Page created on May 3, 2019. Last updated on December 18, 2024 at 16:57
Introduction
Before we begin, we need to know some macroscopic skin lesions.
Excoriation is a traumatic skin lesion often caused by scratching its own skin. A red linear mark forms as the epidermis is broken.
Lichenification is a thickened and rough skin characterised by prominent skin markings. It’s characteristic for lichen simplex chronicus. It can occur in response to of repeated rubbing or itching of the skin.

Lichenification. From https://www.healthline.com/health/lichenification
A macule is a flat, circumscribed lesion less than 5 mm in diameter that is only distinguished from the surrounding skin by its colour. If it is more than 5 mm in diameter it’s called a patch.
Macule. From https://medical-dictionary.thefreedictionary.com/macule
A papule is a circumscribed, solid elevation of the skin less than 5 mm in diameter. If it is greater than 5 mm it’s called a nodule.

Papule. From https://en.wikipedia.org/wiki/Papule
A plaque is a flat-topped elevation of the skin, usually greater than 5 mm in diameter.

Plaques of psoriasis. From https://fineartamerica.com/featured/5-plaque-psoriasis-on-the-skin-dr-p-marazziscience-photo-library.html
A pustule is a discrete, pus-filled raised lesion.

A pustule. From https://www.shutterstock.com/image-photo/purulent-pustule-on-skin-1126098869?src=okW2hsBN1AkZoZtsYKTGPQ-1-2
A scale is a dry, horny, plate-like morphology of the skin.

Scaly skin. From https://healthh.com/scaly-skin/
A vesicle is a fluid-filled raised area 5 mm in diameter or less. If greater than 5 mm it’s a blister.

