoea
Bacillus cereus
- Produces spores which survive cooking
- Food left too long in room temperature -> spores start to proliferate and produce toxin
- Often associated with rice stored at room temperature
- Clinical features
- Diarrhoea
- Vomiting
- Prevention
- Food should be cooked rapidly and then cooled rapidly, not allowed to remain warm for long itme
Campylobacter jejuni
- Epidemiology
- Outbreaks during summer
- Common in EU
- Bacteria ingested through
- Contaminated food or water
- Undercooked meat
- Raw milk
- Clinical features
- Bloody diarrhoea
- May cause Guillain-Barré syndrome
- Prevention:
- Thoroughly cooking the food
- Pasteurizing milk
Salmonella
- Most commonly salmonella enteritidis, typhimurium
- Reservoir
- Poultry
- Pigs
- Cattle
- Ingested through undercooked or contaminated meat or eggs
- Acid labile bacteria
- Healthy adults need to ingest many bacteria to be infected
Enterohaemorrhagic E. coli (EHEC)
- Most important serotype – O157:H7
- Very similar bacterium: Shiga-toxin producing E. coli (STEC)
- Reservoir
- Cattle
- Sheep
- Ingested through
- Person-to-person
- Undercooked ground meat
- Raw milk
- Clinical features
- Causes severe disease
- Bloody diarrhoea
- Fever
- May cause haemolytic uraemic syndrome in children, elderly
- Prevention
- It’s heat-sensitive
Enterotoxigenic E. coli (ETEC)
- Epidemiology
- Major cause of infantile diarrhoea
- Causes traveller’s diarrhoea in visitors to endemic countries
- One of the top four pathogens causing severe diarrhoea in children < 5
- Ingested through contaminated food or water
- Clinical features
- Self-limiting
- Mild diarrhoea
- Can cause dehydration in young children
Shigella
- S. sonnei, S. dysenteriae, etc.
- Epidemiology
- Uncommon in EU, common in developing countries
- 60% of deaths occur in children < 5
- One of the top four pathogens causing severe diarrhoea in children < 5
- Transmitted faecal-oral or via contaminated food or water
- Clinical features
- Produce Shiga toxin
- Causes dysentery (mucoid-bloody diarrhoea)
- High fever
- Can cause haemolytic uraemic syndrome in children and elderly
- No vaccine
Cholera
- Vibrio cholerae
- Affects both children and adults
- Transmission by
- Contaminated water
- Due to non-segregated sewage and drinking water
- Undercooked seafood
- Contaminated water
- Clinical features
- Produces cholera toxin
- Can kill within hours
- Mortality 80% untreated, 1% treated
- Watery diarrhoea 20 – 30 times a day
- Treatment
- 80% of cases can be treated with oral rehydration + salts
- Prevention
- Acid-labile bacterium
- Providing safe water and sanitation is the most important factor in preventing cholera
- Having oral rehydration prepared in case of outbreak
- Oral cholera vaccine
- Should not replace the other preventative measures
Typhoid fever
- Salmonella typhi or paratyphi
- Epidemiology
- Absent from industrialized countries
- Big problem for poorer countries
- Transmission
- Spread faecal-orally
- Clinical features
- Persistent fever
- Headache
- Abdominal pain
- Constipation or diarrhoea
- GI bleeding
- Vaccine
- Exists for salmonella typhi but not for paratyphi
- Oral and injectable
28. Epidemiology and prevention of enteric viral infections
Viral enteric infections
- Rotavirus
- Norovirus
- Poliovirus
Rotavirus
- Epidemiology
- The leading cause of severe diarrhoeal disease in infants and children worldwide
- Most common cause of diarrhoeal deaths in developing countries
- Most common during the winter in temperate climates
- Year-round in tropical climates
- Virtually all children in developing countries are infected before they reach age 3
- RV can also infect adults
- Especially institutionalized and hospitalized
- Transmission
- Spreads rapidly among nonimmune children
- Faecal-oral
- Respiratory droplets
- Contaminated objects
- Symptoms
- Watery diarrhoea
- Vomiting
- Abdominal pain
- Vaccine
- Live attenuated oral vaccine
- Childhood vaccine
- At week 6 and month 3
Norovirus
- A calicivirus
- Epidemiology
- Most common cause of winter gastroenteritis (stomach flu)
- Most common cause of adult gastroenteritis
- Common in developed and developing countries
- Outbreaks common in
