Table of Contents
Page created on November 6, 2019. Last updated on December 18, 2024 at 16:55
Structure of the microcirculation
The microcirculation is the blood flow in the smallest vessels, the arterioles, metarterioles, capillaries, and venules. It is at the level of the microcirculation where nutrients and gases are exchanged with the tissues.
Blood flows from the arterial system and ends in the arterioles. So-called metarterioles branch off from the arterioles and connect the arterioles and the venules. Capillaries branch off from the metarterioles. At the point where the capillary originates from a metarteriole there is a muscular structure called the precapillary sphincter. By adjusting the tone of the precapillary sphincter tissues can regulate how much perfusion they receive.
If a tissue doesn’t require as much blood, the precapillary sphincters will contract. Blood will then not pass through the capillaries and instead flow directly from the arteriole to the venule through the metarteriole.
If a tissue requires more blood the precapillary sphincters will relax. Blood will then flow though the capillaries, where nutrients and gases are exchanged to the tissues.
The pressure difference between the arterioles and the venules also affects the capillary circulation. By increasing the pressure difference a tissue can increase its capillary circulation.
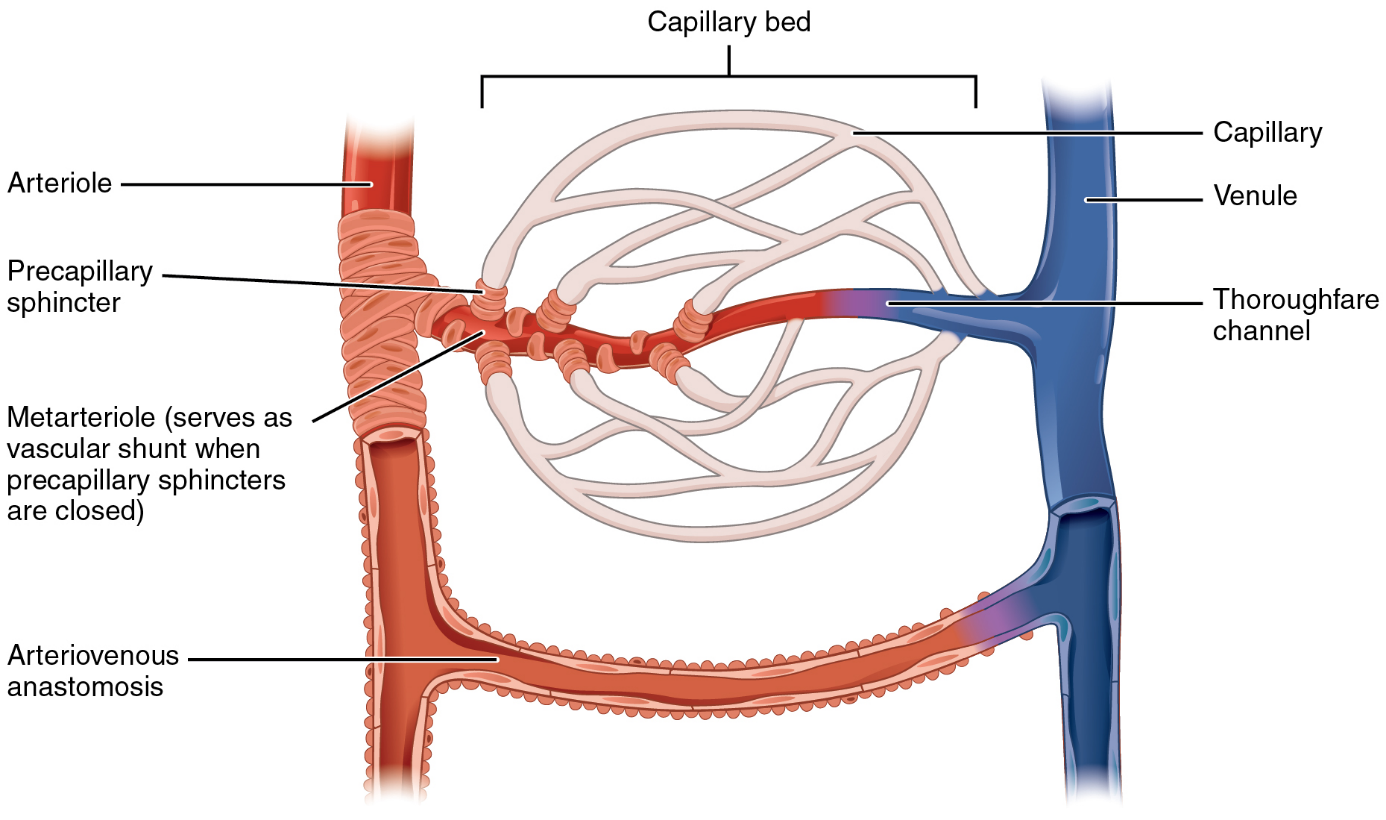
Structure of the microcirculation. From https://en.wikipedia.org/wiki/Metarteriole
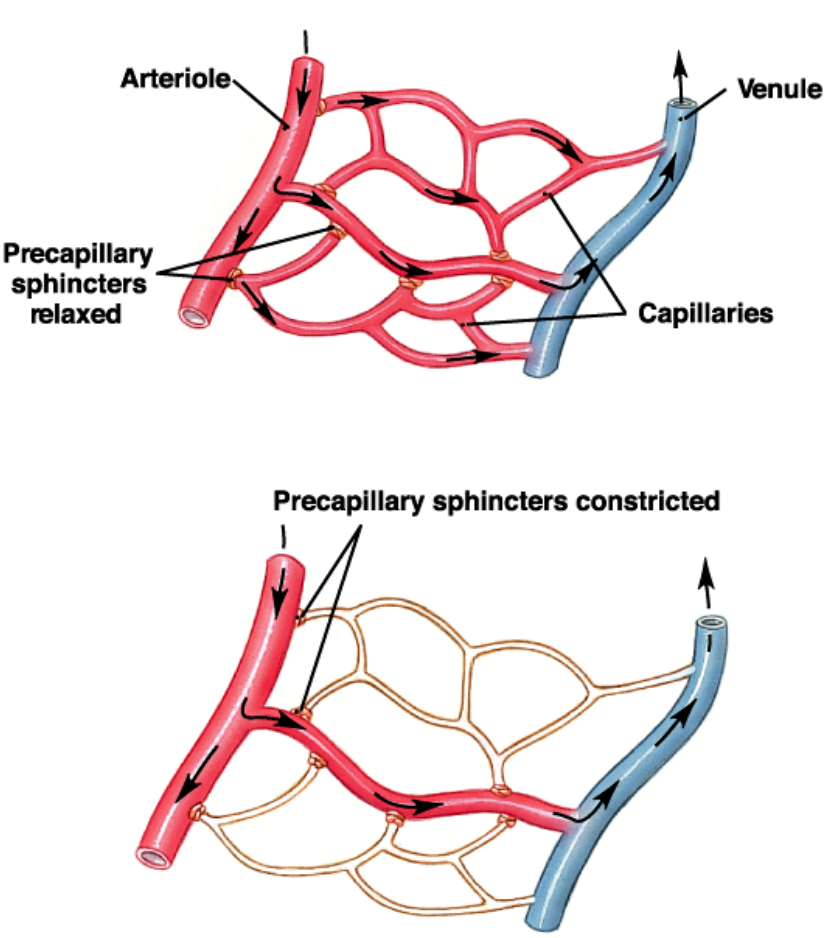
How blood flow in the capillaries varies with the precapillary sphincter tone.
Capillaries
