Page created on May 12, 2019. Last updated on December 18, 2024 at 16:57
Page created on May 12, 2019. Last updated on December 18, 2024 at 16:57
Congenital anomalies of the lung
A bronchogenic cyst is an abnormal budding of the lung primordium. It’s commonly localized in the anterior mediastinum, and often contains respiratory epithelium and cartilage.
Congenital lobar emphysema is a congenital anomaly characterized by hyperinflation of one or multiple lobes. It’s similar to panacinar emphysema. Surgical removal of the affected region cures the condition.
Pulmonary sequestration is a condition where a piece of lung is not connected to the airways. Two types exist, and both are associated with mucus accumulation and pneumonia:
- The extralobar type has its own pleural surface and blood supply. It’s basically an accessory lung.
- The intralobar type occurs inside another, healthy lobe.
Congenital pulmonary airway malformation occurs when the lung parenchyme of an entire lobe is replaced with abnormal lung tissue. They may transform into carcinoma.
Pulmonary hypoplasia means that the number and size of the alveoli is decreased compared to normal. It often occurs with other abnormalities, such as diaphragmatic, renal or musculoskeletal defects. There are multiple reasons it can occur:
- Diaphragmatic defects allow abdominal contents to herniate into the thorax, compressing the lungs and disallowing them to grow
- Lack of respiratory movements due to neuromuscular diseases
- Loss of lung liquid (oligohydramnios)
Pulmonary agenesis or aplasia is when one lobe, one lung or both lungs are absent. In unilateral agenesis is the healthy lobe enlarged.
Atelectasis
Atelectasis is a term used to describe inadequate expansion of air spaces in the lung. Three types exist:
- Resorption atelectasis occurs when there is an obstruction in the airways which prevents air from reaching the distal airways. The oxygen already inside the alveoli will be absorbed, causing the alveoli to collapse. If the obstruction is large and proximal enough can the collapse affect a complete lobe or even an entire lung.
- Compression atelectasis occurs when fluid or air inside the pleural cavity compresses the lung.
- Contraction atelectasis occur when fibrotic tissue in the lung or pleura hampers the expansion and decreases the compliance of the lung.
Resorption atelactasis is the most common type. It’s caused by a foreign body or a mucus plug. Atelectatic lungs are small, firm and wrinkly.
Acute lung injury
Acute lung injury is a spectrum of bilateral lung damage, which can occur in many conditions, like:
- Pneumonia (especially in immunosuppressed people)
- Aspiration of gastric contents
- Sepsis
- Circulatory shock
Symptoms include dyspnoea, hypoxaemia and bilateral pulmonary oedema (without a left-sided heart failure). Any acute lung injury can progress into acute respiratory distress syndrome (ARDS). In ARDS is there diffuse alveolar capillary and epithelial damage. Life-threatening respiratory failure occurs, with resulting cyanosis and hypoxaemia.
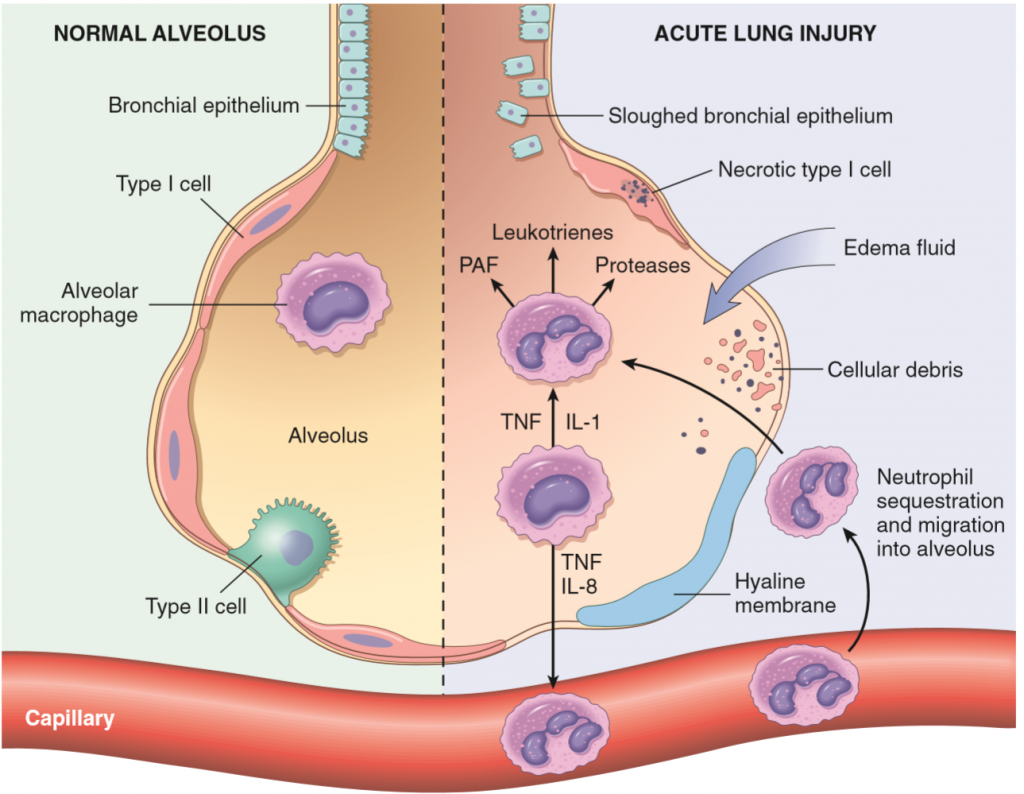
The histological manifestation of ARDS is called diffuse alveolar damage (DAD). It begins when the alveolar-capillary membrane is damaged, which increases vascular permeability and allows exudate to enter the alveoli and prevents gas exchange. Alveolar macrophages respond by recruiting neutrophils, which causes further damage to the endothelium and alveolar epithelium.
The repair process takes place in three phases:
- In the exudative phase fibrin-rich exudate and remnants of necrotic epithelial cells organize and form hyaline membranes. The hyaline membranes cover the gas exchange membrane and blocks it.
- In the regenerative phase, which occurs 1-2 weeks later will type II pneumocytes proliferate and differentiate into type I to rebuild the epithelium.
- In the repair phase new connective tissue formation will cause distortion of the lung architecture and shrinkage of the lungs. A new basement membrane is formed, which incorporates the connective tissue into the interstitium.
Neonatal respiratory distress syndrome (NRDS) is a similar syndrome. It mostly occurs in premature new-borns. It occurs when the babies’ lungs don’t produce enough pulmonary surfactant, which causes the lungs to collapse. The collapsed alveoli rub into each other, damaging the alveolar walls. Fibrin-rich exudate leaks into the alveoli, causing hyaline membranes to form. This blocks gas exchange, which further decreases the level of surfactant.
Infants with this condition are put on respiratory support. If they stay on respiratory support for a long time (weeks) this can cause injury to the alveolar septa, which decreases the number of alveoli and the respiratory surface. This is called bronchopulmonary dysplasia. Giving the infants lower levels of oxygen appears to prevent this from happening.