- Nursing homes
- Hospitals
- Cruise ships
- Transmission
- Faecal-oral
- Person-to-person
- Virus can survive freezing and heating to 60 degrees
- Virus can shed in asymptomatic people for 2 weeks
- Clinical features
- Self-limiting
- Diarrhoea
- Vomiting
- Abdominal cramp
- Diarrhoea
- Fever
- No vaccine
Poliovirus
- Epidemiology
- Mainly affects children under 5
- In pre-vaccine era virtually all children had polio in their life
- Transmission
- Humans are the only known reservoir
- Faecal-oral
- Clinical features
- 95% develop very mild, flu-like symptoms
- 4% may develop aseptic meningitis, myalgia
- 1% develop paralytic poliomyelitis
- Treatment
- Mild cases are self-limiting
- No cure for severe form
- Surveillance for acute flaccid paralysis
- = the gold standard for detecting poliomyelitis
- Prevention
- Vaccine
- Clean water
- Hygiene
- Oral polio vaccine (Sabin)
- Used in countries with high incidence of polio, or neighbours with high incidence of polio
- Live attenuated
- Gives long-lasting immunity
- Gives immunity at the mucous membranes of the intestines
- The attenuated virus can be excreted in faeces and immunize other people
- Has a small risk of vaccine-associated paralytic polio
- Inactivated polio vaccine (Salk)
- Used in most countries
- Killed virus
- Given by IM injection
- No risk of vaccine-associated paralytic polio
- More expensive
29. Epidemiology and prevention of enteric helminth and protozoon infections
Enteric helminth and protozoa infections
- Pinworms
- Giardia
- Amebiasis
- Ascariasis
- Tapeworms
- Whipworm
Pinworms
- Parasite: Enterobius Vermicularis
- Epidemiology
- Outbreaks common in schools
- Transmission
- Faecal-oral
- Clinical features
- Key symptom: itching at the rectum
- Parasites leaves the anus at night, leaves eggs around the anus
- Diagnosis
- Put tape at the anus, look for eggs in the morning
- Treatment:
- Vermox
- Antiminth
Giardiasis
- Parasite: Giardia lamblia
- Epidemiology
- Very common water-borne infection
- Transmission
- Faecal-oral transmission
- Lives in the upper GI tract
- Clinical feaatures
- Diarrhoea
- Abdominal pain
- Flatus
- Steatorrhea
- Diagnosis
- Microscopy of stool to look for cysts
Amebiasis
- Protozoa: Entamoeba histolytica
- Epidemiology
- Found in 4% of the population
- Transmission
- Faecal-oral
- Invades the mucosa of coecum and ascending colon
- Clinical features
- Can be asymptomatic
- Diarrhoea
- Abdominal pain
- Flatus
- Can travel to liver, causing hepatitis
Ascariasis
- Helminth: Ascaris lumbricoides (the large intestine round worm)
- Epidemiology
- The most common helminth infection worldwide
- Mostly affects children in developing and tropical countries
- Transmission
- Transmitted by contaminated food
- Penetrate the intestine, invades liver, lung, heart
- Symptoms
- Can be asymptomatic
- Invasion of lungs -> causes Loeffler syndrome
Tapeworms
- Helminth: Taenia solium
- In raw or undercooked pork or beef
- Can be 25 meters in length
- Cysticercosis -> cysts of larvae in any organ, especially in the brain
Whipworm
- Helminth: Trichuris trichiura
- Epidemiology
- Very common parasitic infection in the US
- Transmission
- Faecal-oral transmission
- Worm lives in coecum and appendix
- Female produces thousands of eggs every day
- Clinical features
- Often asymptomatic
- Allergic reactions
- Anaemia
- Diarrhoea
30. Epidemiology and prevention of viral hepatitides
Risk factors for hepatitis viruses
- Low socioeconomic status
- Crowding
- Poor sanitation
- Lack of safe water
- IV drug users
- People with many sexual partners
- People who receive regular blood transfusions
Prevention
- Primary
- Hygiene
- Safe handling and disposal of needles
- Provide sterile injection equipment to IV drug users
- Testing donated blood
- Promote safe sex
- Secondary
- Screening high-risk people for cirrhosis, HCC
- Tertiary
- Early and appropriate treatment
Hepatitis A
- Epidemiology
- Especially in tropical countries
- In developing countries most children < 10 have been infected
- Common in those who travel abroad
- Transmission
- Faecal-oral transmission
- Direct contact
- Clinical features
- Young children are asymptomatic
