Table of Contents
Page created on December 6, 2018. Last updated on December 18, 2024 at 16:56
Introduction to obstructive lung diseases
Obstructive lung diseases are usually caused by increased airflow resistance, usually due to an obstruction at some point. Four types are important:
- Chronic obstructive pulmonary disease (COPD)
- Chronic bronchitis
- Emphysema
- Bronchiectasis
- Asthma
Emphysema and chronic bronchitis usually occur together, so they’re together called chronic obstructive pulmonary diseases, or COPD. They occur together because the etiology for both is the same: smoking.
The airway obstruction means that these patients struggle to breathe air out. Their FEV1 / FVC ratio (the Tiffeneau index), which measures how much of their total lung volume they can breathe out in one second, is significantly decreased. The normal is >0,7.
We must recall the structure of acini in the lung. These structures are comprised of a respiratory bronchiole, alveolar duct and the alveoli themselves. You can see the structure on the figure below.
Chronic obstructive pulmonary disease
Introduction and epidemiology
Chronic obstructive pulmonary disease (COPD) is characterised by persistent respiratory symptoms and airflow limitation due to airway and/or alveolar abnormalities. It’s common, preventable, and treatable. It is defined as a post-bronchodilator FEV1/FVC ratio of < 0,70.
It affects 11,7% of the world and it’s the third leading cause of death worldwide. Prevalence is expected to rise, and it’s expected to be the leading cause of death in 15 years.
COPD has two phenotypes, chronic bronchitis and emphysema.
Etiology
- Smoking (most important factor)
- Air pollution
- Occupational dusts and chemicals
- Frequent lower respiratory tract infections during childhood
- Alpha-1-antitrypsin deficiency
Pathology
Chronic bronchitis is defined as the presence of a persistent productive (“wet”) cough for at least 3 consecutive months in at least 2 consecutive years. The major pathological changes of chronic bronchitis are mucous gland hypertrophy and hyperplasia and hypersecretion of mucus, which obstructs the airways. The mucosa is often oedematous and covered by mucinous and possibly purulent secretion.
The ratio of mucous glands to the whole thickness of the wall in the bronchi is called the Reid index. It’s usually 0.4 (meaning that 40% of the whole thickness of the bronchial wall is made up of mucous glands), but in chronic bronchitis the glands are hyperplastic and hypertrophic, so this number is increased.
Emphysema is characterised by abnormal permanent enlargement of alveolar spaces because alveolar septa are destroyed. This causes the lung to become abnormally inflated. Two major forms of emphysema are important:
- Centroacinar emphysema affects the respiratory bronchioles but not the alveoli themselves. This type is associated with smoking. It’s more common in the upper lobes of the lung. Smoking causes neutrophils to produce enzymes that degrade the alveolar wall, like elastase.
- Panacinar emphysema affects the alveolar duct and alveoli. This type is associated with a genetic α1-antitrypsin deficiency, and not smoking. α1-antitrypsin is a protein that usually inhibits the effects of proteases like elastase. When this inhibitor is deficient will elastase produced by neutrophils act unopposed to destroy the connective tissue of the lung. It’s more common in the lower lobes of the lung.
