Page created on November 18, 2018. Last updated on December 18, 2024 at 16:56
Type III hypersensitivity
This type of hypersensitivity is also called immune complex disease, as the whole premise of the disease is that so-called immune complexes deposit in vessels, causing inflammation. An immune complex is a complex that is formed when antibodies bind to antigens to form large complexes.
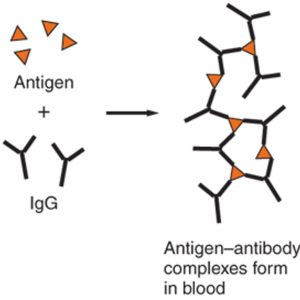
The antigens in this case may be exogenous, like microbial proteins, or endogenous proteins as in autoimmune diseases. The antibodies are usually IgG but can be IgM as well.
The presence of immune complexes themselves doesn’t always mean that there is a hypersensitivity reaction. Immune complex formation is an important mechanism the immune system can use to clump antigens together in order to have them easier removed or phagocytosed. Large immune complexes are easily removed by the spleen and the liver, meaning that the medium or small sized immune complexes are the most pathogenic. Hypersensitivity reactions occur when smaller immune complexes are produced in so large amounts that the body can’t get rid of them, causing them to deposit. If they are formed in the circulation will inflammation be systemic, but if they form in organs will the inflammation be local.
The most frequent sites of deposition are kidneys, joints and small blood vessels, which is why common symptoms of type III hypersensitivity reactions are glomerulonephritis, arthritis and vasculitis. Deposited immune complexes activate the complement system and neutrophils. The complement system causes inflammation with resulting tissue damage, recruitment of neutrophils and monocytes and increased vascular permeability. Neutrophils release lysosomal enzymes and reactive oxygen species, which damage the tissues.
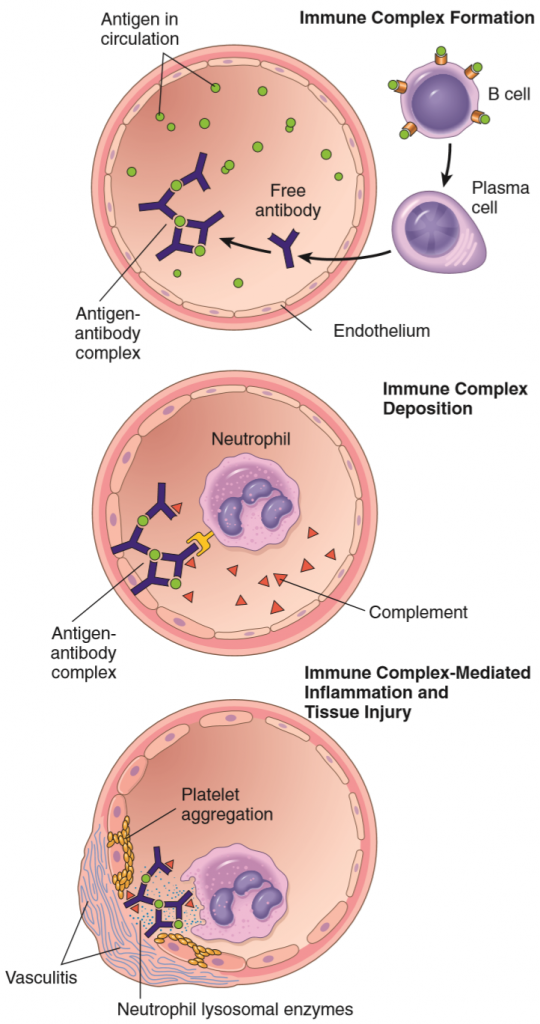
The histomorphology of injury in immune complex disease begins with necrotizing vasculitis. Plasma proteins (especially fibrin) deposit in the vessel wall, causing fibrinoid necrosis. The necrotized vessel is thrombogenic, so thrombosis occurs.