- In developing countries most children are affected before age of 10
- Adults are commonly symptomatic
- Self-limiting, low mortality
- Cannot progress to chronic hepatitis
- Young children are asymptomatic
- Vaccine
- For travellers to endemic areas
- For men who have sex with men
- People with underlying liver disease
Hepatitis B
- Epidemiology
- Causes many deaths worldwide
- Vaccine-preventable disease
- Low prevalence in Europe
- 90% of infected infants develop chronic infection
- 25% of infected infants die
- Transmission
- Vertical
- Blood transfusion
- Sexually
- Between IV drug users
- Clinical features
- Acute infection
- 5 – 10% become chronic
- Diagnosis
- Serology – HBsAg, antibodies
- Prevention
- Promote safe sex
- Needle exchange programmes for IV drug users
- Screening in high-risk groups
- Subunit vaccine
- HBsAg antigen
- Post-exposure chemoprophylaxis
- Passive immunization (immunoglobulins)
Hepatitis C
- Epidemiology
- Mostly found in Africa, East Asia
- Transmission
- Same as Hep B
- Commonly progresses into chronic hepatitis, cirrhosis and HCC
- Screening
- IV drug users
- Patients with HIV
- Health care workers after needlestick injury
- Children of HCV-infected mothers
- Sexual partners of HCV-infected persons
- Treatment
- Antiviral medication can cure 95% of infected people
- Prevention
- No vaccine
- No postexposure prophylaxis
Hepatitis D
- Requires hepatitis B for expression and replication
- Superinfection of Hep D on hep B causes more severe acute illness and more often chronic hepatitis
- Can be prevented with hepatitis B vaccination
Hepatitis E
- Epidemiology
- Common in tropical countries
- Very similar to hep A
- Clinical features
- Cannot progress to chronic hepatitis
- Except serotype 3
- Can cause fulminant hepatitis in people with liver disease or pregnant women
- Cannot progress to chronic hepatitis
- No vaccine available (only in China)
31. Epidemiology and prevention of haematogenic and lymphogenic infections
Vector-borne diseases
- Infections transmitted by the bite of infected arthropods like:
- Flies
- Sleeping sickness
- Mosquitoes
- Malaria
- Yellow fever
- Zika
- Dengue fever
- West Nile fever
- Ticks
- Lyme disease
- Tick-borne encephalitis
- Q fever
- Tularaemia
- Lice
- Fleas
- The plague
- Flies
- The infection can be located inside the vector or outside
- Arthropods are cold-blooded and are therefore very sensitive to changes in the climate
- Climate change changes their habitat -> can make areas previously spared from these diseases become affected
- Prevention
- Protective clothing
- Insect repellant
- Regularly examine the skin for ticks
- Avoid endemic areas
- Remove ticks safely
- Insect nets
Lyme disease
- Borrelia burgdorferi, afzelii and garinii
- Epidemiology
- Endemic in most of Europe, most in central and eastern European countries
- Transmission
- By bite of the Ixodes tick
- Reservoir
- Many small mammals
- Ground-feeding birds
- Symptoms
- Target-shaped rash (erythema migrans)
- Myocarditis
- Neuroborreliosis
- Lyme arthritis
- Prevention
- No vaccine
- Avoiding tick bites
- Early removal of attached ticks
Tick-borne encephalitis
- An arbovirus (= transmitted by arthopod) and a flavivirus (= the genus it belongs to)
- Epidemiology
- Endemic in areas of Europe and Asia
- Most cases occur during the summer
- Transmission
- By bite of the Ixodes tick
- Reservoir
- Small rodents
- Clinical features
- Few infected people get sick
- Illness is worst in elderly
- Neurological symptoms, sometimes permanent
- Prevention
- Vaccine exists
- Avoiding tick bites
- Early removal of attached ticks
Malaria
- Parasites of the genus plasmodium
- Plasmodium falciparum – most severe
- Plasmodium ovale
- Plasmodium vivax
- Epidemiology
- Most cases are in Africa, especially Nigeria and Congo
- Major cause of death in developing countries
- Transmission
- By mosquitoes (Anopheles species)
- Entomologic inoculation rate = how many infectious mosquitoes bites per person per year
- A measure of transmission intensity
- High if above 50
- The higher the EIR, the greater the burden of malaria
- Rarely by blood transfusion, needle sharing, etc.
