Table of Contents
Page created on November 9, 2019. Last updated on December 18, 2024 at 16:55
The kidneys
Functions:
The kidneys have many functions. Their major function is to filter the plasma for waste products. Here are all of the kidney’s functions:
- Excretory functions
- Excretion of waste products
- Urea
- Creatinine
- Excretion of toxins
- Excretion of certain drugs
- Excretion of waste products
- Regulation of fluid and electrolyte balance
- Regulation of the fluid volume
- Keeping the plasma isotonic
- Maintaining isoosmolarity
- Regulating pH
- Synthesis of hormones
- Erythropoietin
- Activation of vitamin D
- Long-term regulation of blood pressure
- Renin-angiotensin-aldosterone system
The kidneys produce urine, which consists of water, electrolyte and other substances which are filtered from the plasma.
Structure:
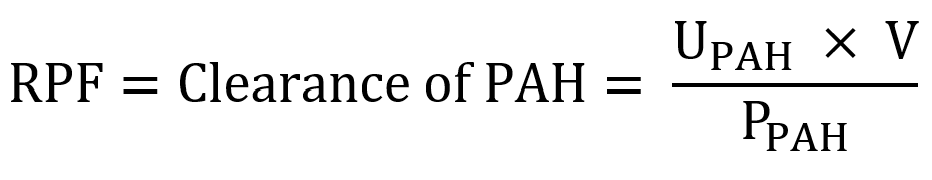
The kidneys are built up of functional units called nephrons. Each kidney has around 1 million nephrons which all work together to produce urine.
Each nephron is comprised of two major parts: A renal corpuscle and a tubule. The renal corpuscle consists of the glomerulus and the Bowman capsule, a capsule around the glomerulus.
The tubule can be divided into four parts:
- The proximal convoluted tubule
- The loop of Henle, which is divided into two parts:
- The descending limb of loop of Henle
- The ascending limb of loop of Henle
- The distal convoluted tubule
Each tubule empties into a collecting duct, which carries urine toward the bladder.
Two nephrons. From Wikipedia.
The renal corpuscle:
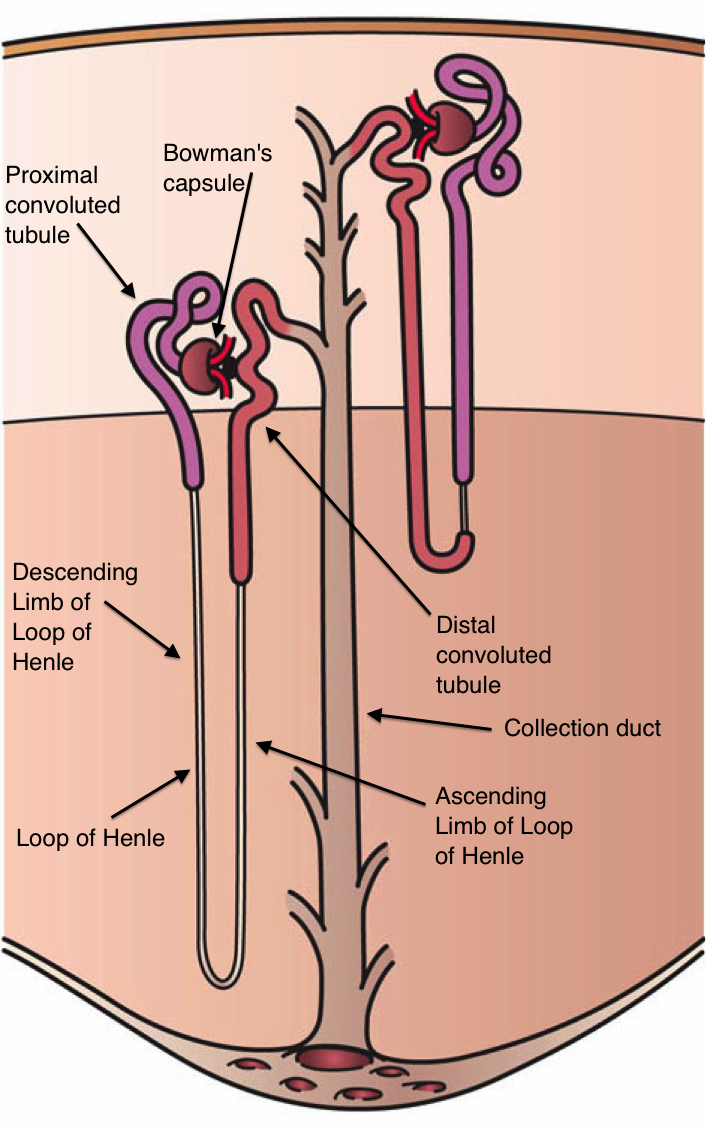
The renal corpuscle is comprised of the glomerulus and the Bowman capsule. The glomerulus is a network of capillaries, often described as a tuft. Blood enters the glomerulus through a so-called afferent arteriole and leaves the glomerulus through an efferent arteriole. The Bowman capsule contains a space called the Bowman space.
