Table of Contents
Page created on October 2, 2021. Last updated on December 18, 2024 at 16:58
Introduction
Immobilising patients during the postoperative period increases the risk for venous thromboembolism (VTE), including DVT and PE. Especially orthopaedic and traumatological surgeries require longer postoperative immobilisation. It’s important to prevent and know how to recognise this.
Recognition
For clinical features of VTE, see topic 33 of internal medicine final.
Risk stratification and prevention for non-orthopaedic surgery
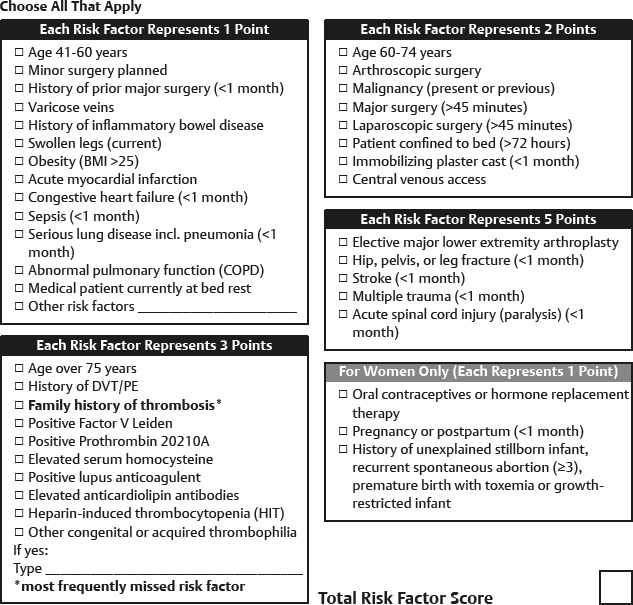
To choose the proper modality of prevention, it’s important to quantify the patient’s risk for VTE. The Caprini score can be used to quantify this risk.
Based on the Caprini score, the suggested interventions are as follows:
| VTE risk | Caprini score | Prophylaxis recommended |
| Very low | 0 | None |
| Low | 1 – 2 | Mechanical prevention |
| Moderate | 3 – 4 | LMWH |
| High | ≥ 5 | LMWH ± mechanical prevention |
The following methods are used in prevention:
- Early and frequent ambulation/physiotherapy
- Mechanical prevention
- Compression stockings
- Intermittent pneumatic compression of the leg
- Pharmacological prophylaxis with LMWH
The preferred anticoagulants for pharmacological prophylaxis are dalteparin (Fragmin) 5000 IE s.c. or enoxaparin (Klexane) 40 mg s.c.
The optimal timing for initiation and termination of anticoagulant prophylaxis should be individualised. Generally, in uncomplicated cases with low bleeding risk they’re initiated 12 hours before surgery and continued until the patient becomes fully ambulatory or is discharged.
In patients at high risk for bleeding, anticoagulants are contraindicated for prevention. Patients at moderate or high risk for DVT/PE with contraindications to anticoagulants should receive non-pharmacological methods of prevention.
Risk stratification and prevention for orthopaedic surgery
To choose the proper modality of prevention, it’s important to quantify the patient’s risk for VTE. The Caprini score is generally not used for orthopaedic surgery, as it was only validated for non-orthopaedic surgery. No scoring system is used to evaluate for VTE risk in orthopaedic surgery; an individual assessment based on the patient’s risk factors is used to estimate the risk. The following are known risk factors for VTE after orthopaedic surgery:
- History of VTE
- Age > 80
- Severe comorbidity (Charlson score > 3)
- High ASA classification
The Charlson comorbidity index scores the patient’s comorbidities based on severity.
The type of surgery is also important. Major surgery (hip or knee replacement or other hip fracture treatment) is considered high-risk for VTE and in these cases pharmacological prophylaxis is usually recommended.
The following methods are used in prevention:
- Early and frequent ambulation/physiotherapy
- Mechanical prevention
- Compression stockings
- Intermittent pneumatic compression of the leg
- Pharmacological prophylaxis with anticoagulants
The preferred anticoagulants for pharmacological prophylaxis are dalteparin (Fragmin) 2500 – 5000 IE s.c. or enoxaparin (Klexane) 40 mg s.c. Apixaban (Eliquis), dabigatran (Pradaxa), and rivaroxaban (Xarelto) are likely equally good alternatives for orthopaedic surgery.
| Type of surgery | Risk for VTE | Prophylaxis recommended |
| Larger hip or knee surgery | Moderate or high risk | Anticoagulant for 10 – 35 days |
| Larger hip or knee surgery | Low risk | Anticoagulant for 10 days |
| Smaller surgeries | Any risk | No anticoagulant |
Treatment
For treatment of VTE, see topic 33 of internal medicine final.
It might also be worth noting that the individual assessment of thrombotic risk in orthopedic surgery is not only based on the patient’s risk factors, but also procedural risk factors (e.g. the greater the extent and duration, the higher the risk, and immobilization and casting increase the risk). It might also be worth mentioning that in general, all patients undergoing major orthopedic surgery are designated as “High thrombotic risk”.
Kind regards
That was already partially covered by the table, but I’ve added a paragraph about it too now. Thanks.