- Reservoir
- No animal reservoir
- Only lives in humans
- Risk groups for severe disease
- Pregnant women
- Children and infants
- HIV infected
- Prevention
- Chemoprophylaxis:
- For travellers to malaria endemic countries
- For high-risk residents of endemic countries
- Kill mosquitoes
- Insect nets
- Clothes that cover the body
- Mosquito repellent
- Chemoprophylaxis:
- Vaccine
- Name: RTS,S
- Very recent (2019)
- Against plasmodium falciparum
Crimean-Congo haemorrhagic fever (CCHF)
- CCHF virus, a type of nairovirus
- Endemic in Africa, Balkans, Middle East, Asia
- Transmission by tick
- Symptoms
- Up to 80% lethality
- Fever
- Diffuse bleeding
- Diarrhoea
- Petechiae
Tick-borne relapsing fever
- Caused by several spirochaetes
- Transmission by tick
- Symptoms
- Relapsing fever
- Headache
West Nile virus
- A flavivirus
- Epidemiology
- Originated from Africa, now present worldwide
- Reservoir
- Birds
- Transmission
- Mosquitoes
- Symptoms
- Often asymptomatic
- Most commonly mild infection flu-like symptoms and rash
- Rarely meningitis or encephalitis
- Prevention
- Protect against mosquito bites
Japanese encephalitis
- Japanese encephalitis virus
- Epidemiology
- Main cause of viral encephalitis in many parts of Asia
- Reservoir: birds
- Transmission by mosquitoes
- Symptoms
- Often asymptomatic
- Rarely encephalitis and neurological sequelae
- Vaccine exists
Zika virus
- A flavivirus
- Transmission by mosquito
- Symptoms
- Often asymptomatic
- Congenital zika causes CNS malformations
- Prevention
- Protect against bites
Yellow fever
- Yellow fever virus, a flavivirus
- Transmission by mosquito
- Occurs in Sub-Saharan Africa and South America
- Infants and children are at highest risk
- Clinical features
- Most patients experience mild symptoms
- 15% develop serious disease
- Haematemesis
- Bloody diarrhoea
- Jaundice
- Organ failure
- Prevention
- Vaccine
- Reccomended for those travelling to or living in areas with yellow fever transmission
- Protection against mosquito bites
- Vaccine
Lymphatic filariasis
- Also called elephantiasis
- Filarial parasites transmitted to humans through mosquitoes
- Causes severe lymphoedema
32. Epidemiology and prevention of infections transmitted through the skin
Wound infections
- Pathogen enters through a wound
- Local inflammation at site
- Risk factors
- Diabetes
- Immunosuppression
- Old or young age
- Foreign material in wounds
- Crowded conditions
- Poor hygiene
Tetanus
- Clostridium tetani
- Epidemiology
- Present worldwide
- More common in rural communities and agricultural regions
- Transmission
- Bacterium produces spores
- Contaminated objects in contact with wounds or ulcers
- Penetrating injury from contaminated object (nails)
- No person-to-person
- Reservoir:
- Soil
- Animal GI tract and faeces
- Toxins
- Tetanolysin – haemolyses. No pathological activity
- Tetanospasmin – causes symptoms of tetanus
- Clinical features
- Fatality 10 – 20% with therapy (without: 50%)
- Generalized tetanus
- Most common form
- Descending muscle rigidity
- Laryngospasm, breathing difficulty
- Risus sardonicus – smiling grin
- Opisthotonus – spasm of the back muscles
- Localized tetanus
- Tetanus symptoms in the area of the infection only
- Rare, very good prognosis
- Cephalic tetanus
- Rare, poor prognosis
- If infection occurs at head or ear
- Dysfunction of cranial motor nerves
- Neonatal tetanus
- Neonate exposed during birth
- Very poor prognosis
- Treatment
- Supportive care
- Protection of the airways
- Neutralization of toxins (passive immunization)
- Prevention
- Toxoid vaccine (DTaP)
- Childhood vaccine
- However, protection only lasts approx 10 years, so it’s recommended to get a booster shot for high risk groups (dirty wounds, military) if it’s more than 10 years since last booster
- Clean birth
- Toxoid vaccine (DTaP)
Gas gangrene
- Clostridium perfringens, other clostridium spp.