When blood is inside the glomerulus the blood is filtered into the Bowman space. The Bowman space opens into the tubular system and therefore carries the so-called ultrafiltrate into the tubule. This process is called glomerular filtration.
The filtered blood leaves the glomerulus through the efferent arteriole. The efferent arteriole will then form a capillary network around the tubules. This capillary network is called the peritubular capillary network. The capillary network empties into the renal vein.
A nephron and the peritubular capillary network. From https://courses.lumenlearning.com/suny-ap2/chapter/gross-anatomy-of-the-kidney/
Glomerular filtration
The capillaries which comprise the glomerulus have special walls. Like all vessels they’re lined by endothelial cells. The endothelial cells are tightly connected with no pores between them. However, they have so-called fenestrae. Fenestrae are pores which go though the endothelial cells. The fenestrae allow fluid and solutes to pass through the capillary wall and into the Bowman’s capsule. The fenestrae are not large enough to allow proteins or cells to pass through, so proteins and cells are never filtered.
More specifically, only molecules smaller than approx. 65 kDa are filtered. The glomerular basement membrane is negatively charged, so negatively charged proteins like albumin are not filtered either, even though they’re smaller than 65 kDa.
When blood passes through the glomerulus around 20% of the plasma is filtered. The filtered fluid is called the glomerular filtrate or ultrafiltrate, and it enters the tubular system of the nephron through the Bowman space. The ultrafiltrate has very similar composition as the plasma, except that it does not contain proteins.
Glomerular filtration rate:
The rate at which blood is filtered through all the glomeruli of the kidney is called the glomerular filtration rate (GFR). The GFR is normally 100 – 125 mL/min, meaning that around 100 millilitres of plasma pass through the glomerular filter every minute.
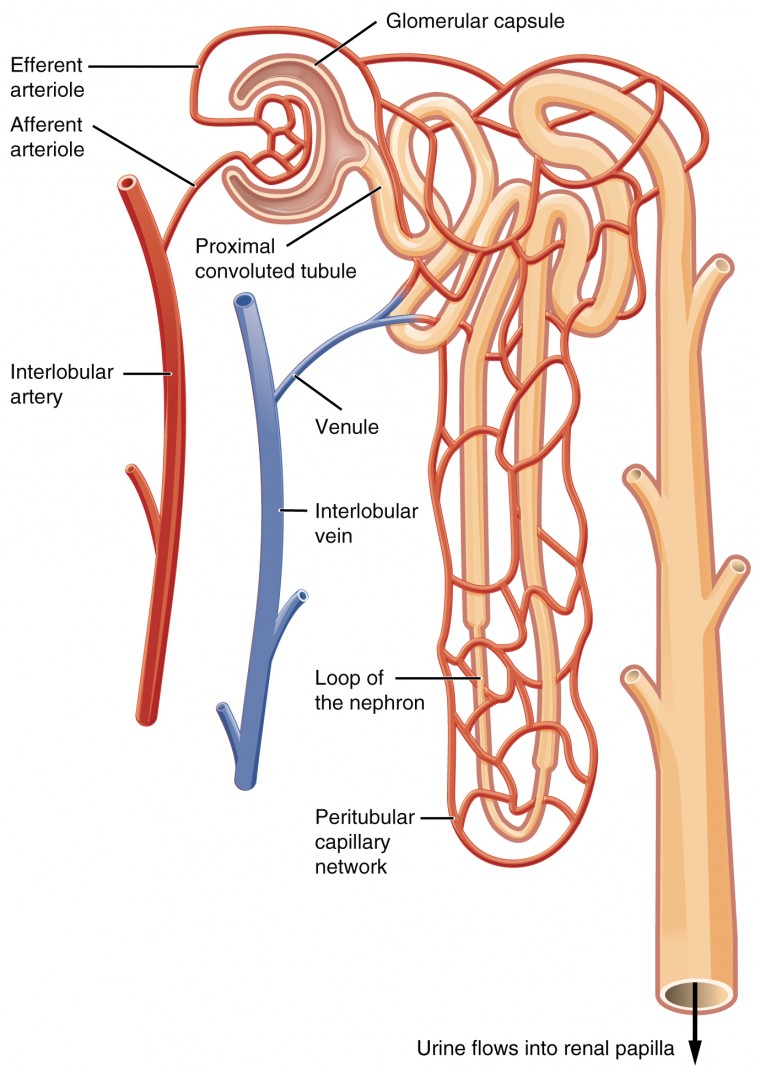
We have previously discussed the Starling forces which influence whether fluid leaves or enters the capillaries. The same forces act on the glomerular capillaries, but the sum of the forces is larger than in normal capillaries. We can calculate the so-called effective filtration pressure (EFP) or ultrafiltration pressure with the Starling equation:
![]()
PGC is the hydrostatic pressure inside the glomerular capillaries. This hydrostatic pressure is normally around 60 mmHg, which is much higher than in normal capillaries (around 17 mmHg). This is because normal capillaries empty into low-pressure veins, while glomerular capillaries empty into an artery, which has much higher pressure than a vein.
