Page created on May 22, 2019. Last updated on December 18, 2024 at 16:56
I recommend reading through the internal medicine topic 3 for a better introduction to this topic.
Introduction
The cardiac conduction system goes from the SA node -> atria -> AV node -> His bundle -> Purkinje fibres -> ventricles. Block at the area of the SA node is called SA block while block at the area of the AV node is called AV block.
Etiology:
- Ischaemic heart disease
- AMI
- Cardiomyopathy
- Myocarditis
- High vagal tone
- Drugs
- Digitalis
- Beta blockers
- Electrolyte abnormalities
SA block
SA block refers to the impaired impulse conduction from the SA node to the atrial tissue. It has very little clinical importance, so it should be enough if you know that it exists.
ECG morphology:
We classify four types:
- 1st degree SA block
- 2nd degree SA block
- Type I
- Type II
- 3rd degree SA block
1st degree SA block: Impulses from the SA node reaches the atria with a delay. This is impossible to see on a normal ECG.
Type I 2nd degree SA block: The time it takes for the signal to travel from the SA node to the atria increases with each beat. This also means that the P-P intervals become shorter with every beat. This progresses until one impulse is completely blocked and a P-wave is skipped. A pause occurs and the P-P interval begins again at normal length.
The fact that the P-P interval becomes shorter and not longer is counterintuitive, but correct. It’s because the time it takes for the signal to reach the atria from the SA node increases with each beat. Either way it’s not that important to understand the reason behind it.
Type II 2nd degree SA block: Impulses from the SA node are blocked at random intervals, or every second impulse is blocked (advanced block). An advanced block cannot be distinguished from sinus bradycardia on an ECG.
3rd degree SA block: No impulses are conducted from the SA node. There is asystole (isoelectric line). An escape rhythm may develop and continue to provide cardiac output. If an escape rhythm doesn’t develop, cardiac arrest occurs.
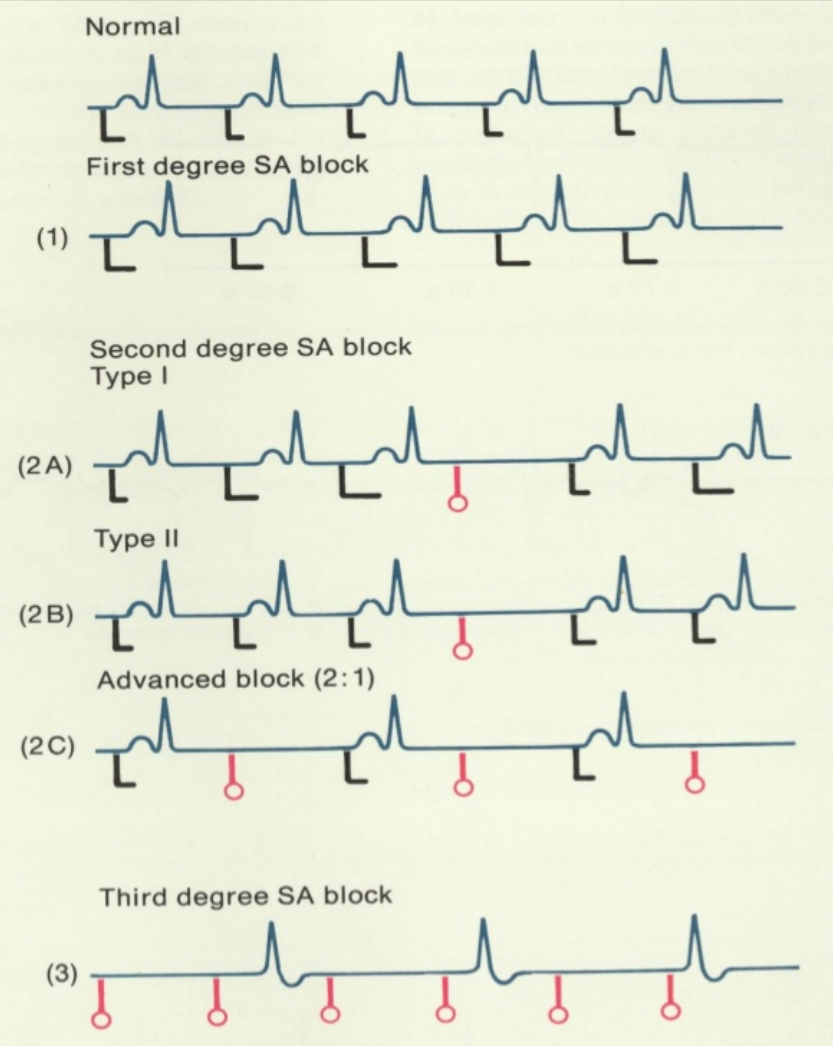
The black lines show when the SA node fires and the time it takes for the impulse to reach the atria (the P-wave). The red lines show where impulses from the SA node are blocked. From https://www.slideshare.net/thrs/arrhythmia-ecg-bradycardia20120909
AV block
AV block refers to the impaired conduction of signals through the AV node. It is much more important than SA block and should be the focus of this topic.