- Risk factors
- Peripheral artery disease
- Diabetes mellitus
- Transmission
- Spores enter wounds and thrive in anaerobic environment
- Often seen after trauma (accidents) or postoperative
- Prevention
- Clean any skin injury thoroughly
- Remove foreign objects from wounds
- Give post-exposure antibiotics
Epidemic keratoconjunctivitis
- Adenovirus
- Transmission
- Direct contact with eye secretions
- Indirect contact by contaminated ophthalmic instruments
- Epidemics
- Schools
- Hospitals
- Nursing homes
- Etc.
- Prevention
- Good hygiene
- Don’t use the same ophthalmic instruments in patients with symptoms of keratoconjunctivitis and healthy patients
Trachoma
- Chlamydia trachomatis in the eye
- Epidemiology
- Major cause of blindness in developing countries
- Transmission
- Direct contact with eye discharge
- Spread by flies
- Repeated eye infections can cause blindness
- Prevention
- Sanitation of the face
- Antibiotics
Pediculosis – lice infestation
- Epidemiology
- Found in all countries and climates
- More common in developing countries
- Transmission
- Direct contact
- Indirect – via sharing objects like combs, clothes, hats
- Three types
- Pediculus capitis – head louse
- Grow in hair
- Lay eggs at the scalp
- Pediculus corporis – body louse
- Lives in clothing, not in body hair
- Pthirus pubis – pubic louse
- Grow in pubic hair
- STD
- Pediculus capitis – head louse
- Lice can be the vector of
- Rickettsia prowazeki (typhus)
- Borrelia recurrentis (relapsing fever)
- Clinical features
- Itching
- Prevention
- Don’t share stuff
- Avoid head-to-head contact
- Wash clothes at 60
Scabies
- Sarcoptes scabiei var hominis
- A mite that burrows into the epidermis, where they live and deposit eggs
- Epidemiology
- Occurs worldwide
- More common in developing countries
- Often affects children and sexually active adults
- In crowded conditions
- Reservoir
- Humans
- Transmission
- Direct contact
- Symptoms
- Itching
- Pimple-like rash
- Burrows in the skin
- Prevention
- Avoid direct contact with infected
- Objects an infected person has used should be washed
33. Epidemiology and prevention of zoonotic helminth and bacterial infections
Zoonoses
- A disease that is naturally transmissible from vertebrate animals to humans and vice versa
- > 60% of all infectious disease are zoonoses
- Bacterial
- Listeria monocytogenes
- Brucella
- Leptospirosis
- Bacillus anthracis
- Tularaemia
- Q fever
- Salmonella
- Plague
- Shigella
- Helminth
- Trichinella spiralsis
- Taenia solium
- Echinococcus
Listeriosis
- Listeria monocytogenes
- Reservoir
- Animals are often asymptomatic but have the bacteria in their feces
- Transmission
- Faecal-oral
- Also found in processed meat, soft cheese
- Can cause abortion in pregnant women
- Prevention
- Pasteurizing dairy products
- Pregnant women should avoid soft cheeses and pre-packed salads
- Hand-washing
Brucellosis
- Caused by brucella spp.
