Table of Contents
Page created on April 9, 2019. Last updated on December 18, 2024 at 16:57
Cerebral oedema
Cerebral oedema is the accumulation of excess fluid within the brain parenchyme. There are three different types:
- Vasogenic oedema
- Cytotoxic oedema
- Interstitial oedema
Vasogenic oedema occurs when the blood-brain barrier is damaged, which allows fluid to shift from the intravascular compartment into the extracellular compartment of the brain. It can be localized or generalized. It occurs due to inflammation, ischaemia or tumors. This oedema contains proteins.
Cytotoxic oedema occurs when there is an increase in intracellular fluid of the cells in the CNS. This occurs secondary to a metabolic disorder that causes the Na+/K+ ATPase to dysfunction. It occurs in response to ischaemia or certain toxins, like uraemia.
Interstitial oedema occurs when the CSF-brain barrier is disrupted, which allows CSF to enter the brain interstitium. This type of oedema differs from vasogenic oedema as it contains almost no proteins.
Oedematous brains are softer than normal. If the oedema is generalized the gyri are flattened, the sulci are narrowed and the ventricular cavities are compressed.
Increased intracranial pressure
Because the brain lives in a closed space inside the skull will any severe enough oedema cause the intracranial pressure (ICP) to rise. Increased ICP may occur due to:
- A mass in the brain (mass effect)
- Tumor
- Oedema
- Haematoma
- Abscess
- Generalized oedema
- Trauma
- Ischaemia
- Hyperammonaemia
- Uraemia
- Hypotonicity
- Decreased reabsorption of CSF
- Obstructive hydrocephalus
- Meningitis
- Increase in intracerebral blood volume
- Hypercapnia
- Venous sinus thrombosis
- Venous congestion – like in heart failure
Increased intracranial pressure has multiple consequences:
- Headache
- Papilloedema – swelling of the optic disc, which can be seen on ophthalmoscopy
- Altered consciousness
- Decerebration – quadriplegia with all extremities extended
- Cerebral herniation
Cerebral herniation
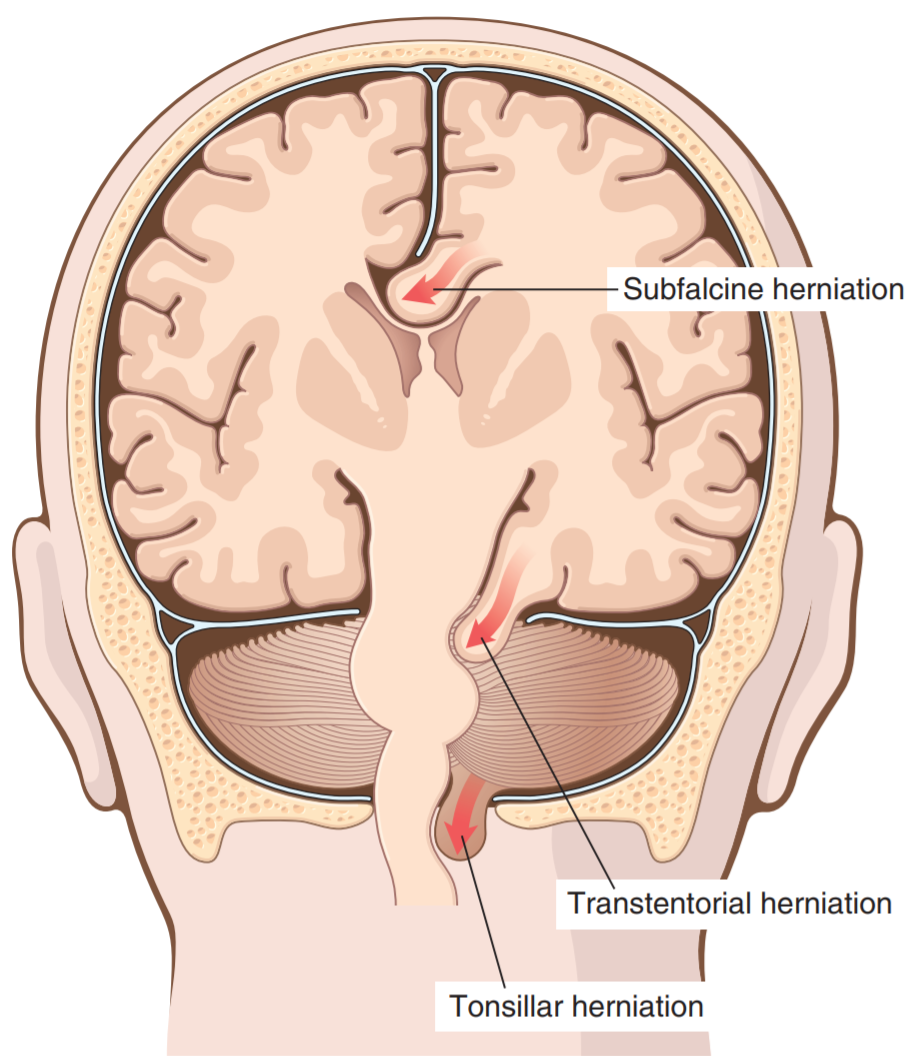
The cranial vault is subdivided by rigid folds of the dura mater, the tentorium cerebelli and the falx cerebri. If the brain parenchyme expands, as it does in oedema, the parenchyme may herniate across these rigid folds. The herniated parenchyme is often “pinched”, which promotes infarction and swelling of the affected parenchyme.
There are three types:
- Subfalcine (= cingulate) herniation
- Transtentorial (= uncinate) herniation
