Table of Contents
Page created on November 9, 2019. Last updated on December 18, 2024 at 16:55
Anatomy of the respiratory system
The respiratory system is comprised of two parts; the upper respiratory tract and the lower.
The upper respiratory tract includes the:
- Nose
- Nasal cavity
- Oral cavity
- Pharynx
- Larynx
- Trachea (until the bifurcation)
The lower respiratory tract includes the:
- Bronchi
- Bronchioli
- Cartilaginous bronchioli
- Membranous bronchioli
- Respiratory bronchioli
- Alveolar ducts
- Alveoli
The respiratory bronchioli, alveolar ducts and alveoli are where gas exchange occurs, so they’re sometimes called the “exchange zone”. Most of gas exchange occurs in the alveoli.
Inspiration
Breathing is comprised of two parts; inspiration and expiration.
Inspiration is an active process, meaning that it requires muscle contraction and therefore energy. The most important muscle for inspiration is the diaphragm, and the diaphragm is the only muscle used to breathe when breathing normally. External intercostal muscles and the so-called accessory breathing muscles can assist the diaphragm in inspiration if forceful inspiration is needed, such as during exercise or difficulty breathing.
The lungs don’t inflate themselves. Air doesn’t enter the lung because air is forced down the trachea. Instead, air is sucked into the lungs through the trachea when the thoracic cavity expands. When the thoracic cavity expands the lungs expand with it. This creates a negative pressure inside the lungs, which “sucks” air into the lungs through the mouth and nose.
When the diaphragm contracts the abdominal contents are pushed downward and the ribs are lifted upward and outward. This increases the volume of the thoracic cavity, which sucks air into the lungs.
Expiration
Unlike inspiration, expiration is normally a passive process. The thoracic wall is elastic. As the thoracic cavity expands and air enters the lungs the thoracic wall is stretched. Because the wall is elastic it will return to its resting position and length as soon as the diaphragm relaxes after inspiration is complete. This compresses the thoracic cavity, forcing air out of the lung without the use of any muscles.
During exercise expiration becomes an active process. During expiration the abdominal and internal intercostal muscles will contract, which compresses the thoracic cavity, forcing air out of the lungs through the mouth and nose.
In cases where there is increased airway resistance, which makes it more difficult for air to leave the lungs, expiration also becomes an active process. This occurs in the case of asthma and chronic obstructive pulmonary disease (COPD).
Compliance
We already discussed the concept of compliance when talking about vessels, but the concept is also important for the lungs.
Compliance refers to how much pressure is necessary to inflate the lung by a certain amount of air. The higher the compliance, the less pressure is necessary to inflate the lung. Compliance is inversely proportional with elastic resistance. When elastic resistance increases the compliance decreases. You can think of compliance as the opposite of “stiffness”.
The normal value of compliance of the lung is 2 L/kPa. This means that a pressure of 1 kilopascal will fill the lungs with 2 litres of air.
The concept of compliance is important because the compliance of the lung changes in different lung diseases. It can either increase or decrease, depending on the disease. In the disease emphysema the compliance increases while in pulmonary fibrosis the compliance decreases.
Intrathoracic pressures
The pressure in the atmosphere is 760 mmHg. When we talk about positive or negative pressures, we refer to pressures which are larger than or smaller than 760 mmHg, respectively.
The intrapleural or intrathoracic pressure is always negative, meaning that it’s less than the atmospheric pressure. It is because the pressure inside the thorax is negative that the lung expands while the thoracic cavity does too.
The intraalveolar or simply alveolar pressure is the pressure of air inside the alveoli. During inspiration the alveolar pressure decreases, which is what sucks air into the lungs and alveoli. During expiration the alveolar pressure increases, which pushes air out.
Spirometry
Spirometry is the most common test used to measure pulmonary function. It measures the volume of air which can be inhaled and exhaled and the speed of airflow. More specifically, spirometry allows us to measure the so-called static and dynamic lung parameters.
The static parameters include 4 different lung volumes and 4 different the lung capacities. Spirometry can measure all lung volumes except the residual volume. It also cannot measure any lung capacity which includes the residual volume.
The dynamic parameters are those which depend on the speed of airflow.
The lung parameters depends on a lot of physiological factors, like age, height, weight and gender.