- Epidemiology
- Occurs worldwide
- Most common in Mediterranean region
- Reservoir
- Cattle
- Dogs
- Sheep
- Goats
- Pigs
- Transmission
- Direct or indirect contact with animals
- Contaminated animal products
- Symptoms
- Fever
- Arthritis
- Can infect any organ
- Heart
- Brain
- Prevention
- Vaccination of animals
- Pasteurization
Leptospirosis
- Leptospira spp
- Epidemiology
- Most common in tropical areas
- Reservoirs
- Many wild animals (rat, mouse)
- Transmission
- Direct contact with urine of infected animals
- Indirect contact with urine
- Clinical features
- Mild disease (fever, myalgia)
- Severe disease
- Rare
- High mortality
- Haemorrhages
- Acute kidney injury
- Prevention
- Controlling rodent populations
- Avoid contaminated areas
- Improve water and food storage conditions
Anthrax
- Bacillus anthracis
- Epidemiology
- Very rare in western countries (0 – 2 cases per year)
- Reservoir:
- Grass-eating animals (sheep)
- Transmission
- By exposure to spores
- Eating contaminated meat
- Through skin
- Inhalation of spore
- Clinical features
- Skin anthrax
- Most common (95%)
- If spore enters through skin
- Necrotic skin eschars
- Lung anthrax
- Very rare
- If spore is inhaled
- Haemorrhagic mediastinitis
- 75% mortality
- Gastrointestinal anthrax
- Skin anthrax
- Prevention
- Vaccination of animals
- Protective equipment in workers
Tularaemia
- Francisella tularensis
- Reservoir
- Rabbits
- Hare
- Squirrels
- Transmission
- Bite of infected insects (ticks, mosquitoes, flies)
- Contact with infected animal
- Eating undercooked infected meat
- Symptoms
- Fever
- Lymphadenopathy
Q fever
- Coxiella burneti
- Reservoi
- Sheep
- Goat
- Cattle
- Transmission
- Inhalation of aerosols with the bacterium
- Symptoms
- 50% asymptomatic
- Headache
- Fever
- Chronic Q fever
- In 1% of cases
- Endocarditis
- Hepatitis
34. Epidemiology and prevention of zoonotic protozoon and viral infections
- Viral zoonoses
- Rabies
- Hantavirus
- Influenza
- Crimean-Congo haemorrhagic fever
- Ebola
- Rift valley fever
- Protozoan zoonoses
- Toxoplasma
Rabies
- Rabies virus is a type of lyssavirus
- Epidemiology
- Very few cases in Europe
- Present in all parts of the world
- 95% of death occur in Asia and Africa
- Reservoir
- Dogs, bats, wolves, foxes
- Transmission:
- Bite or direct contact with saliva of infected animal
- Retrograde transport from nerves at bite site to the CNS
- Incubation period
- 1-3 months
- Depends on how far from the CNS the infection occurred
- Two types
- Encephalitic rabies (most common)
- CNS symptoms
- Agitation
- Confusion
- Hypersalivation
- Paralytic rabies
- Flaccid paralysis spreading from the bite wound
- Both
- Hydrophobia
- Encephalitic rabies (most common)
- Prevention
- Human vaccine
- For travellers spending much time outdoors
- For high-risk occupations, like veterinarians
- Oral immunization of animals
- Releasing baits containing oral vaccine into high-risk areas
- Vaccination of dogs
- Teaching children to avoid animal bites
- Post-exposure prophylaxis
- Washing wound for 15 minutes
- Giving rabies vaccine soon after bite
- Administration of rabies antibodies if needed
- Human vaccine
Hantavirus
- Hantavirus is a bunyavirus
- Reservoir
- Rodents
- Transmission
- Inhalation of infected rodent urine or droppings
- Bites
- Risk groups
- Forest workers
- Farmers
- Clinical features
- Haemorrhagic fever with renal syndrome
- Hantavirus cardiopulmonary syndrome
- Prevention
- Avoidance of dust
- Minimizing contact with rodents
Toxoplasmosis
- Toxoplasma gondii (a helminth)
- Reservoir
- Cats
- Transmission
- Ingestion of cysts
- Direct through cat faeces
- Indirect through food or water contaminated with cat faeces
- Pigs, cows can ingest cyst, making their meat infected
- Clinical features
- A part of TORCH
- Perinatal death
- Congenital infection
- Neurocognitive deficit
- Prevention
- Avoid contact with cat litter
- Hand hygiene
- Avoid undercooked meat
35. Epidemiology and prevention of sexually transmitted diseases (excluding AIDS)
- Epidemiology
- Chlamydia 2,5x more common in women
- Gonorrhoea slightly more common in women
- Antibiotic resistance is increasing
