Table of Contents
Page created on October 24, 2018. Last updated on December 18, 2024 at 16:56
The V/Q ratio
Respiration is the most effective when gas exchange takes place in a well-ventilated alveolus while the capillary blood supply of the alveolus is good. We need a method to evaluate this, so we introduce two new symbols. V is the alveolar ventilation, while Q is the perialveolar capillary blood perfusion. They’re both measured in litres per minute. We often talk about the ratio between the two, the ventilation/perfusion ratio, or V/Q ratio.
As we saw in topic 43, ventilation of the alveoli in the base of the lung is higher than in the apex of the lung. Ventilation increases from the apex to the base of the lung, mostly because of gravity.
Perfusion is also different in the different parts of the lung. Like ventilation is it higher in the base of the lung than in the apex. This is also due to gravity: the pulmonary arteries enter the lung in the middle, so blood flowing to the apex must fight gravity while blood flowing to the base is helped by gravity.
While both ventilation and perfusion increase toward the base is it important to understand that perfusion increases much more. In other words, the difference in perfusion between the base and apex is much larger than the difference in ventilation between the same parts. Ventilation at the base is only approximately 20% larger than in the apex, but perfusion is more than 100% larger.
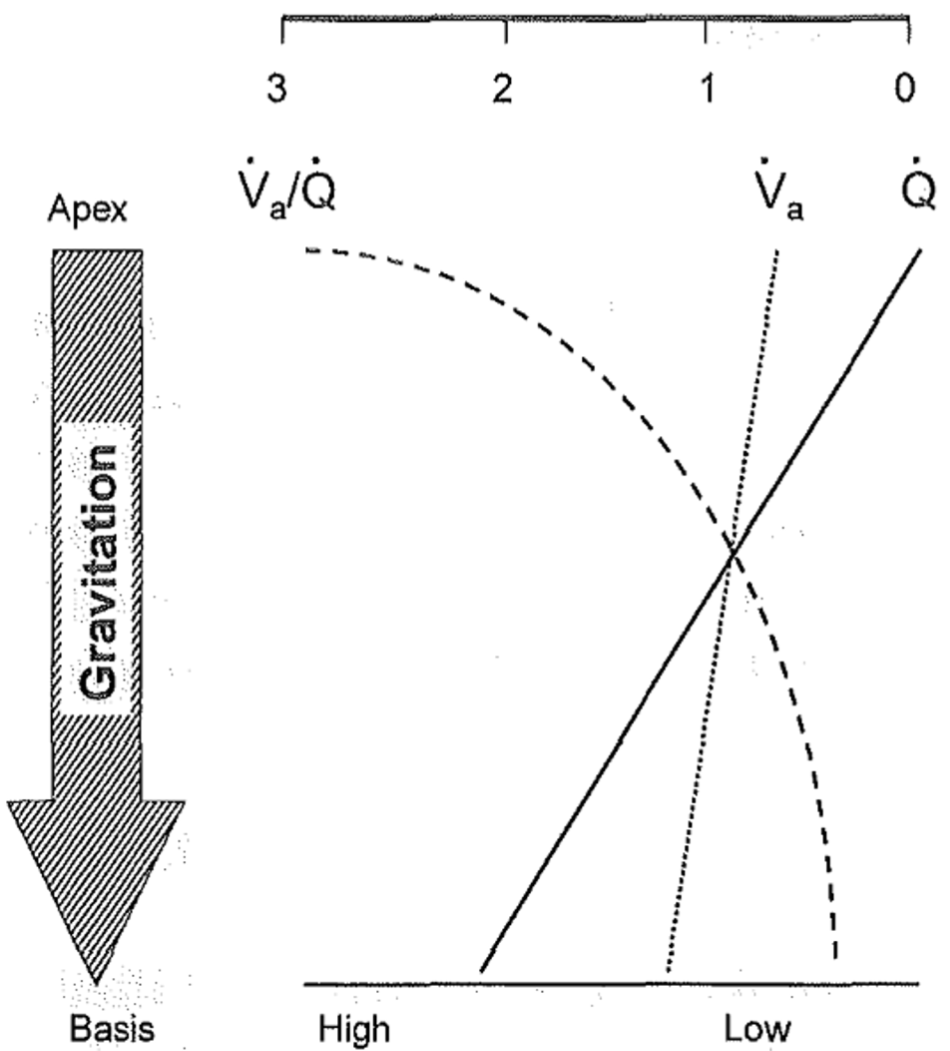
As seen on the figure, both V and Q increase (go further left) toward the base of the lung, however Q increases more than V. The V/Q ratio also changes considerably depending on where we are in the lung, from over 3 at the apex to below 1 at the base. We consider the V/Q ratio for a healthy lung as a whole to be just below 1, around 0.8, even though this is true only for the middle part of the lung, as seen on the figure.