Lung volumes and capacities
The volumes of the lungs change during the breathing cycle. We can define 4 different lung volumes and 4 different lung capacities.
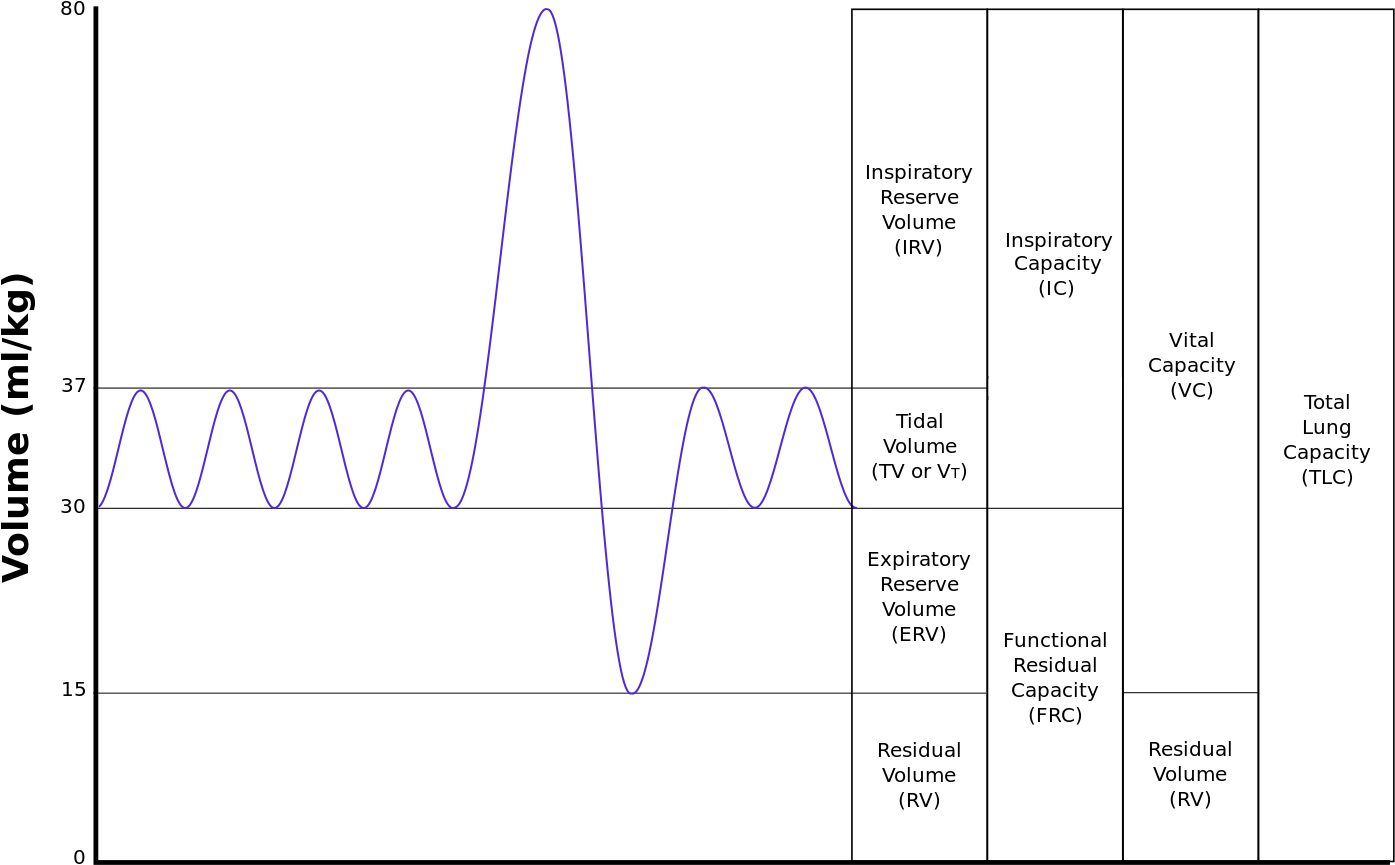
The tidal volume (TV) is the volume of air which is inhaled and exhaled normally with every breath during rest. It is normally 500 mL.
The inspiratory reserve volume (IRV) is the maximum amount of air which can be inhaled after a normal inhalation. During exercise the body’s need for oxygen increases and so the lungs inhale more air with each breath, corresponding to the inspiratory reserve volume. It’s normally 3000 mL, meaning that you can normally inhale 3 more litres of air after a normal inspiration.
