Table of Contents
Page created on December 11, 2018. Last updated on December 18, 2024 at 16:56
General about blood
The most important components of the blood are:
| Component | Concentration |
| Na+ | 135 – 145 mmol/L |
| K+ | 3.5 – 5.0 mmol/L |
| Ca2+ | 2.3 – 2.7 mmol/L |
| Cl– | 100 – 106 mmol/L |
| Protein | 60-84 g/L |
| Albumin | 35-50 g/L |
| Haemoglobin | 140 – 160 g/L |
| RBCs | 4 – 5 million/μL or 4 – 5 trillion (T) /L |
Cells in the body communicate with the outside world via the extracellular spaces. The most important EC spaces are:
- Interstitial fluid
- Blood plasma
- Lymph
- Cerebrospinal fluid
- Aqueous humour
The function of blood is to transport oxygen, carbon dioxide, glucose, metabolites, plasma proteins, hormones and other compounds between these extracellular spaces.
RBCs
Erythropoietin (EPO) is the most important hormone in the regulation of erythropoiesis, although both cortisol and androgens stimulate EPO production. EPO is produced in the peritubular interstitial cells in the kidney in response to hypoxia.
Many compounds are necessary to produce RBCs, mainly:
- Protein – for globin formation
- Iron – for heme synthesis
- Folic acid and B12
RBCs have a characteristic shape, namely they’re biconcave discs (discs where both sides are concave).
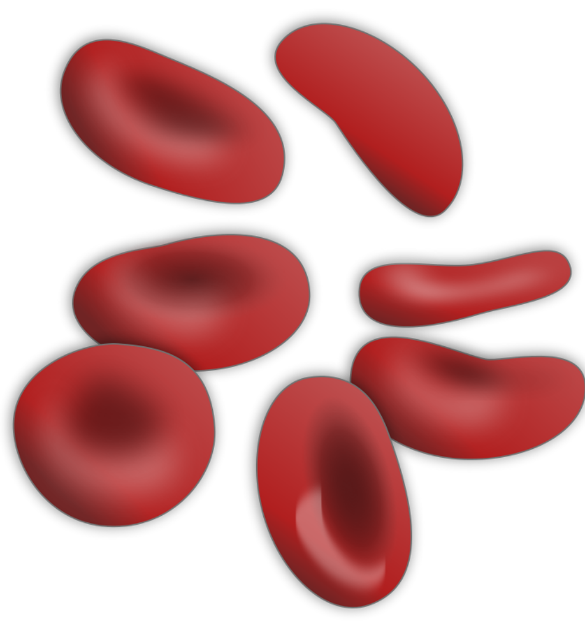
Their diameter is 5 – 7 µm. Red blood cell distribution width (RDW) is a measure of how variable the blood cells in a sample is. When it is abnormally high does it mean that the RBCs in that sample have very different sizes, which is characteristic for some anaemias. High RDW measures the degree of anisocytosis. The word means “not” + “similar” + “cell size”. Anisocytosis is important because many anaemias have anisocytosis as a characteristic feature, along with the average cell size (microcytosis, normocytosis or macrocytosis).
RBCs are incomplete cells without nuclei or mitochondria. Their cell membrane has high plasticity (ability to change shape) because the phospholipid cell membrane is supported by a strong but flexible protein network. Recall that the lumen of capillaries is only slightly larger than the diameter of RBCs, so RBCs inside capillaries are forced to flow in a single file. If the plasticity of the cell is impaired will RBC flow inside capillaries damage the membrane, which decreases the life span of the cells.
RBCs have two important enzyme systems: Glycolytic enzymes (they don’t have mitochondria after all) and pentose phosphate pathway enzymes (also called direct oxidation of glucose), most notable glucose 6-phosphate dehydrogenase. Of course is haemoglobin also important.
2,3-diphosphoglycerate (2,3-DPG, also called 2,3-BPG) is a by-product of glycolysis. As seen in topic 48 will the presence of 2,3-DPG shift the haemoglobin-oxygen dissociation curve to the right, which increases tissue oxygenation.
Anaemia
Anaemia is any condition where the Hb content in the blood decreases below 130 g/L in males or 120 g/L in females. However, small decreases won’t produce symptoms, because increased levels of factors like 2,3-DPG can compensate for the decreased Hb by increasing tissue oxygenation. Clinical symptoms occur when the Hb level is below 90 – 100 g/L. At Hb levels below 70 – 80 g/L will cardiac output increase, which can lead to high-output cardiac failure.
There are many ways the total Hb content of the blood can be reduced, like too few RBCs or too little Hb in the RBCs.
The size of RBCs is described as microcytic, normocytic or macrocytic. The haemoglobin content of RBCs directly affects the red colour intensity of the cells. We therefore use hypochromic, normochromic and hyperchromic to characterize the Hb content of each cell. However, the size of each red blood cell and its Hb content is very closely related, so anaemias are often normocytic and normochromic, or microcytic and hypochromic or macrocytic and hyperchromic.
We can classify anaemias based on two things; their morphology and their cause (etiology):
Morphological classification:
| Type | Cause |
| Microcytic and hypochromic | Iron deficiency or vitamin C deficiency |
| Normocytic and normochromic | Erythropoietin or protein deficiency, blood loss, haemolysis, aplastic anaemia |
| Macrocytic and hyperchromic | Vitamin B12 or folic acid deficiency, pernicious anemiae |
Etiological classification:
| Reduced RBC production: | ||
| Aplastic anaemia | Bone marrow suppression | |
| Deficiency anaemias | Iron, Folic acid, B12 or protein deficiency | |
| Other disease-associated forms | Chronic renal failure | |
| Impaired RBC lifespan (haemolytic anaemias): | ||
| Corpuscular anaemias | Abnormal membrane, enzyme deficiency, abnormal haemoglobin | |
| Extracorpuscular anaemias | Trauma, toxins, autoimmune diseases | |
Consequences of anaemia
Anaemias cause decreased tissue perfusion. That has the following most characteristic symptoms:
- Headache
- Somnolence
- Renal tubular hypoxia
- Pale skin
- Muscle weakness
Cardiac output will be increased to compensate for the low oxygen content. This causes the circulation to become hyperdynamic. Tachycardia is especially characteristic. If the anaemia is severe enough (<70 – 80 g/L) to cause high-output heart failure will the symptoms be the same as the symptoms of high-output heart failure. It’s at this point where the increased CO isn’t enough to compensate for the anaemia, so the body must start to redistribute the circulation to the heart and brain, leaving other organs susceptible to hypoxia. Venous congestion also occurs.
When the level of Hb in the blood decreases will the haemoglobin saturation actually increase (because there are fewer haemoglobin molecules to saturate), but the total arterial oxygen content will decrease. This causes anaemic hypoxia of peripheral tissues.
You won’t get hypoxemic hypoxia, because then you would have polyglobulia as compensation. That’s why this is anemic hypoxia. I still agree with you that the tissues are hypoxemic. That’s correct for both hypoxemic and anemic hypoxia.
Fixed. Thanks