- STDs more frequent in Black and Asian ethnicities in western countries
- Prevention
- Primary
- Condoms
- HPV vaccination
- Primary
36. Epidemiology and prevention of AIDS
- Epidemiology of HIV and AIDS
- 34 million worldwide live with HIV
- 23 million in Africa
- Most new infections occur in Africa as well
- 1.8 million deaths worldwide due to AIDS in 2010
- 1.2 million in Africa
- Adult prevalence of AIDS in Africa: 4,7%
- After the HIV epidemic began in ~80s, the life expectancy in Southern Africa actually decreased
- HIV is primarily transmitted through sex, and primarily by men who have sex with men
- In non-African countries, black peoples are more commonly affected than other ethnicities
- For every 100 HIV+ mother there will be 35 HIV+ babies
- Complications of AIDS
- Pneumocystis pneumonia (by pneumocystis jirovecii)
- Toxoplasmosis
- Candida infection
- Tuberculosis
- Kaposi sarcoma
- Prevention
- Primary
- Antiretroviral prophylaxis for HIV-positive pregnant women
- The use of this is increasing
- Condom use
- Female condoms also exist
- Antiretroviral prophylaxis for HIV-positive pregnant women
- Tertiary
- Antiretroviral therapy to HIV-positive people
- Postexposure prophylaxis
- Primary
37. Epidemiology and prevention of prion diseases
- Prions
- = wrongly folded proteins which are very resistant, especially against heating
- The protein in question is called PrP and is normally in the C isoform (PrPC protein)
- Transformation to the Sc (scrapie) isoform can occur when a PrPC protein comes into contact with a PrPSc isoform of the protein
- It can also occur spontaneously, but that is extremely rare
- The Sc isoform is resistant to proteolysis
- Transmissible per os
- Prion diseases = transmissible spongiform encephalopathies (TSE)
- Bovine spongiform encephalopathy (BSE)
- In 🐄
- BSE epidemic occured in 80s – 90s Britain after feeding cattle with prion-contaminated meat and bone meal (MBM)
- Can be transmitted to humans
- Scrapie
- In sheep and 🐐
- Creutzfeldt-Jakob disease
- In humans
- Familal or spontaneous
- Variant Creutzfeldt-Jakob disease
- In humans
- Similar to Creutzfeldt-Jakob disease but caused by eating prion-contaminated beef (BSE)
- Kuru disease
- In humans
- Acquired through cannibalism
- Nowadays extinct after the cannabalistic Fore people in Papua New Guinea stopped funerary cannibalism
- Fatal familial insomnia
- In humans
- Bovine spongiform encephalopathy (BSE)
- Prevention
- In response to the british epidemic, import of british beef was banned worldwide (and still is many places today)
- Preventing BSE in cattle is the most important preventative measure
- Health politics must ensure correct handling and feeding of cattle
- Affected animals should be euthanized and destroyed
- Destruction of prions
- Autoclaving
- Proteases
- Denaturating agents
38. New infectious diseases. Bioterrorism
- New infectious diseases
- COVID-19
- H1N1 influenza
- Caused 1918 pandemic (Spanish flu) and 2009 pandemic (swine flu)
- SARS
- Zika virus
- Multi-drug resistant tuberculosis
- Bioterrorism
- = the use of microorganisms or their products to cause harms
- Characteristics of bioterrorism agents which make them appealing to terrorists
- Inexpensive
- Readily available
- Easy to produce in quantity
- Can be transmitted between humans
- Hard to treat
- Potential bioterrorism agents are classified into categories, based on their risk
- Category A – highest risk
- Easily disseminated and transmitted
- Has high mortality rates
- Difficult to treat
- Difficult to prepare against
- Examples
- Tularaemia
- Anthrax
- Smallpox
- Botulism
- Bubonic plage
- Viral haemorrhagic fevers
- Category B – second highest risk
- Brucellosis
- Q fever
- Typhus
- Viral encephalitis
- Category C – third highest risk
- Can be engineered for use in bioterrorism
- Nipah virus
- Hantavirus
- Prevention
- National preparedness
- Limit availability of possible bioterrorism agents
Is it really true that pneumonia has a 57% mortality while sepsis has a 23% mortality? This seems odd to me
It might not be as high as 57%, but remember that this is for healthcare-associated pneumonia, not regular pneumonia.
