Page created on September 29, 2018. Last updated on December 18, 2024 at 16:56
In high-output cardiac failure, the problem isn’t that the heart has an abnormally low capacity to increase or manage its cardiac output. The problem is rather that some peripheral or systemic condition causes the body to have an extraordinarily high demand for cardiac output! The heart will initially try to satisfy the tissues’ higher demand but over time, the heart will take damage for it.
The low-output variant is more frequent than the high-output variant.
| Low-output heart failure | High-output heart failure | |
| Peripheral oxygen demand | Normal | High |
| Cardiac function | Diminished | Initially normal |
| Cardiac output | Low | High |
| Primary cause | Heart or lung-related | Peripheral causes |
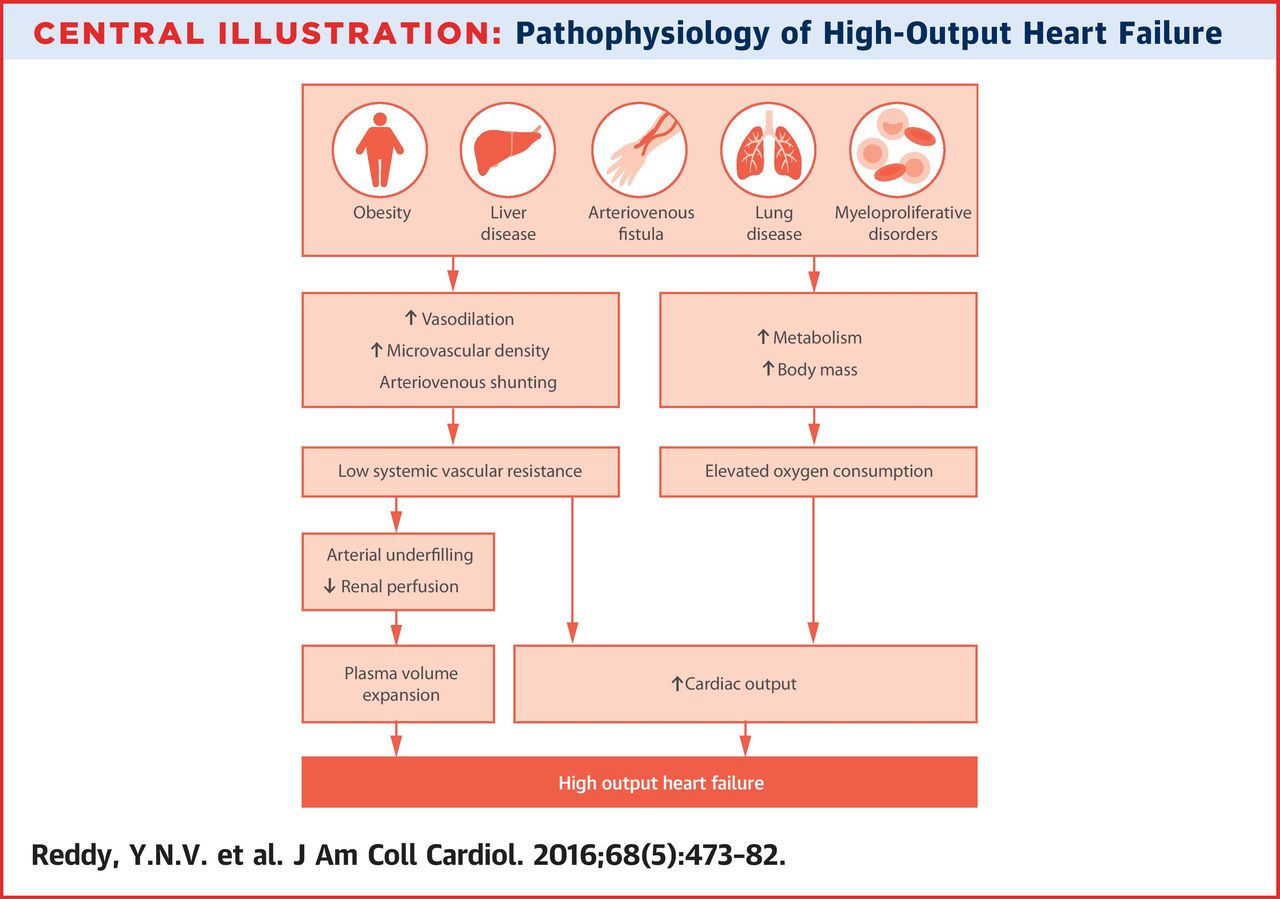
High-output cardiac failure is often seen in:
- Severe anaemia
- Arteriovenous fistula
- Wet beri-beri
- Hyperthyroidism
- Pregnancy
- Septic shock
- Hepatic disease and cirrhosis
High-output cardiac failure can develop either due to a decreased afterload or to an increase in preload. When afterload decreases or preload increases the heart will automatically increase contractility (Frank-Starling) and heart rate to keep up. This will increase stroke volume and cardiac output. The increased preload will increase the end-diastolic volume (due to increased filling) so much that the end-diastolic pressure also increases. This causes backward congestion in the veins together with general signs of backward failure.
Most of the total peripheral resistance comes from the high resistance in the arterioles. When an arteriovenous fistula develops the circulation can circumvent the arterioles and go through the fistula instead. This causes a large drop in total peripheral resistance, which again decreases the afterload, which must be compensated by the heart by increasing cardiac output.
In severe anaemia the tissues of the body will become hypoxic, which causes them to release by-products of anaerobic metabolism like lactate and adenosine. Both compounds are vasodilators, so when they’re released the vessels of the body dilate so that the total peripheral resistance decreases. Anaemia also reduces the haematocrit of the blood, which means that the viscosity (the thickness) of the blood will decrease as well. The decrease in TPR and viscosity decreases the afterload.
Beri-beri is caused by thiamine deficiency. A symptom of this deficiency is vasodilation of vessels due to the dysfunction of the muscles in the tunica media of the vessels.
In hyperthyroidism, all tissues are turned into a hypermetabolic state due to being overstimulated by the increased levels of thyroid hormones. This increases the tissues’ O2-demand, which warrants an increase in cardiac output. The increased metabolism also causes a vasodilation of the skin because the amount of heat the body must get rid of increases.
In hepatic disease porto-caval anastomoses inside the liver will be formed, which again lowers the TPR.
In septic shock the endotoxin produced by the bacteria will trigger significant vasodilation of the arterioles, which will decrease blood pressure and TPR.