Ideally the V/Q ratio of the whole lung would be 1, meaning that we have just enough perfusion of the alveoli to saturate the blood fully with oxygen. When this ratio deviates far from 1 we call it V/Q ratio mismatching.
Decreased ventilation/perfusion ratio
When the V/Q ratio is decreased the ventilation is lower than the perfusion. Decreased V/Q ratio is seen in any disorder where ventilation is impaired, like:
- Chronic bronchitis
- Atelectasis
- Bronchial obstruction
- Asthma
- Hepatopulmonary syndrome
- Pulmonary oedema
When an area of the lung has perfusion but no ventilation (V/Q = 0) it’s called a “shunt”, because blood passing through this area receives no gas exchange, as if shunted through an arterio-venous shunt (even though no new vessels are formed). When blood flows past an unventilated alveolus the blood flow serve no “purpose” with regards to gas exchange, it just flows from the arterial to the venous end without being oxygenated.
A low V/Q ratio means that the blood flowing around the alveoli will be incompletely oxygenated, causing hypoxaemia and hypercapnia. The hypercapnia will induce hyperventilation, to compensate.
The lung has mechanisms to compensate for a low V/Q ratio in localized parts of the lung. If a part of the lung has low V/Q ratio there will be a local vasoconstriction in the area, which reduces the perfusion (Q) to increase the V/Q ratio, and to redirect the blood to other, well-ventilated areas of the lung.
A small degree of shunting is normal. 2-3% of the total pulmonary perfusion is supplied by the bronchial arteries and will be drained by the pulmonary veins. This blood won’t be exposed to alveolar air, so it doesn’t contribute to gas exchange. This type of shunt is called anatomical shunt. We also have a functional shunt, as the basal part of the lung naturally has a low V/Q ratio. The presence of these two shunts shows means that around 4-6% of the pulmonary circulation is shunted (not exposed to air and oxygenated).
If there is some ventilation (V/Q is above 0) the hypoxaemia caused by the low ventilation can be compensated for by supplying the patient with 100% pure O2. If ventilation is 0, giving pure O2 wouldn’t help
Increased ventilation/perfusion ratio
When the capillaries supplying the alveoli is obstructed the perfusion (Q) will be very low or even 0, meaning that the V/Q ratio increases toward infinity. Because there is no gas exchange the air inside the alveoli will have the same gas composition as the outside air.
When perfusion of an area becomes zero will the area effectively become dead space.
Increased V/Q ratio is seen in:
- Emphysema
- Pulmonary embolism
Emphysema increases the volume of the lungs that can be ventilated, however this extra volume doesn’t receive any extra blood supply, meaning that the V/Q ratio increases.
In pulmonary embolism the capillaries supplying the alveoli will become obstructed, reducing the blood supply and increasing the V/Q ratio.
Consequences of V/Q mismatching
Whether V/Q is increased or decreased there will be hypoxaemia. In the beginning there be will normocapnia, meaning there is only a partial respiratory failure. A severe V/Q mismatching may eventually yield hypercapnia, meaning that the respiratory failure becomes global instead of partial.
“This blood doesn’t contribute to gas exchange, so it will be exposed to alveolar air.” ?
Fixed now.
Yes, I agree.
In the book at page 103, it says that emphysema decreases the respiratory surface by atelectasis and bullae, in addition to decrease the diffusion. It decreases both V and Q.
Okay, but on page 100 it says that V/Q is increased. It’s entirely possible that both V and Q decrease while V/Q increases, as long as Q decreases more than V, which is probably the case here.
Please which book is it that you guys are talking about? I am new to this page and I am a medical student in Ghana.
Our university has written its own book on pathophysiology, intended to cover the curriculum for our exam. (It’s not good)