Table of Contents
Page created on October 28, 2018. Last updated on December 18, 2024 at 16:56
Obstructive pulmonary disorders
In obstructive lung diseases is the non-elastic airway resistance increased, mostly during expiration. It can be due to extrathoracic or intrathoracic obstructions.
When extrathoracic obstructions are present is inspiration hampered while expiration is mostly normal. Examples of extrathoracic obstructions include:
- Post-intubation hardening of the trachea
- Compression of trachea
- Goitre
- Tumour
- Laryngeal spasm
Extrathoracic obstruction is often accompanied by stridor, a high-pitched sound on inspiration.
Intrathoracic obstructions are much more frequent. The most common types are the chronic obstructive pulmonary diseases (COPD) and asthma.
Chronic obstructive pulmonary diseases
COPD is a progressive airway obstruction that may partially be reversible. Two diseases belong to the COPD group. They are chronic bronchitis and emphysema. Chronic bronchitis accounts for 85% of COPD cases while emphysema accounts for 10%.
COPD is diagnosed based on three criteria.
- FEV1 < 80% of predicted FEV1
- Tiffeneau index (FEV1/FVC) < 70%
- Only partially reversible upon administration of bronchodilator
FEV1 varies considerably depending on height, gender, weight and other factors. A normal value of FEV1 for every patient will be calculated based on these factors. If the patient’s actual measured FEV1 is less than 80% of this “predicted” FEV1 will this point to COPD.
The third criterium is based on the degree of which the symptoms get better after giving bronchodilators to the patient. We usually say that if the values improve by less than 12% does this point to COPD. It’s usually phrased as “< 12 % amelioration”, where amelioration means “improvement”.
We can distinguish three phases of COPD. They’re summarized in the table below.
| Mild phase | Moderate phase | Severe phase | |
| FVC | < 80% | < 60% | < 50% |
| FEV1 | < 80% | < 60% | < 30-40 % |
| Tiffeneau index | < 70% | < 60% | < 40% |
All types of COPD can lead to chronic global respiratory failure.
Chronic bronchitis
Chronic bronchitis is characterized by increased bronchial secretion, chronic cough and enhanced sputum production. It’s either chronic or appears periodically (at least 2 months per year for 2 consecutive years.
It’s often caused by these factors:
- Active, chronic smoking (90% of cases)
- Occupational dust exposure
- Silicosis
- α1 antitrypsin deficiency (most important inherited factor)
- Air pollution (smog)
- Blood group “A”
- Vitamin C deficiency
- Alcoholism
Smoking is the most important factor in developing chronic bronchitis. Cigarette smoke contains many compounds that damage the airways, like polycyclic aromatic hydrocarbons. It damages the airways by many mechanisms:
- Paralyzes the mucociliary clearance
- Causes neutrophil inflammation of airways
- Hyperplasia of goblet cells
- Increased mucous secretion
- Promotes metaplasia of mucosa
- Inhibits the function of Lys-oxidase
The mechanisms are similar in air pollution and silicosis.
Cigarette smoke activates tissue macrophages in the lungs, which attract and active neutrophils. These neutrophils release neutrophil elastase and collagenase enzymes that break down the parenchyme. Lys-oxidase is an enzyme that has a protective role against parenchyme destruction by neutrophils.
The airway inflammation by neutrophils causes oedema and hyperplasia of the bronchial wall, which is what obstructs the bronchi. The increased mucus secretion from the increased number of goblet cells also contributes. The bronchial smooth muscle also develops a tendency to spasm. The mucosal metaplasia increases the risk for cancer.
During a medical procedure called bronchoalveolar lavage is a bronchoscope passed into the lungs and “washes” a small part of the lung with fluid. This fluid is then collected and examined. This bronchoalveolar lavage fluid contains neutrophils in patients with COPD.
α1 antitrypsin (A1AT) is an acute phase protein, produced by the liver during systemic inflammation. It’s a serine protease inhibitor. Its main function is to limit the damage caused by neutrophil elastase during inflammation. In the case where this protein is genetically deficient will the damage caused by neutrophils in the airways be significantly larger. The gene for A1AT is on chromosome 14.
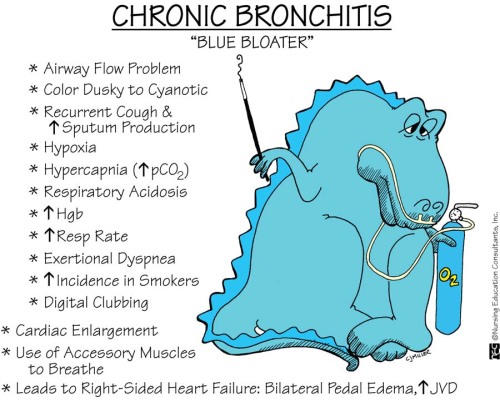
Some patients with chronic bronchitis have special characteristic that have given them the nickname “blue bloaters”. Blue because they’re cyanotic and bloaters because they’re often obese. Not all chronic bronchitis patients develop this morphology. The ones who do probably have an underlying primary alveolar hypoventilation.