ECG morphology:
We classify four types:
- 1st degree AV block
- 2nd degree AV block
- Mobitz type I (Wenckebach phenomenon)
- Mobitz type II
- 3rd degree AV block
1st degree AV block: The PR-interval is abnormally long (> 200 ms).
2nd degree AV block Mobitz type I: The PR-interval becomes progressively longer until a beat is not conducted at all.
2nd degree AV block Mobitz type II: The PR-interval is fixed, but some beats are not conducted. The non-conducted beats can occur randomly or in patterns. A 2:1 block is when every other beat is conducted to the ventricles. A 3:1 block is when only one out of three beats are conducted to the ventricles. A 3:2 block is when two out of three beats are conducted to the ventricles.
3rd degree AV block: No impulses are conducted to the ventricles. An escape rhythm must kick in to preserve cardiac output. If an escape rhythm develops, the atrial and ventricular rate will be dissociated.
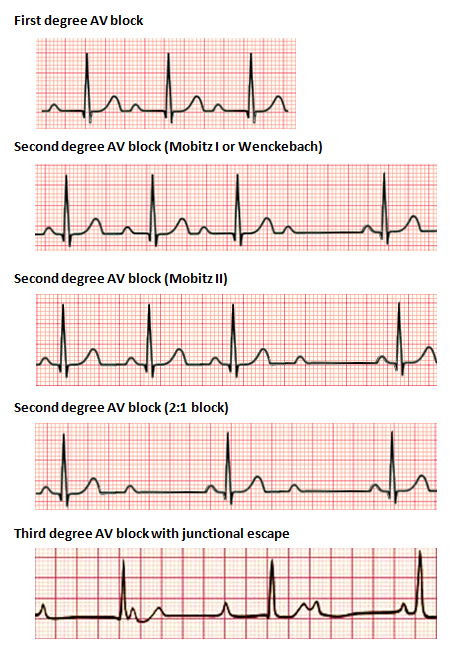
From https://en.wikipedia.org/wiki/Heart_block
Clinical features:
1st degree AV block is usually asymptomatic and requires no treatment. It is often an incidental finding.
2nd degree AV block Mobitz type I is also usually asymptomatic. In symptomatic people it may cause an irregular pulse and it may cause symptoms of cerebral hypoperfusion.
2nd degree AV block Mobitz type II is rarely asymptomatic. Symptoms of cerebral hypoperfusion and chest pain can occur.
3rd degree AV block requires an escape rhythm to be survivable. If an escape rhythm develops symptoms of cerebral hypoperfusion, dyspnoea and heart failure can occur. A Stokes-Adams attack may occur while waiting for the escape rhythm to kick in. If an escape rhythm doesn’t develop cardiac arrest occurs.
Treatment:
In symptomatic cases any underlying condition should be treated. If that’s not possible, a permanent pacemaker can be placed.