- Foraminal (= tonsillar) herniation
Subfalcine herniation, also called cingulate herniation occurs when unilateral or asymmetric expansion of a cerebral hemisphere herniates the cingulate gyrus medially, under the edge of the falx cerebri. This may compress the anterior cerebral artery.
Transtentorial herniation, also called uncinate herniation occurs when the medial aspect of the temporal lobe is compressed against the free margin of the tentorium cerebelli, which allows it to herniate inferiorly along the brain stem. This herniation may compress the oculomotor nerve, causing ptosis (drooping of the eyelid), mydriasis (dilated pupils) and ophthalmoplegia (weakness of one or more extraocular muscles).
This type of herniation may rupture arteries or veins in the pons, which causes a characteristic Duret bleeding. Intracranial haemorrhages are further described in topic 39.
Foraminal herniation, also called tonsillar herniation occurs when the cerebellar tonsils herniate through the foramen magnum. This is the most serious cerebral herniation as it may compress vital respiratory and cardiac centres in the medulla oblongata.
Hydrocephalus
CSF is produced by choroid plexus, after which it flows through the ventricles just to reach the subarachnoid space through the foramina of Luschka and Magendie where it will be absorbed by arachnoid granulations. The rate of production and absorption is usually balanced, so that the CSF volume isn’t excessive.
Hydrocephalus refers to increased amount of CSF in the ventricular system. It most commonly occurs due to impaired flow or absorption. There are three major types, the communicating type, the non-communicating type and hydrocephalus ex vacuo.
Non-communicating hydrocephalus occurs when there is an obstruction of CSF flow within the ventricles, most commonly at the site of the foramina of Monro (between the lateral and third ventricles) or at the site of the cerebral aqueduct (between the third and fourth ventricles). This causes parts of the ventricular system to dilate.
Communicating hydrocephalus occurs when there is an obstruction of CSF flow outside the ventricles, or when there is a reduction in CSF absorption. It often occurs due to:
- Obstruction
- Tumor
- Congenital malformations
- Reduced CSF absorption
- Chronic meningitis
- Subarachnoid haemorrhage
Normal pressure hydrocephalus is a form of communicating hydrocephalus where there is a classic triad of symptoms, including dementia, gait disturbance and incontinence.
