Table of Contents
Page created on September 29, 2018. Last updated on December 18, 2024 at 16:56
Summary
Heart failure is the condition where the heart is unable to pump enough blood to meet the needs of the body. Most failing hearts can maintain a 5 L/min cardiac output during rest. However, their cardiac output can’t increase when the body requires more perfusion, such as during exercise. Only when the demand for CO increases will the failing heart cause symptoms, except in the very late stages of heart failure.
People with heart failure utilize three compensatory mechanisms to try to increase their CO:
- Activation of RAAS -> increased salt and water retention
- High sympathetic activity -> increased heart rate
- Hypertrophy of the left ventricle
These compensatory mechanisms manage to increase the CO, but they cause other problems.
Cardiac output distribution
In rest is the cardiac output distributed as follows:
- Veins have 75-80%, arteries have 15% and the capillaries have 5-10% of the blood volume
- The brain receives 15% of CO
- The splanchnic organs receive 30%
- The skin receives 10%
- The kidneys receive 25%
- The coronaries receive 5%
Along with the table in topic 2.
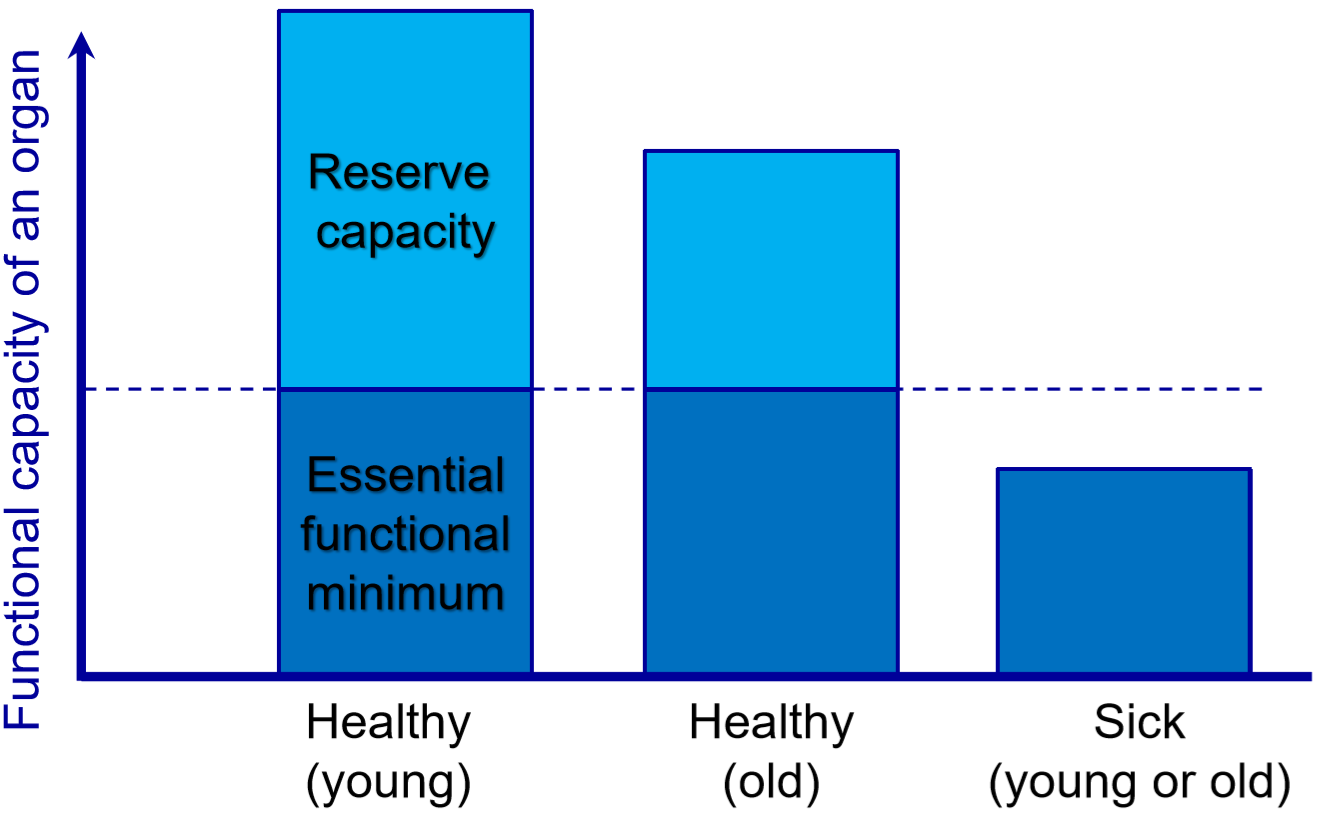
As we saw in the previous topic, the hearts of healthy people have a capacity to increase their cardiac outputs significantly when needed. They have a large reserve capacity. This reserve capacity becomes smaller with age but is still considerable, even in old age. However, sick and failing hearts don’t have a lot of reserve capacity; the most failing hearts may even be unable to uphold the resting cardiac output of 5 L/min!
Heart failure
Heart failure is an important condition which requires proper explanation. Because the condition is spread across multiple topics, it’s difficult to explain it properly. Therefore, I’ve decided to introduce it properly in this topic, although that doesn’t necessarily mean that all this information belongs under this specific topic.
Definition
When the heart is unable to pump sufficiently to maintain the CO to meet the body’s needs, there is heart failure. In most cases when we talk about heart failure we mean chronic heart failure, which the patient cannot be cured of. Many forms of heart failure exist, as we will see.