Capillaries don’t have smooth muscle. They consist of a single layer of endothelial cells surrounded by a basement membrane. Between the endothelial cells are so-called pores or clefts. The lumen of the capillaries is 4 – 9 µm, barely enough for RBCs to squeeze through, thanks to their flexibility.
Passage of substances across the capillary wall:
For nutrients and gases to reach the tissues they must cross the capillary vessel wall. The exact way the molecule crosses the vessel wall varies depending on the properties of the molecule.
Small water-soluble substances like water, glucose and amino acids pass through the small pores.
Large water-soluble substances cross by a process called pinocytosis.
Lipid-soluble substances, including O2 and CO2, diffuse directly through the capillary wall.
Structure of capillary wall in different organs:
In the capillaries in the brain the pores are very small. The endothelial cells are continuous and are bound together by tight junctions. This allows only extremely small molecules to pass into or out of the brain.
In the capillaries of the liver the pores are very large. The endothelial cells are discontinuous, with large pores between them. This allows almost all molecules in the plasma to leave the blood and enter the interstitial space. This is necessary for the liver to detoxify the blood.
In the kidney the capillaries have fenestrae instead of pores. These fenestrae are not pores between the endothelial cells but rather holes through the endothelial cells. These fenestrae allow large amounts of small molecules to cross the capillary membrane. This is essential for the kidney to filter the blood.