Chronic bronchitis can be treated by muscarinic antagonists (bronchodilators), β2 agonists (bronchodilators), theophylline and glucocorticoids (prednisone).
Chronic bronchitis can in some cases lead to emphysema.
Emphysema
In emphysema are the septa between the alveoli destroyed. This causes the lung to be hyperinflated. Alveoli fuse and form bullas (singular: bulla), which reduces the total respiratory surface of the lung. Bullas give the lung a “bubble wrap” morphology.
Emphysema can occur primarily due to α1 antitrypsin deficiency or secondary due to smoking, or both.
In healthy people is there a balance between protease and antiprotease (A1AT) activity. In some people is this balance tilted toward protease activity, and these people can develop emphysema. This balance tilt can occur due to decreased antiprotease activity due to α1 antitrypsin deficiency or due to increased protease activity due to neutrophil inflammation in smoking.
We can distinguish two types of emphysema. Centrilobular emphysema occurs in smoking while panlobular emphysema occurs in α1 antitrypsin deficiency.
The proteases degrade and destroy the elastic fibres in the alveolar septa. This decreases the elastic recoil of the lung, meaning that the passive process of expiration becomes harder. Lung compliance becomes abnormally high. Destroyed elastic fibres also lead to some alveoli collapsing at expiration.
Because the alveolar septa are destroyed is the risk that bullas can burst very high. If this happens pneumothorax occurs.
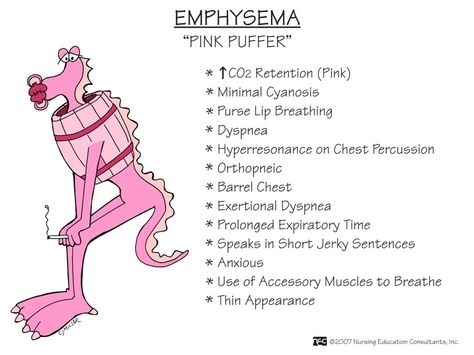
Like for chronic bronchitis does emphysema have a characteristic patient morphology. Patients usually have pinkish skin, barrel chest and are skinny.
Bronchial asthma
Bronchial asthma or just asthma is a disease characterized by episodes of paroxysmal (sudden), reversible bronchospasm including dyspnoea with wheezing. It can cease by itself but is often reversed by medication. Because of this is asthma not classified as a COPD. Between the asthmatic attacks do patients breathe normally.
Two forms of asthma exist. The intrinsic (non-allergic) type has unknown aetiology while the extrinsic (allergic) type is evoked by certain antigens. Genetics play a minor background role in both types. The increase in environmental factors like pollens and air pollution the last years has caused a sharp increase in asthma cases. The following factors increase the risk of developing asthma:
- Obesity
- Male gender
- Overenthusiastic hygiene
- Few infections during childhood
- No exposure to bacteria or parasites
- Bad diet
The following factors can trigger an asthmatic attack:
- Allergens
- Perfume
- Pollen
- House dust mites
- Mold
- Aspirin
- 3-5% of people with asthma can have asthma attacks triggered by aspirin
- Smoking
- Infections
- Exercise
- Air pollution
- Stress and anxiety
In patients with asthma are the airways chronically inflamed by eosinophilic inflammation. This inflammation is a type 1 hypersensitivity. This causes their airways to be hypersensitive to certain triggers. It begins with the first exposure to an allergen. Antigen-presenting cells will phagocytose the allergen and present it to a T-helper cell, turning and turn it into a Th-2 helper cell. The Th-2 cell and APCs will produce IL-4 and IL-5. IL-4 cause B-cells to produce IgE antibodies against the allergen. The antibodies will attach to the surface of mast cells. The mast cells are now sensitized.
IL-5 recruits and activates eosinophils, causing the eosinophil inflammation. It also induces oedema, increased mucous secretion and bronchial smooth muscle contraction.
When the allergen later reappears will the mast cells immediately recognize it and release its granules (a process called degranulation). These granules contain prostaglandins, thromboxanes, platelet activating factor and most importantly leukotrienes. The leukotrienes are what induce the smooth muscle contraction that causes the bronchospasm.
Asthma can’t be cured, but symptoms can be reduced. It is treated by administering:
- β2-agonists by inhalation
- Anticholinergic drugs (muscarinic M3 antagonists)
- Corticosteroids by inhalation
- Theophyllin
I am not sure of the cause of COPD emphysema in my case. I smoked pack a day for 12 or 13 years, but quit 40 years ago. I have been an outdoor person all my adult life. Coughing started last summer producing thick mucus, greenish tint to clear. I tried prednisone and antibiotics, but no change. X-rays are negative, heart lungs and blood and serum chemistries all are normal. I have lung calcification from childhood bout with histoplasmosis. I am 75 years old and retired.My current doctor directed me to totalcureherbsfoundation .c om which I purchase the COPD herbal remedies from them ,they are located in Johannesburg, the herbal treatment has effectively reduce all my symptoms totally, am waiting to complete the 15 weeks usage because they guaranteed me total cure.
cool story bro