Page created on December 15, 2018. Last updated on December 18, 2024 at 16:56
Uraemia and azotaemia
Azotaemia is defined as an elevation of waste products like urea and creatinine in the blood. This is not always symptomatic.
On the other hand, uraemia refers to the clinical symptoms which occur in response to the toxic effects of urea, creatinine and other waste products. Uraemia classically occurs in the setting of end stage renal disease (ESRD), the last stage of chronic kidney disease (CKD). Uraemia and end stage renal disease are sometimes used interchangeably.
Uraemia is caused by:
- Increased levels of:
- Nitrogen-containing waste products, like urea and creatinine
- H+ (proton)
- PO43- (phosphate)
- SO42- (sulphate)
- Aluminium
- Na+ (sodium)
- K+ (potassium)
- Hormones like insulin, glucagon, gastrin and prolactin
- Other uraemic toxins
- Urea
- Creatinine
- Guanidino compounds (Includes three molecules: MG (methylguanidine), GSA (guanidinosuccinic acid), GAA (guanidinoacetic acid))
- PTH
- Ammonia
- Uric acid
- Decreased levels of:
- Bicarbonate
- Calcium
- Iron
- Protein
BUN (blood urea nitrogen) measures the amount of nitrogen as part of the urea molecule in the blood, instead of measuring the amount of urea itself. It’s really silly and is mostly in use in USA and America-influenced countries. However, you can and should think of BUN as the same as the urea content in the blood. In Norway and Hungary we use the urea level instead of BUN. Urea is sometimes called carbamide
The urea level in the blood is called blood urea nitrogen (BUN). It’s normally between 6 and 20 mg/dL. Symptoms of uraemia start to appear when the BUN reaches around 80 mg/dL.
It’s difficult to pinpoint exactly at which phase of chronic kidney disease uraemia occurs, as it depends on several factors. Urea and creatinine levels in the serum have noticeable increase when GFR is below 50% of normal. However, phase I and II are often asymptomatic for the patient, even though they already have some degree of uraemia at phase II. Uraemia is most characteristic in end stage kidney disease, the last stage of chronic kidney disease.
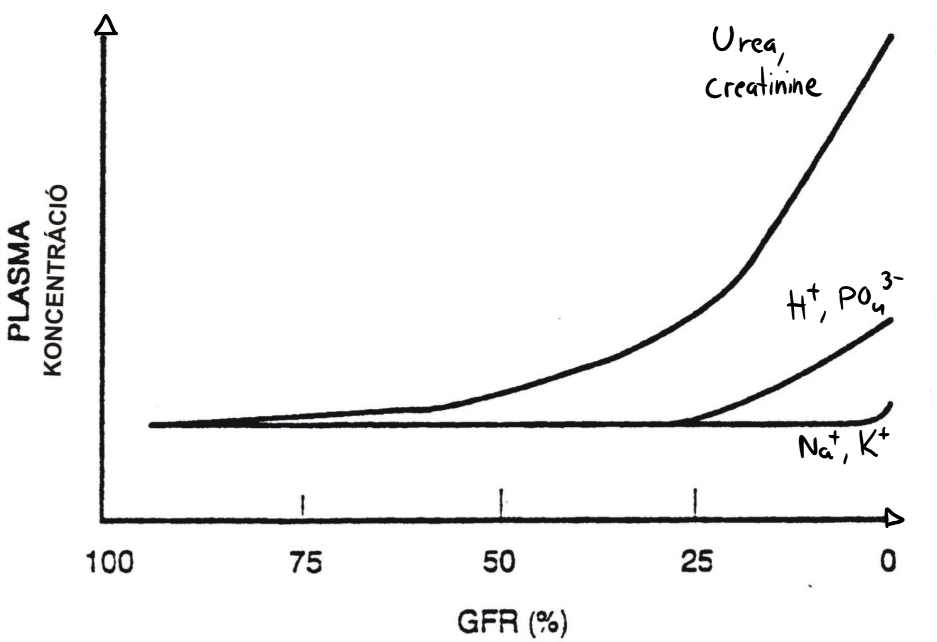
From topic 64. Recall that end-stage renal failure occurs when GFR is less than 15% than normal. At this point will the excretory functions be so impaired that phosphate and protons are retained.
Uraemic toxins
Not just one substance causes the problems in uraemia, but rather many. Uraemic toxins are substances that are normally present in very small amounts in the blood but are toxic when present in high concentration. The most important are:
- Urea
- Creatinine
- Guanidino compounds (Includes three molecules: MG, GSA, GAA)
- When urea accumulates will the urea cycle slow down, causing accumulation of arginine and ornithine. These amino acids will enter other pathways that form these guanidino compounds.
- PTH
- Ammonia
- Uric acid
These substances are toxic by the following mechanisms:
- They slow down cell metabolism by inhibiting enzymes non-specifically
- They increase membrane permeability
- They damage the neural, immune, haematopoietic and cardiovascular systems
- They demyelinate nerves
- They inhibit ADH secretion
Consequences of uraemia
Clinical features:
-
- Itching
- Fatigue
- Nausea, vomiting
- Ammonia-smelling breath
- Asterixis
- Uraemic encephalopathy (see topic 71)
Complications:
- Cardiovascular
- Hypertension (explained in topic 69)
- Myocardial impairment
- Rhythm abnormalities (due to electrolyte imbalance)
- Pericarditis
- Haematologic
- Anaemia (explained in topic 69)
- Increased risk of infection
- Respiratory
- Pleuritis
- Pulmonary oedema
- Metabolic
- Hypometabolism (due to enzyme inhibition)
- Glucose utilization decreases -> Hyperglycaemia
- Metabolic acidosis (due to increased H+ retention)
- Enhanced protein catabolism, which increases production of urea
- Bone deformities (explained in topic 69)
- Neuromuscular
- Muscle atrophy (due to protein deficiency)
- Peripheral neuropathy
Because of hyposthenuria is the failing kidney unable to deal with salt or water loads (increased salt or water intakes). Any of these will cause a quick rise in plasma volume, leading to fast development of oedema, not only in the periphery but in the lung as well. The rise in plasma volume also causes hypertension. Salt and water intake must therefore be regulated closely.
Also because of hyposthenuria is the kidney unable to regulate salt reabsorption, meaning that the serum sodium level is almost completely dependent on the salt intake. This means that salt intake also majorly affects the blood pressure and the tonicity. Excess salt intake will lead to hypertonicity.
Uraemia also has a macroscopical finding. Uraemic frost is a description for what looks like frost on the affected persons head. It occurs when the BUN level is above 200 mg/dL (not important), but is very uncommon nowadays as most people with renal failure are treated (mostly by dialysis), so that the BUN level never gets that high. Many physicians have never seen it as a result. The person’s sweat contains urea, and when the sweat evaporates will urea crystallize.
This is more of a fun fact. It’s not important to know.

Black man with dandruff? No, it’s uraemic frost.
Hi,
I was wondering what these three abreviated guanidino compounds are called? “MG, GSA, GAA”
Sincerely
Cristiano
Added, although it’s probably not important to know