On the other hand, inpatients are usually regularly screened for sepsis with qSOFA or NEWS, which may contribute to the relatively low sepsis mortality rate. I can’t recall where I got the numbers, but I assume from the lecture.
Hi! For the topic “20. Nosocomial infections. Sterilization, disinfection” – I failed because I did not know the sterilization and disinfection in detail, everything from them documenting every step (in case of infection, or a potential lawsuit) what type of methods, phenol-coefficient, Joseph Lister, what kind of methods you would use to sterilize fluids to before you administer it (autoclave), biological indicators, etc. Obviously my own fault not remembering it from micro, but maybe it would be wise to add a little footnote to study this! 🙂 And for the topic “Health politics” from PH1 they wanted to know mostly about primordial and primary health prevention, if that is useful in any way (since those notes are a little bit short). For primordial prevention they wanted me to answer stuff like make laws against smoking, increase taxes on sugar and alcohol, improve city infrastructure, reduce pollution, vaccination programs. They were laughing a little bit when I answered “increase the socioeconomic status of the population” and commented that it would be great but maybe not that possible in practice 🙁 That was all, enjoy your first day as a graduate!!!! 🙂 Thank you for all the work you have done here, I would have repeated a hundred years if it was not for you, and I know I am speaking for most POTE-students when I say that. Thanks <3
Thank you for the detailed information! Added it to the notes.
<3
“Adult prevalence of WHO in Africa: 4,7%”
I hope that we one day will find a cure for this atrocious disease! #eliminateWHO
Hahah. As funny as it is, I should fix ut so people don’t get confused. Thanks for the laugh tho
Tetanus toxin is not just for high risk groups. It’s mandatory for everyone. He failed me for that 🙁
Tetanus is both a childhood vaccine (in DTaP) and a high-risk vaccine. I’ve added some words to explain it.
Sorry you failed.
Hello , I hope you are doing well 🙂 <3
Did you write topic 13 according to the lecture 🙂 ?
Thank you and good luck with your exams
I write all topics according to lecture or seminar in most subjects, unless they’re not available, in which case I use other sources. I don’t remember exactly for this topic but I think there was a lecture or seminar for it. Is there a reason you’re asking?
Thanks for your replay <3
No But other sources are totally different 🙁 and i like yours more , but its so hard to study a subject 2 times and I just wanna make sure that yours is from he department's lecture or seminars , also topic 15 16 17 ? are they the same?
Like I said, I’m pretty sure but I can’t remember exactly for all topics. If there were lectures and seminars available when I wrote them, then I used them. You can check the lectures and seminars on Potepedia yourself and compare to see which notes are most similar to the lectures.
Has anybody ever shopped at Doc’s Vape-n-K’s Vapor Store in 56 Bradshawgate?
That’s odd, someone else asked almost the exact same question earlier.
In order to determine the best trimmer for balls, you will have to decide how much of the area you would like to trim, and what style of blades best suites you. There are three main styles of pubic shavers. Each offers different options in trimming pubes.
How did public health 4 make you think of ball trimmers?
FYI its Giardia lamblia. Everywhere you have it written it says lambila.
But that’s harder to pronounce!
Fixed.
Hello , I have my exam tomorrow , but anyway do you think we really need to know the symptoms of the infections ?
Thanks in advance <3
To some degree at least, yes. But not very specific.
Good luck! You’ll nail it. <3
Edit: I failed my first chance in PH6 because I didn't know the clinical features of diphtheria and pertussis infections well enough. So disregard what I said, you should learn the symptoms!
Hey, this is so helpful thank you! not to sound rude, but will this be enough to pass the exam, cause some of the topics are rather short 😛 do they expect much more then what is written do you think? 🙂
Nobody can tell you upfront exactly what is enough and what isn’t enough to pass the exam. I have faith in the notes and believe they should be enough, but I obviously can’t guarantee it. In my opinion the ideal thing to do would be to read my notes and then the lectures to fill in the gaps, but this is POTE – even after reading through lectures and seminars you might not know everything they ask.
And no, they usually don’t expect a lot in public health.
Hello
i hope you are doing well !! do you think we need to memorize the names of the studies/trials ?
Don’t think the names are so important, no.
Stay safe!
you too <3 <3