Page created on October 25, 2018. Last updated on December 18, 2024 at 16:56
Up until now have we talked about ventilation. Now let’s talk about diffusion.
Alveolo-capillary diffusion
Oxygen gets to the perialveolar capillaries by diffusion from the alveolar space, and carbon dioxide diffuses the opposite direction. Diffusion happens across the alveolo-capillary or diffusion membrane, which has the following layers:
- Alveolar epithelial cell (type 1 pneumocyte)
- Alveolar basement membrane
- Interstitium
- Capillary basement membrane
- Capillary endothelium
There are many layers, however the distance from the alveoli till the capillaries is just a few µm long, much shorter than the diameter of a red blood cell!
On the two sides of the diffusion membrane are the partial pressures of oxygen and carbon dioxide different. They’re summed up in the table below:
| Carbon dioxide | Oxygen | |
| Capillary | 46 mmHg | 40 mmHg |
| Alveolus | 40 mmHg | 100 mmHg |
| Pressure difference | 6 mmHg | 60 mmHg |
As we can see is the pressure difference much smaller for carbon dioxide than for oxygen. This is because CO2 naturally diffuses more easily, so it doesn’t need a large pressure gradient to diffuse in satisfactory amounts. Oxygen however doesn’t diffuse so easily, so it needs a much larger pressure gradient to diffuse enough.
The surface of the lung that can be used for diffusion is normally 70 – 90 m2.
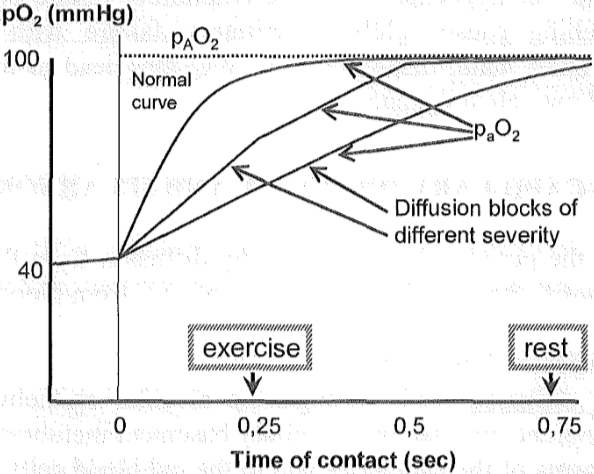
Diffusion isn’t an instant process; it takes some time. If the blood flow is way too quick, it won’t “stay around” long enough around the alveoli to be sufficiently filled with oxygen. Thankfully isn’t this a problem in healthy persons. This contact time or diffusion time is 0.75 seconds in rest, which is enough for the partial pressure of O2 in the capillaries to increase from 40 to 100 mmHg. In exercise will the blood flow more quickly, meaning that the contact time is reduced to just 0.25 seconds. This isn’t a problem however, as most of the diffusion is done in the first 0.25 seconds anyway. pO2 doesn’t increase to quite 100 mmHg but very close.
Any of these four factors (length of diffusion membrane, pressure gradients, diffusion surface and diffusion time) can be abnormal and lead to poor perfusion.
Causes of diffusion disorders
Disorders that give longer diffusion route are:
- Thickened alveolar wall
- Pulmonary oedema (fluid in the alveolar spaces)
- Thickened capillary membrane
- Wet lung (fluid in the interstitium)
- Severe left ventricular failure
- Acute respiratory distress syndrome
- Interstitial lung diseases
- Silicosis
- Sarcoidosis
- Tuberculosis
We rarely see disorders of the pressure gradients. It’s only seen in high altitude, when the oxygen tension in the air is low, which will reduce the pressure gradient of oxygen.
Disorders that yield reduced respiratory surface are:
- Resection of the lung
- Lung parenchyme destruction
- Fibrosis
- Pneumonia
- Atelectasis
- Emphysema
Decreasing the contact time occurs in widespread destruction or obstruction of capillaries. The remaining capillaries will receive such a fast blood flow that the contact time becomes insufficiently low and the O2 diffusion is strongly affected. CO2 isn’t really affected because it diffuses very easily anyway. This mostly just occurs in advanced stages of fibrosis.