Heart failure is not an etiology; it’s a clinical syndrome. There are many causes of heart failure. The most common causes are hypertension and ischaemic heart disease like myocardial infarction. The left ventricle and the right ventricle may fail separately, but the failure of one ventricle usually leads to the failure of the other. More about this in later topics.
Heart failure is a clinical syndrome where the patient has symptoms and/or signs of insufficient cardiac output (“forward” symptoms) and/or backwards congestion (“backward” symptoms). This is due to an underlying decrease in systolic or diastolic function of the heart. Decreased systolic function refers to decreased ability of the heart to eject blood, reflected as a decreased left ventricular ejection fraction (LVEF, usually shortened to simply EF). Decreased diastolic function refers to decreased ability of the heart to fill with blood.
Not all people with heart failure have symptoms of volume overload, and as such, the term “congestive” heart failure is no longer preferred.
Some people with heart failure experience a stable course throughout their life, with no worsening of their symptoms. However, most people with HF experience at least one episode of worsening. This is called an acute decompensation or an exacerbation, and may occur over days or weeks or months. From there, the condition may continue to worsen or return to the condition before the worsening.
The mortality of heart failure has decreased significantly with modern treatment. According to one study, the 1-year mortality without medical therapy was approximately 52%, but with optimal modern medical therapy the 1-year mortality was approximately 7%.
Biomarkers
There are several biomarkers for heart failure, the most important ones being BNP and NT-proBNP.
The serum levels of brain natriuretic peptide (BNP, which is produced in the ventricles despite the name) correlates closely with the degree of heart failure. NT-proBNP is a precursor of BNP and a laboratory parameter which is used to measure the degree of heart failure in patients.
Compensatory mechanisms
When people with failing hearts exercise their hearts cannot increase the CO by the physiological mechanisms, as the myocardium is dysfunctional somehow. Instead, their bodies will employ these three compensatory mechanisms. These mechanisms try to increase the cardiac output during exercise despite the dysfunctional myocardium:
- Decreased stimulation of baroreceptors -> sympathetic activity ↑ -> Heart rate ↑, contractility ↑
- Low CO -> GFR ↓ -> RAAS activation -> salt and water retention ↑ -> preload ↑
- EDp ↑ -> Hypertrophy of ventricles
The cardiac output increase by these mechanisms is significant, which enables patients with heart failure to maintain a 5 L/min CO in rest, despite their failing heart. However their reserve capacity is always smaller than in healthy individuals.
When healthy people exercise, they experience sympathetic activation. This vasoconstricts all arterioles. However, their muscles produce vasodilators which overcome this vasoconstriction in the vessels of the active muscles. This decreases the total peripheral resistance.
When the sympathetic nervous system is activated during heart failure there is no vasodilation in the muscles. This means that there is vasoconstriction in all arterioles in the body, which increases the total peripheral resistance and therefore the afterload the heart must pump against. This impairs cardiac output, and is one of the reasons why these compensatory mechanisms cannot increase the cardiac output sufficiently during exercise.
The activation of RAAS will increase preload. However, angiotensin II is a potent vasoconstriction, which will increase the total peripheral resistance further, further increaseing the afterload.
Hypertrophy of the myocardium is effective in increasing its contractility. However, hypertrophic myocardium has three downsides. First, it’s less compliant. This increases the end-diastolic pressure in the ventricles, which impairs ventricular filling. Second, hypertrophic myocardium also requires more oxygen, which can predispose to ischaemic heart disease. Third, hypertrophic myocardium undergoes a process called myocardial remodeling, which is a series of histopathological changes in the myocardium which causes the ventricular performance to progressively decline. Hence, the compensatory mechanisms which allow sufficient cardiac output acutely will cause a long-term worsening of the cardiac output.
When ventricles are less compliant does it become more difficult to fill them up. Because of this can’t the EDV be increased without a higher end-diastolic pressure (EDp). This increased pressure will increase wall tension in the ventricle and impair the subendocardial blood flow. More about this here.
States of compensation
Most patients with heart failure are well-compensated while resting, meaning that these compensatory mechanisms enable their hearts to provide at least 5 L/min. However, once they do anything that increases the body’s need for cardiac output, like walking up stairs, experiencing heat or do light exercise the compensatory mechanisms will become insufficient to keep up with the required cardiac output. Most patients with heart failure are in this subcompensated state, meaning that they are compensated in rest, and so they only experience symptoms during exercise when the heart becomes decompensated. The worse the degree of heart failure, the less activity can the patient do before experiencing symptoms.
Decompensation is the temporary state where a patient with heart failure starts to experience symptoms of, like early fatigue and tiredness, dyspnoea and nocturia, or when the compensatory mechanisms themselves produce symptoms, like tachycardia or venous congestion. It’s called decompensation because there are no further compensatory mechanisms that can increase the cardiac output. Most patients only get decompensated during activity, so the symptoms will improve with rest.
In end-stage (severe) heart failures will it be difficult to maintain cardiac output even in rest with these compensatory mechanisms. In these cases will blood be redistributed between organs, to keep the vital organs (brain, heart) perfused sufficiently while the other organs go hypoperfused. This will lead to cardiogenic shock. In end-stage chronic heart failure will every organ except the brain receive less than normal blood perfusion because the CO can be as low as 3.5 L/min!
NYHA functional classification
The amount of exercise a patient can do before becoming decompensated obviously depends on the degree of heart failure. The New York Heart Association (NYHA) has created a classification system for heart failure that is widely used. It’s very simple:
- NYHA I – Heart failure with no clinical symptoms
- NYHA II – Heart failure symptoms occur after walking 2-3 flights of stairs
- NYHA III – Heart failure symptoms occur after walking on flat ground
- NYHA IV – Heart failure symptoms occur during rest or minimal activity