Hydrocephalus ex vacuo refers to a compensatory increase in CSF volume due to atrophy of the brain parenchyme. It usually occurs after degenerative diseases or infarcts.
Malformations of the CNS
CNS malformations occur in around 1 – 2% of the population, and they’re more common in people who have multiple birth defects.
The developmental malformations may be divided into four subtypes:
- Neural tube defects/spinal dysraphisms
- Anencephaly
- Spina bifida
- Spina bifida occulta
- Meningocele
- Meningomyelocele
- Forebrain anomalies
- Holoprosencephaly
- Microcephaly
- Megalencephaly
- Lissencephaly
- Polymicrogyria
- Corpus callosum agenesis
- Cortical malformation
- Posterior fossa anomalies
- Dandy-Walker malformation
- Arnold-Chiari malformation
- Spinal cord anomalies
- Hydromyelia
- Syringomyelia
Neural tube defects
The formation of the neural tube, which gives rise to the ventricular system, brain and spinal cord, occurs early in the embryogenesis. Neural tube defects, also called spinal dysraphisms, occur when the neural tube isn’t closed properly.
The most important cause of neural tube defects is folate deficiency, but there is a genetic background as well. Hyperthermia is another important cause. Folate supplementation during pregnancy is important to prevent this developmental malformation.
The most important neural tube defects are:
- Anencephaly – absence of the brain and top of skull
- Spina bifida
- Spina bifida occulta – asymptomatic bony defects
- Meningocele – Defect in the vertebral column containing dura and arachnoid maters
- Myelomeningocele – Defects in the vertebral column containing dura and arachnoid maters and spinal cord
Spina bifida is the most common congenital CNS malformation. Common symptoms of it includes back pain, incontinence, paraplegia and meningitis.
Most babies born with anencephaly live only a few hours or days, but a baby survived for three years with the condition.
Forebrain anomalies
Anomalies of the forebrain or prosencephalon develop due to abnormal proliferation and migration of subependymal progenitor cells. This most frequently causes fewer mature neurons to develop, causing microencephaly, but it may cause megalencephaly as well.
These anomalies are associated with:
- Chromosome abnormalities
- Foetal alcohol syndrome
- HIV infection
- Diabetes mellitus in the mother
The most important forebrain anomalies are:
- Holoprosencephaly
- Lissencephaly/pachygyria – decreased/absence of gyration, smooth-surfaced brain
- Microencephaly – smaller than average brain
- Megalencephaly – larger than average brain
- Polymicrogyria – increased, abnormal gyri. Cobblestone-like surface
- Corpus callosum agenesis
- Cortical malformation – often associated with epilepsy
Holoprosencephaly involves abnormal fission and rotation of the forebrain, which disrupts the normal midline-pattern of the brain. In mild forms may only the olfactory bulbs and related structures be absent, but in severe forms the brain may not be divided into hemispheres and lobes. It’s associated with facial midline defects like cyclopia.
Posterior fossa anomalies
These anomalies involve misplacement or absence of portions of the cerebellum. The most important ones are the Arnold-Chiari and Dandy-Walker malformations.
Arnold-Chiari malformations exists in four types, where type I is the mildest. It may involve:
- Tonsillar herniation
- Lumbar myelomeningocele
- Cerebellar hypoplasia
- Syringomyelia
Dandy-Walker malformation involves:
- An enlarged posterior fossa
- Hypoplastic vermis
- Cystic 4th ventricle
- Non-communicating hydrocephalus
Spinal cord anomalies
Spinal cord anomalies involve abnormalities of the spinal cord that don’t affect the spinal column or overlying skin. The most important ones are:
- Hydromyelia – dilated central canal
- Syringomyelia – fluid-filled cyst in spinal cord
Hello Nikolas!
Hope that u r doing well!
In Duret bleeding arteries and veins as well may rupture- Robin’s p814
Added! Thank you.
Stay safe!