The rate of fluid flow across the capillary wall; the Starling forces:
Because the capillaries are permeable to water, plasma fluid (mostly water) will leave and enter the capillaries. If exactly the same amount of water enters and leaves the capillaries there is no net fluid flow or movement. If more water leaves the capillaries that entering the capillaries there is a net fluid movement out of the capillaries. Let’s see which factors determine the net fluid movement.
The rate of flow of plasma fluid across the capillary wall depends on four forces. These forces determine whether there will be a net fluid movement out of the capillaries into the tissues or a net fluid movement out of the capillaries into the tissues. These forces are called Starling forces. The Starling forces are related to the net fluid movement by the Starling equation.
Two of the Starling forces are hydrostatic forces and two of them are colloid forces. The Starling equation looks like this:
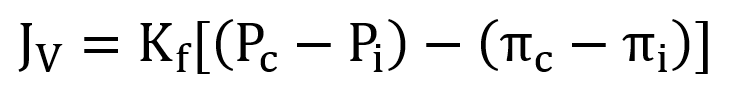
or
![]()
JV is the net fluid flow. If JV is positive, there is net fluid movement out of the capillary into the tissues. This is called filtration. If JV is negative, there is net fluid movement out of the tissues into the capillaries. This is called absorption.
Kf is the filtration coefficient. It refers to the permeability of the capillary wall, which can be regulated by many factors we’ll look at later.
Pc is the capillary hydrostatic pressure. It is determined by the hydrostatic pressure in the arteries, arterioles, venules or veins. When the hydrostatic pressure in any of these vessels increases the hydrostatic pressure in the capillaries will also increase.
Pi is the interstitial hydrostatic pressure, the hydrostatic pressure in the interstitial space. It is normally 0 mmHg.
πp is the capillary colloid pressure. The colloid pressure depends on the concentration of proteins in the blood. When the concentration of proteins in the blood decreases the capillary colloid pressure decreases, which favours filtration of fluid.
πi is the interstitial colloid pressure. It depends on the concentration of proteins in the interstitial space, which is usually very low.
The net fluid flow is usually slightly positive, which means that normally more fluid exits the capillaries than entering it, causing there to be a net outward flow of fluid (filtration). This excess fluid enters the lymphatic vessels, which eventually drains into the systemic circulation.
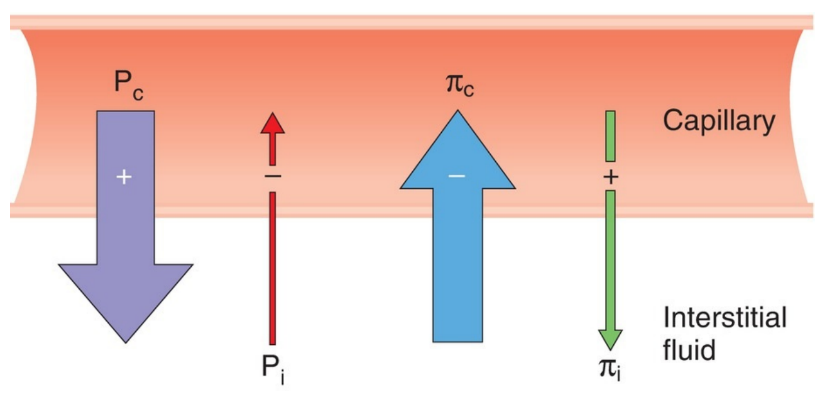
Illustration of the four Starling forces and which direction the forces work. From BRS.
Regulation of capillary permeability
The capillary permeability (Kf in the Starling equation) can be increased or decreased depending on whether filtration or absorption in the capillaries is desirable.
By contracting the endothelial cells of the capillary wall, which increases the size of the pores, the capillary permeability can be regulated. Several molecules can increase the capillary permeability by this way:
- Histamine
- Serotonin
- Bradykinin and other kinins
- Leukotrienes
Oedema
Oedema (edema) refers to increased amount of interstitial fluid, which causes the interstitium to swell. It occurs if for any reason the capillary filtration increases so much that the lymphatic system doesn’t have the capacity to drain the excess interstitial fluid. This causes interstitial fluid will accumulate and therefore swelling of the interstitium.
Oedema usually occurs when:
- The plasma protein concentration decreases, so the πp decreases, which increases JV
- The venous pressure increases, so the Pc increases, which increases JV
- Something causes the capillary permeability (Kf) to increase, which increases JV