The expiratory reserve volume (ERV) is the maximum amount of air which can be exhaled after a normal exhalation. It’s normally 1000 mL, meaning that you can normally exhale 1 more litre of air after a normal expiration.
The residual volume (RV) is the volume of air remaining in the lungs after the most forceful expiration possible. It is normally 1200 mL, meaning that 1.2 litres of air remain in the lungs after you’ve exhaled as hard as you possibly can. It’s the only volume which cannot be measured by spirometry.
The lung capacities are combinations of two or more lung volumes.
The inspiratory capacity (IC) is the maximum amount of air which can be inhaled after a normal exhalation. It’s the sum of the tidal volume and the inspiratory reserve volume. It’s normally around 3500 mL.
The functional residual capacity (FRC) is the amount of air which remains in the lung at the end of a normal expiration. It’s the sum of the expiratory reserve volume and the residual volume. It’s around 2300 mL.
The vital capacity (VC) is the maximum amount of air a person can exhale after first filling the lungs to their maximum extent. It’s the sum of the inspiratory reserve volume, tidal volume and expiratory reserve volume. It’s around 4600 mL. It’s sometimes called forced vital capacity (FVC).
The total lung capacity (TLC) is the maximum volume to which the lung can be expanded with the greatest possible effort. It’s the sum of the vital capacity and the residual volume. It’s around 5800 mL.
Lung volumes:
|
Name |
Abbreviation |
Normal value (mL) |
|
Tidal volume |
TV | 500 |
| Inspiratory reserve volume | IRV |
3000 |
|
Expiratory reserve volume |
ERV | 1000 |
| Residual volume | RV |
1200 |
Lung capacities:
|
Name |
Abbreviation | Normal value (mL) | Calculation |
| Inspiratory capacity | IC | 3500 |
TV + IRV |
|
Functional residual capacity |
FRC | 2300 | ERV + RV |
| (Forced) vital capacity | (F)VC | 4600 |
IRV + TV + ERV |
|
Total lung capacity |
TLC | 5800 |
IRV + TV + ERV + RV |
Dynamic lung parameters
The dynamic lung parameters are those which measure the airflow and its velocity during inspiration and expiration. The parameters are:
- Peak expiratory flow (PEF)
- Forced expiratory flow (FEF)
- Forced expiratory flow at 75% lung capacity (FEF75)
- Forced expiratory flow at 50% lung capacity (FEF50)
- Forced expiratory flow at 25% lung capacity (FEF25)
- Forced expiratory volume in one second (FEV1)
- Forced inspiratory volume in one second (FIV1)
- The Tiffeneau index
The peak expiratory flow (PEF) is the maximum possible velocity the patient can exhale air at.
The forced expiratory flow (FEF) is the maximum possible velocity the patient can exhale air at when the lung is at a given capacity. For example, FEF75 measures the velocity of the air flow during exhalation when the lung is only 75% filled with air. FEF50 measures the velocity when the lung is 50% filled, and so on.
The forced expiratory volume in one second (FEV1) measures how much air the patient can exhale during one second, after a full inspiration.
The forced inspiratory volume in one second (FIV1) measures how much air the patient can inhale during one second, after a full expiration.
The Tiffeneau index is not a measured parameter. It’s a percentage which is calculated by dividing FEV1/FVC. It’s normally above 70%. This means that normally, a person should be able to exhale 70% of their whole forced vital capacity within 1 second.