Vesicles. From https://ufhealth.org/vesicles
We also need to know some histological terms:
Acantholysis refers to loss of intercellular adhesion of keratinocytes.
Acanthosis refers to diffuse epidermal hyperplasia.
Dyskeratosis refers to abnormal keratinization of cells below the stratum granulosum.
Hyperkeratosis refers to hyperplasia of the stratum corneum.
Lentiginous refers to proliferation of melanocytes in the epidermal basal cell layer.
Papillomatosis refers to elevated skin due to hyperplasia and enlargement of dermal papillae.
Parakeratosis refers to keratinization while the cells of the stratum corneum retain their nuclei. (the cells of the stratum corneum normally lose their nuclei)
Spongiosis refers to intercellular oedema of the epidermis.
Benign melanocytic lesions
Melanocytes are the cells that are responsible for skin pigmentation. These cells reside among keratinocytes in the basal layer of the epidermis and produce melanin in so-called melanosomes, which the keratinocytes then take up.
Ephelis is a common type of freckle. It appears in sun-exposed skin and is usually more prominent during the summer than in the winter. It occurs due to melanocytes producing more melanin than normal, without any hyperplasia.
Lentigo is a hyperpigmented macule. It also appears in sun-exposed skin. It is due to a benign hyperplasia of melanocytes.
Cafe au lait spots are also hyperpigmented macules. Unlike lentigo they are not associated with sun exposure and is instead present at birth. If a person has many (> 6) Cafe au lait spots they probably have neurofibromatosis type 1. People suffering from NF1 have increased risk for MPNST, a highly malignant soft tissue tumor of the nerve sheath.
Melanocytic nevi (singular: nevus) is a benign neoplasm of melanocytes. They’re often small, brown papules with well-defined, rounded borders, but they can be flat as well. Hair may grow out of the nevus. Melanocytic nevi can be congenital or acquired. The cells of melanocytic nevi are called nevus cells and are morphologically different from melanocytes, although they originate from them. These neoplasms have three different stages:
- Junctional nevus – nevus cells form nests at dermo-epidermal junction, on the epidermal side
- Compound nevus – nevus cells form nests in the dermis as well
- Intradermal nevus – nevus cells form nests only in the dermis (no cells in the epidermis)
Spitz nevi have atypical nevus cells that can mimic melanoma.
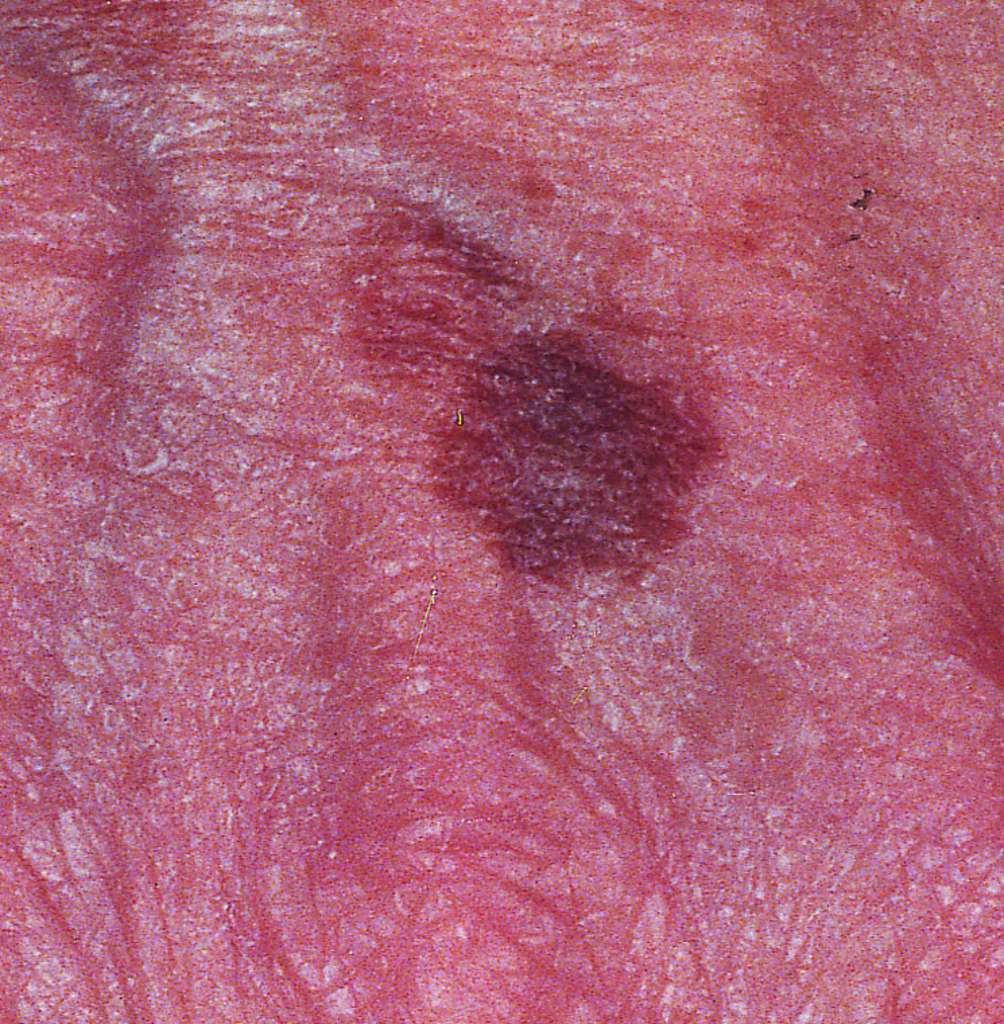
Dysplastic nevi (or Clark nevi) are similar to melanocytic nevi, but they are larger, have a rougher surface and have irregular borders. These neoplastic cells show atypia. The presence of dysplastic nevi are associated with an increased risk for melanoma, but they’re not precancerous lesions for melanoma. Melanoma very rarely develops from dysplastic nevi.
The presence of many dysplastic nevi in a patient with a positive family history for melanoma is called dysplastic nevus syndrome is associated with an almost 100% lifetime risk of developing melanoma.
Melanoma
Melanoma is a highly malignant tumor arising from melanocytes. It is the most common cause of death from dermatological diseases. It’s caused by UV radiation-mediated DNA damage, so the risk factors are excessive sunlight exposure and conditions that predispose to increased sunlight exposure or decreased defence against this type of DNA damage.
Risk factors:
- Excessive exposure to UV radiation (much sun, little sunscreen)
- Light skin
- Dysplastic nevus syndrome
- Albinism
- Xeroderma pigmentosum
People with albinism produce no melanin and the melanocytes are therefore more exposed to UV radiation. People with xeroderma pigmentosum lack the enzymes that repair UV-mediated DNA damage and therefore have increased risk for melanoma.
Very few dysplastic nevi transform into melanoma; most cases of melanoma arise de novo. Because of this, sporadic dysplastic nevi don’t increase the risk significantly for developing melanoma. Dysplastic nevus syndrome however has an almost 100% risk of developing into melanoma.