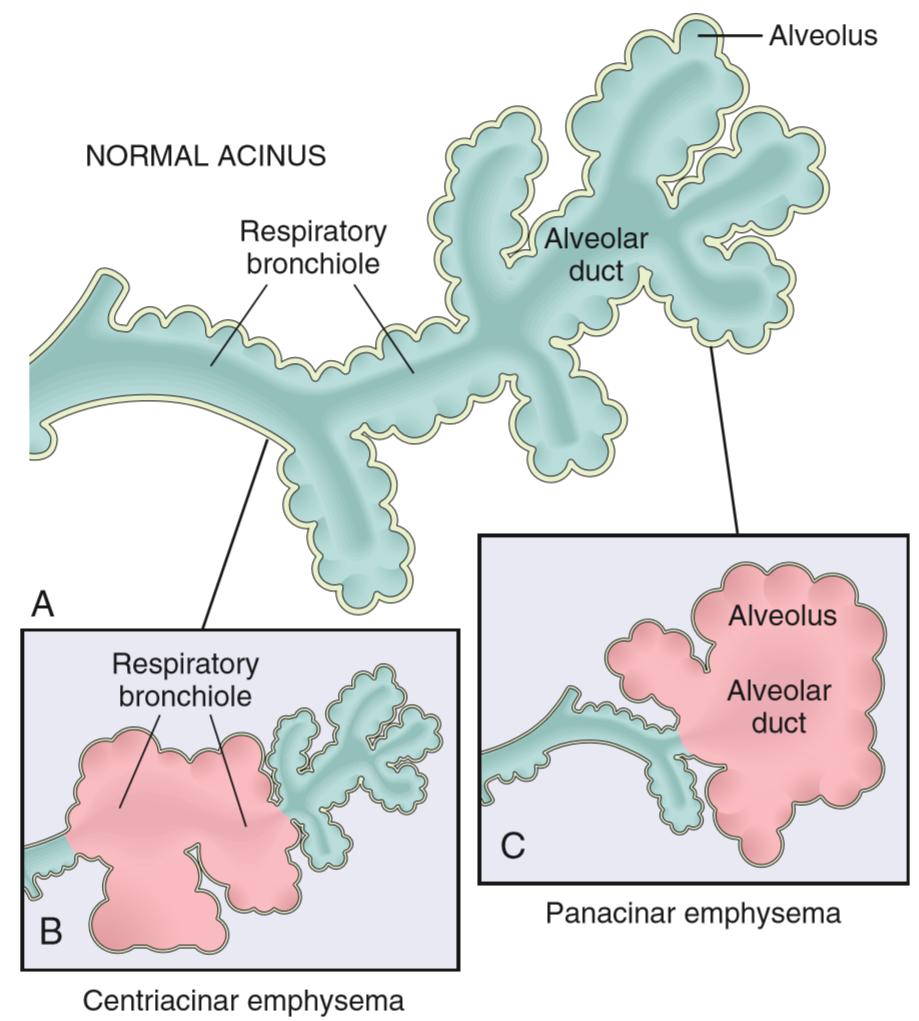
Structure of acini and the two most important types of emphysema. Remember that the centriacinar type is associated with cigarettes.
The obstruction in emphysema occurs when the walls of terminal bronchioles also lose elastic tissue which causes them to collapse during expiration. This “traps” air in the alveoli, which causes the lungs to become hyperinflated.
Clinical features
People suffering from chronic bronchitis can have episodes of acute worsenings of the symptoms, called acute exacerbations. These episodes can be caused by bacterial infection, like by haemophilus, or by viruses, allergens or smoke.
The most important symptom of chronic bronchitis is productive cough, initially without outflow obstruction. Only some patients develop severe enough obstruction that it starts to produce symptoms like respiratory failure. These patients are often obese and cyanotic, which has given them the nickname blue bloaters.
The most important symptom of emphysema is dyspnoea. The hyperinflation causes the lung to expand, and the chest with it. The antero-posterior diameter of the chest increases, which gives the morphology called barrel chest. The destruction of the alveolar wall also decreases the total alveolar surface available for gas exchange, which decreases the diffusion capacity. Patients with emphysema are often hunched over, as they try to use accessory breathing muscles to help force the air out. Skinny, barrel-chested, hunched-over, dyspnoeic people are classic emphysema patients, often called pink puffers. Coughing is not a characteristic symptom. Hypoxia-induced pulmonary vasoconstriction causes pulmonary hypertension with eventual cor pulmonale.
Bronchial asthma
Introduction and epidemiology
Asthma is a chronic inflammatory disorder of the airways characterised by airway hyperresponsiveness which causes recurrent asthmatic attacks. These are episodes of bronchoconstriction, leading to wheezing, dyspnoea, and coughing, sometimes after being exposed to a certain trigger.
It’s one of the most common chronic diseases worldwide. It affects around 300 million people, affect Western countries more than non-Western ones. Prevalence is increasing. In the UK every 5th person has asthma.
Uncontrolled asthma can be fatal, but the mortality rate of asthma is highest in non-Western countries. Asthma diagnosis is not easy, especially in children, and it is frequently overdiagnosed.
Classification
We can subdivide asthma into allergen-induced asthma, non-allergen-induced asthma, and intrinsic asthma. There can be overlap between these types.
Allergen-induced asthma (atopic asthma) is more related to allergens, and usually has onset in childhood. It’s usually a part of the atopic march, which includes the development of atopic dermatitis first, then hay fever, and lastly allergic asthma. These patients usually have TH2-dependent and eosinophil inflammation.
Non-allergen-induced asthma is more related to airway irritants, drugs, and infections, and usually has onset in adulthood. These patients usually do not have TH2-dependent inflammation or eosinophil inflammation, but rather neutrophil inflammation.
In intrinsic asthma, there is airway hyperreactivity without inflammation or allergy.