Hepatopulmonary syndrome
Patients that have chronic liver failure, often due to cirrhosis, can sometimes develop respiratory symptoms as well. Interestingly will these patients have dyspnoea and hypoxaemia, but only in standing, orthostatic position! The term for dyspnoea that occurs only while standing is platypnoea, and the term for hypoxaemia that occurs only in the same condition is orthodeoxia.
Recall that ventilation is different in different parts of the lung; it’s lowest in the apex and highest in the base. These changes are due to gravity, so they only occur while standing. In supine position is the ventilation and perfusion mostly the same everywhere in the lung.
Recall that when the V/Q ratio decreases because of either decreased ventilation or increased perfusion will a shunt be formed, because blood passes from the arterial to the venous side without being fully oxygenized. To avoid this will the lungs vasoconstrict the vessels in the area where the V/Q is too low.
The pathogenesis of hepatopulmonary syndrome is only partially known. We know that the liver clears the blood of vasodilators like NO. In liver disease will the liver’s capacity to remove vasodilators be decreased, meaning that vasodilators will travel to the lungs and dilate the vessels there.
The dilation causes a V/Q mismatch by preventing the lung from vasoconstricting vessels in the base of the lung to increase the V/Q ratio when the patients stands up.
The dilated vessels in the lung will have such a large diameter that the diffusion route will be longer. Oxygen can’t diffuse into the centre of the vessel, only to the periphery of the vessel. This means that only parts of the blood will be saturated with oxygen, effectively causing a diffusion abnormality.
Hi, Nik
It is important, since the center of the vessel will be some kind of a shunt, and will not be oxygenated. If then less blood gets oxygenated, hypoxia will be provoked.
The amount of peripheral blood that gets oxygenated can’t just give off their oxygen to their neighbors. It will leave them with no oxygen themselves.
Unfortunately I still don’t understand.
I don’t feel like your explanation answered any of my questions. How is it different whether the oxygen is in the periphery or centre of the vessel? Oxygen is dissolved in the blood, as soon as it reaches the periphery of the vessel shouldn’t it dissolve uniformly in the whole vessel? Blood flow isn’t perfectly laminar, so any blood in the periphery of the vessel will get mixed with the blood in the centre. How is a shunt formed in the centre of a vessel? This doesn’t make sense to me.
Anyway, that explanation doesn’t explain the orthodeoxia, which my explanation does.
Hello, Nik!
This came up as an question during one of the lectures. Mártha said a good answer would be that:
“When you have a cirrhosis, the livers ability to eliminate, let’s say vasodilators, is vanished. Therefore the vasodilators continues their way toward the lungs, causing a vasodilation there. This will of course increase the diameter of the vessels. The oxygen trapped in the middle of this vessel will not be able to diffuse into the alveoli! (The CO2 will, be able to diffuse). This will cause hypoxia and normocapnia(partial respiratory failure).”
Hey. I appreciate it. Also, since I wrote this topic has the department published a document with details on hepatopulmonary syndrome.
I like your explanation, but I don’t understand why oxygen would diffuse into the alveoli. Could you explain?
The document writes this:
But I don’t understand the part where oxygen only reaches the peripheral part. The peripheral part of what? The vessel? Why does it matter for gas exchange that oxygen only reaches the periphery of the vessel?
Hi, Nik
The diffused oxygen, from the alveoli, only reaches the outermost part of the vessels. The peripheral part. The distance between the center of the vessel and the alveoli is to large for oxygen to diffuse. (Imagine that oxygen is able to diffundate 30 micrometer, but the distance from the alveoli to the center of the vessel is 50 micrometer.)
It is, due to this fact, that there is somewhat of a shunt formation. The blood in the center of the vessel don’t change their content, it will leave the pulmonary circulation as it came.
Okay, I understand that oxygen can’t travel to the centre of the vessel, but why is that important? Won’t oxygen diffuse freely around in the blood until it binds to haemoglobin anyway?
I don’t understand how the oxygen being in the periphery of the vessel affects the oxygen tension in the blood. It’s still in the blood?