The PGC depends on the pressure difference in the afferent and efferent arteriole.
PBS is the hydrostatic pressure inside the Bowman space. It is normally low.
πGC is the oncotic pressure inside the glomerular capillaries. It is mostly the same as the oncotic pressure of other capillaries, as they contain the same blood.
πBS is the oncotic pressure inside the Bowman space. Because proteins are normally not filtered into the bowman space the πBS is normally zero.
Because the hydrostatic pressure inside the glomerular capillaries is so high the ultrafiltration is always positive, meaning that there will always be filtration. The effective filtration pressure is normally around 10 mmHg.
The forces which are responsible for ultrafiltration. From Guyton.
Now that we know the effective filtration pressure, we can use it to calculate the GFR with the following formula:
![]()
Kf is the filtration coefficient. It is a constant value for the glomerular capillaries and is not very important.
Regulation of the GFR:
Now that we know which factors determine the GFR we can look at which factors the body uses to regulate it.
By vasoconstricting or vasodilating the afferent or efferent arteriole we can change the hydrostatic pressure inside the glomerulus. In addition to this some pathological states can change the GFR too.
|
Mechanism |
Example cause | Effect on GFR |
| Constriction of afferent arteriole | Sympathetic activation |
↓ |
|
Constriction of efferent arteriole |
Angiotensin II ↑ | ↑ |
| Dilation of afferent arteriole | Atrial natriuretic peptide (ANP) |
↑ |
|
Dilation of efferent arteriole |
Tubuloglomerular feedback (↑ NaCl in distal tubule) | ↓ |
| Increased plasma protein concentration |
↓ |
|
|
Decreased plasma protein concentration |
↑ | |
| Blockage of the tubular system | Kidney stone |
↓ |
The arterioles are not innervated by the parasympathetic nervous system. The tubuloglomerular feedback system is not important to know about.
Excretion
Excretion is a measurement of how much of a substance is excreted into the urine by the kidneys every minute. It is calculated like this:
E = U x V
E is the excretion, measured in mg/min.
U is the concentration of the substance in the urine.
V is the minute diuresis; how much urine is produced by the kidneys every minute. It’s normally around 1 mL/min.
Clearance
Clearance, or more specifically plasma clearance is a measurement of how much of a specific substance can be removed or cleared from the plasma every minute. It is usually measured in mL/min.
For example, if the clearance of Na+ is 5 mL/min we know that the kidneys clear 5 mL of plasma of Na+ every minute.
Clearance can be calculated by the following formula:
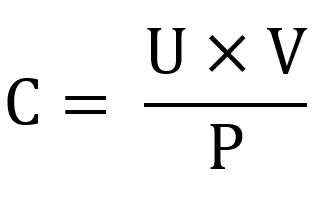
C is the clearance, measured in mL/min.
U is the concentration of the substance in the urine.
V is the minute diuresis; how much urine is produced by the kidneys every minute.
P is the concentration of the substance in the plasma.
Clearance can also be expressed in terms of excretion:
C = E / P
Methods of clearance:
The kidneys can clear substances from the plasma in two ways: It can filter them by glomerular filtration, or it can secrete them by tubular secretion, the details of which we will see in topic 76.
The kidneys can also reabsorb substances it has filtered or secreted. This occurs in the tubular system and will also be described in topic 76.