Aspirin-exacerbated respiratory disease (aspirin asthma) is a special type of asthma which occurs in people taking aspirin or NSAIDs.
Pathology
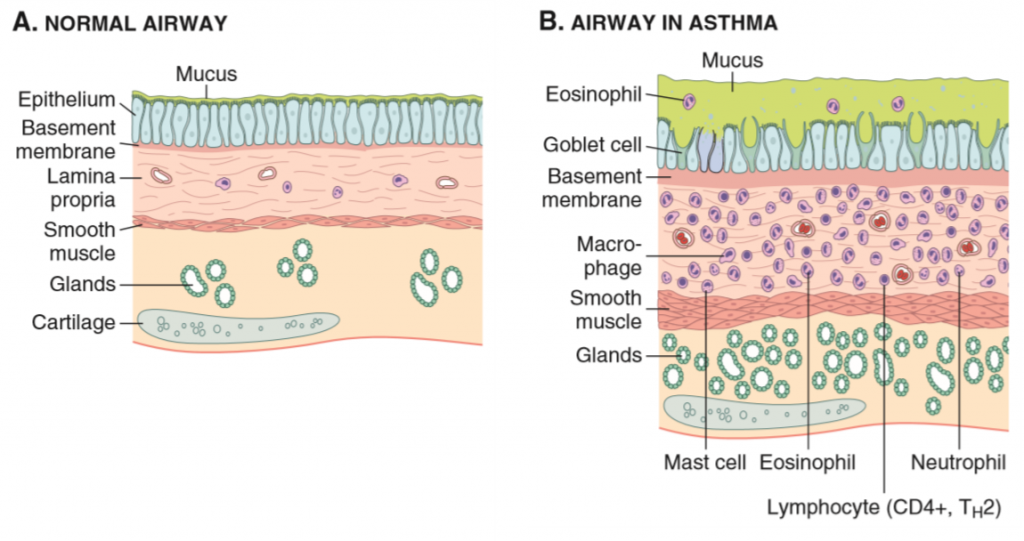
Asthma is characterised by intermittent and reversible airway obstruction, eosinophilic inflammation of the bronchi, bronchial smooth muscle hypertrophy and hyperreactivity, and increased mucus secretion.
Allergen-induced asthma (atopic asthma) is associated with allergy and eczema and is often hereditary. It involves a hypersensitivity type I reaction, which has two phases: the early phase and the late phase. In the early phase there will be bronchoconstriction and increased mucus production, while the late phase is characterised by inflammation. When these reactions occur repeatedly, this will lead to structural changes in the bronchial wall, called airway remodelling, which is when smooth muscle and mucus gland hypertrophy occurs.
Non-allergen-induced asthma (intrinsic asthma) has no association with allergy, and the pathomechanism is unknown. Viral infection may trigger it.
Clinical features
Asthma is characterised by asthmatic attacks, episodes of bronchoconstriction, leading to symptoms like wheezing, dyspnoea, chest tightness, and coughing. These episodes typically occur at night or in the morning.
Bronchiectasis
Introduction and epidemiology
Bronchiectasis means permanent dilation of the bronchi that’s caused by destruction of the smooth muscle and supporting elastic tissue. It’s a secondary condition that usually occurs due to chronic necrotizing infections, often due to:
- Bronchial obstruction
- Tumors
- Foreign bodies
- Thick mucus (cystic fibrosis)
- Necrotizing bacterial infections
- Immunodeficient people
- Staphylococcus aureus pneumonia
- Klebsiella pneumonia
Pathology
Obstruction interferes with the airways’ clearing mechanisms. This makes the airways a much better place for infections, causing chronic necrotizing infections. Proteolytic enzymes and reactive oxygen species produced by leukocytes then damage the walls.
The most distal airways are most severely dilated, up to 4x their normal diameter. A common finding during autopsy is that the airways can be opened all the way to the periphery of the lung, because the distal airways are so dilated. In healthy lungs are the distal airways so small that they can’t be opened during autopsy.
Clinical features
The most common clinical symptom is severe, persistent productive cough with purulent sputum, possibly haemoptysis. Abscesses and empyema of the airways can occur.
α1-antitrypsin is a protease inhibitor, not elastase
Elastase is a protease, and in the pathomechanism of alpha-1-antitrypsin deficiency, neutrophil elastase is the most important protease to be inhibited. I’ve changed the wording slightly to reflect this.
On the exam the paraseptal emphysema and the interstitial emphysema was also asked 🙂