Pathogenesis: Melanoma is characterised by two different growth phases; the radial growth phase and the vertical growth phase.
During the radial/horizontal growth phase, the tumor grows horizontally along the epidermis, corresponding to an in situ lesion. During this phase the tumor cells don’t have the capacity to metastasize.
During the vertical growth phase, the tumor grows vertically into the dermis. It is during this phase that the tumor cells acquire the ability to metastasize. It is the extent of the vertical growth phase that determines the biological behaviour and prognosis.
Subtypes: Multiple subtypes of melanoma exist:
Superficial spreading melanoma is the most common subtype. It’s characterised by a long radial growth phase and mostly superficial spreading.
Nodular melanoma is the second most common type. It’s characterised by the formation of a nodule. Its vertical growth phase occurs early, which is why it has a poorer prognosis than the other types.
Lentigo maligna melanoma is the third most common type. Its radial growth phase is long and slow.
Acral lentiginous melanoma is the least common type. Its radial growth phase is slow. It occurs on the palms or soles of dark-skinned individuals. Unlike the other subtypes this type is not related to UV exposure.
Diagnosis: The ABCDE criteria are useful for distinguishing between benign skin lesions and melanoma:
- A – asymmetric shape
- B – border is irregular
- C – colour is irregular
- D – diameter enlarged (> 5 mm)
- E – Evolution (as in, the lesion changes over time)
The ugly duckling sign is also useful. The sign is positive if a person has a lesion that is different from other nevi on the same patient. Benign nevi usually look similar on the same person.
Melanomas can also bleed and itch, which benign melanocytic lesions don’t do. Hair never grows out of melanomas.
Two staging systems are important in melanoma. The most important is the Breslow depth, which measures the length in millimetres from the stratum granulosum to the deepest part of the tumor. The prognosis worsens considerably with increase in depth; tumors of just a few mm (2 – 4) have significantly poorer prognosis than those that are 1 – 2 mm.
The other staging system is the Clark level, which ranges from I to V. At level I the tumor is in situ, and at level V the tumor has invaded the subcutaneous tissue. The Breslow depth has proven to be of higher prognostic value than the Clark level.
Prognosis: The survival rate drops in cases where metastases are present at the time of diagnosis. Melanoma frequently metastasizes into the liver, lung, brain and bone. Rarely, melanoma can metastasize into unusual locations like the heart and gallbladder. These metastases have characteristic black pigmentation.
The prognosis is poorer in tumors that have penetrated the dermis.
Hello,
Would you please elaborate on this sentence?
“Tumors of just a few mm (2-4) have significantly poorer prognosis than those that are 1-2 mm”
Done.
Hi! I think Clark nevi and dysplastic nevi are the same? At least the lecture said it is
I think you’re right. Changed now.
¡Hola, Nik!
Just wanted to tell you that under our seminar, our teacher said that neither Breslow or Clark is preferred over the other. They are usually used together and “fill each other out”.
Clark is considered less predictive and of less value nowadays:
https://www.verywellhealth.com/clark-level-and-breslow-thickness-for-melanoma-staging-3010751
https://www.ncbi.nlm.nih.gov/pubmed/11504744
https://www.curemelanoma.org/about-melanoma/melanoma-staging/breslow-depth-and-clark-level/
https://emedicine.medscape.com/article/1295718-overview#a6
Szia Nick❤️
Acantholysis is loss of intErcelluar adhesions
True
Fixed.
the lecture is out now 😉
Nope. The lecture they published is called “dermatopathology” but actually only includes the inflammatory skin diseases, and not the epithelial or melanocytic ones.