Different substances are filtered, secreted and reabsorbed to different degrees. For example:
- Glucose is filtered but 100% of it is reabsorbed, so it is not cleared at all
- Amino acids are filtered but 100% of them are reabsorbed, so it is not cleared at all
- Creatinine is filtered but not reabsorbed or secreted
- Inulin is filtered but not reabsorbed or secreted
- Urea is filtered but some of it is reabsorbed. It is not secreted
- Uric acid is filtered and secreted but not reabsorbed
We can use some of these substances to measure the rate of filtration and clearance.
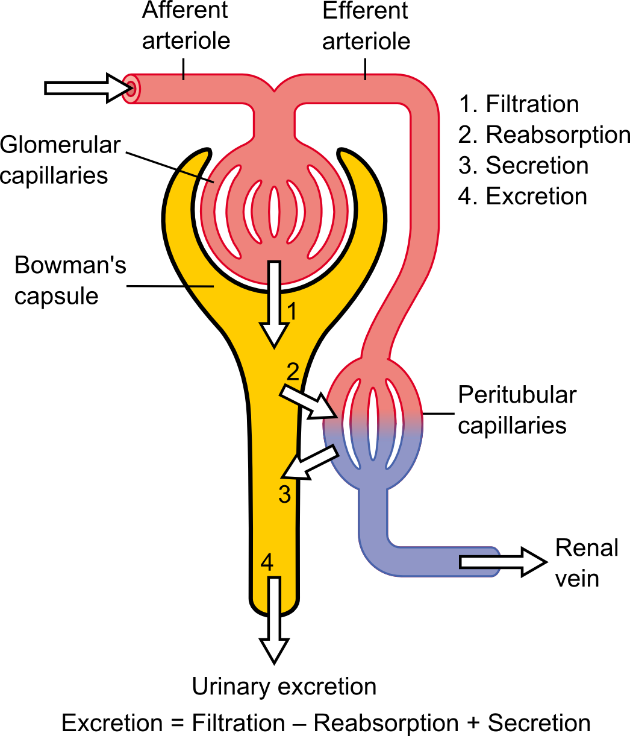
The different fates of substances in the nephron. From Wikipedia.
Relationship between clearance, filtration, reabsorption and secretion
Compounds with clearance = 0:
Some compounds are not cleared from the kidney at all, which means that they cannot be found in urine in normal circumstances. This includes compounds like glucose and amino acids. These are valuable energy sources which the body doesn’t want to lose.
These compounds are filtered by the glomerulus, but they’re quickly reabsorbed by the tubular system before they’re excreted in the urine.
Compounds with clearance = GFR:
Some compounds have clearance equal to the GFR. This is because they are completely filtered and not secreted or reabsorbed. This includes inulin and creatinine.
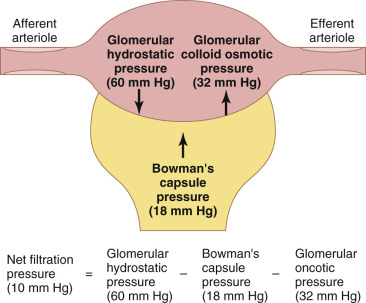
Compounds with clearance = RPF:
One compound has clearance (almost) equal to the renal plasma flow (see next topic). This compound is called PAH. Because PAH is completely filtered and secreted, all plasma which flows through the kidney is almost completely cleared of PAH. This is why the clearance of PAH is almost equal to the RPF.
Measurement of GFR using inulin:
Because inulin is filtered, but not reabsorbed or secreted, the clearance of it can be used to measure the GFR. We administer inulin to a patient. We then measure the plasma concentration of inulin (Pinulin), the minute diuresis (V) and the concentration of inulin in the urine (Uinulin). We can then calculate the clearance of inulin, which is equal to the GFR:
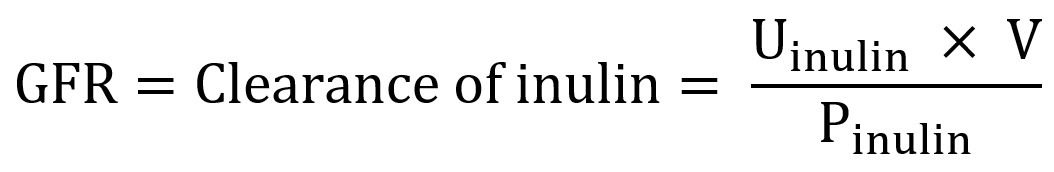
Measurement of RPF using PAH:
Because PAH is filtered and secreted but not reabsorbed its clearance is almost equal to the RPF. By calculating the clearance of PAH, we can estimate the renal plasma flow.