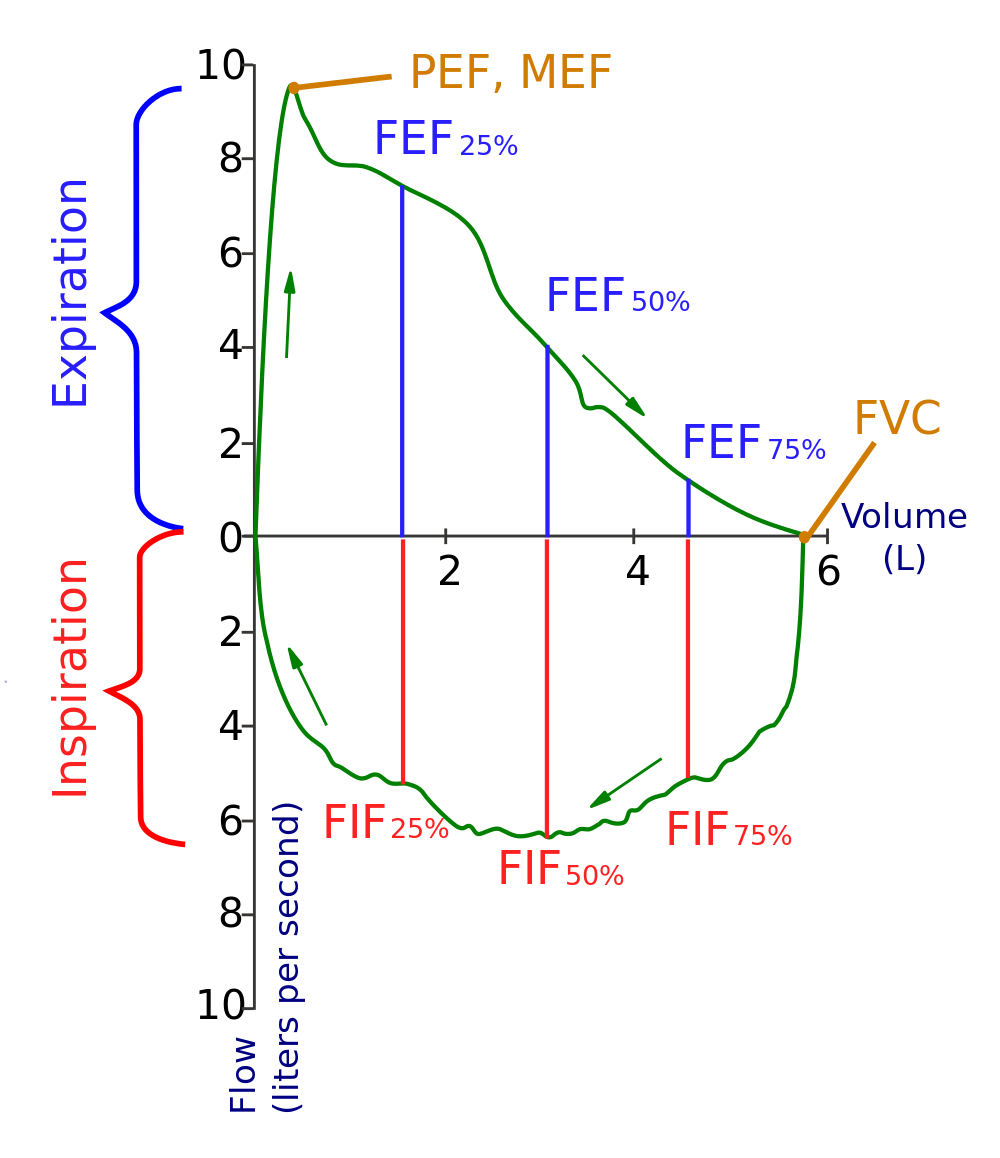
A so-called “flow-volume-loop”. At the start of the spirometry the trace begins at the origin (0,0). As the patient expires the trace moves upward and clockwise. The arrows show the direction of the trace. From Wikipedia.
Respiratory disorders
Many respiratory disorders alter the static and/or dynamic lung parameters and can therefore be diagnosed with spirometry. We distinguish obstructive lung disorders and restrictive lung disorders.
Obstructive lung disorders:
Obstructive lung disorders involve an obstruction of the airways. This causes expiration to become more difficult. The most important obstructive lung disorders are:
- Asthma
- Chronic obstructive pulmonary diseases (COPD), which include:
- Chronic bronchitis
- Emphysema
The parameter which changes the most in all obstructive lung disorders is the FEV1. This causes the Tiffeneau index to decrease, which is characteristic for obstructive lung diseases.
In emphysema some other parameters also change:
- Compliance of the lung increases
- Elasticity of the lung decreases
- The total lung capacity increases
Restrictive lung disorders:
Restrictive lung disorders involve a decrease in expansibility of the lungs, causing the lungs to be more “restricted”. This means that inspiration becomes more difficult. The following parameters change:
- The total lung capacity decreases
- The vital capacity decreases
- The compliance decreases
- The Tiffeneau index is normal or abnormally high