Systemic immune complex disease begins when immune complexes form in the circulation. These complexes eventually deposit in tissues, which causes an acute necrotizing vasculitis in these tissues. A prime example of this is serum sickness, which occurs when patients are administered serum from healthy people (these usually contains antibodies that are beneficial to the patients). After 5 days has the patient produced antibodies against the antigens in the foreign serum. Immune complexes form and deposit. Serum sickness doesn’t occur often nowadays, however the disease progression is similar in all systemic immune complex diseases.
Local immune complex disease means that symptoms occur only where the antigen was planted. A model of this is the Arthus reaction, where we inject an antigen under the skin of a previously immunized animal. At the site of injection will an inflammatory reaction develop, and after some hours will there be oedema, haemorrhage and possibly ulceration.
Here are some important immune complex diseases:
| Disease | Antigen involved | Clinicopathological manifestation |
| Arthus reaction | Foreign proteins | Cutaneous vasculitis |
| Polyarteritis nodosa | Sometimes hepatitis B virus proteins | Systemic vasculitis |
| Poststreptococcal glomerulonephritis | Proteins in streptococcus cell wall | Glomerulonephritis |
| Reactive arthritis | Bacterial antigens | Acute arthritis |
| Serum sickness | Various proteins | Arthritis, vasculitis, glomerulonephritis |
| Systemic lupus erythematosus | Nuclear antigens | Nephritis, skin lesions, arthritis, more |
Type IV hypersensitivity
The other types of hypersensitivity have been mediated by antibodies; however type IV is mediated by cells and not antibodies. It is therefore also known as T-cell mediated hypersensitivity.
Both CD4+ TH cells and CD8+ TC are involved in T-cell mediated hypersensitivity. Of the TH cells are the TH1 and TH17 subtypes most important, as they secrete pro-inflammatory cytokines that recruit and activate macrophages and other cells. TC cells are involved as they exert cytotoxicity, killing host cells and causing tissue damage.
TH cell mediated type IV hypersensitivities are often called delayed-type hypersensitivity, or DTH.
Delayed-type hypersensitivity begins when antigen-presenting cells first meet and phagocytose an antigen, either self-antigen or microbial antigen. The APCs then present this antigen to the TH cells. The APCs also produce cytokines, the types of which decide whether the TH cell will differentiate into TH1 or TH17 subtypes. The person is now sensitized, and nothing more happens, however the TH1 and TH17 cells will “remember the antigen” until the next time it appears.
Upon subsequent exposure to the antigen will the previously differentiated TH1 and TH17 be recruited to the site of the antigen and immediately secrete pro-inflammatory cytokines that recruit and activate neutrophils, macrophages and monocytes. Activated (M1) macrophages will continue to phagocytose antigens and continue to present them to T-cells and continue to produce cytokines which stimulate TH1 and TH17-cells, producing a positive feedback loop between activated macrophages and TH cells. However, note that so far has nothing pathogenic happened. This is part of the normal immune response against pathogens. Tissue injury (and therefore hypersensitivity) occurs when the pathogen can’t be eliminated. That is when the positive feedback loop becomes an inflammatory machine with no brakes.
In some DTH reactions will granulomas develop. Over a period of weeks will the TH cells in the tissues be replaced by activated macrophages. These macrophages accumulate and take on a special morphology where they become large, flat and eosinophilic. At this point they’re known as epithelioid cells (due to their resemblance to epithelial cells). Under the influence of IFN-γ, produced by TH1 cells, will epithelioid cells fuse with each other and form multinucleated giant cells. The microscopic accumulation of giant and epithelioid cells, surrounded by lymphocytes, is called a granuloma. Note that granulomatous inflammation doesn’t always require a DTH reaction, and not all DTH reactions results in granuloma formation.
Delayed-type hypersensitivity is delayed because it takes 12-48 hours for TH1 and TH17 cells to arrive at the site of the antigen and to start producing cytokines.
The classic example used to show the characteristic delay and symptoms of a DTH reaction is the tuberculin test. It is a test used to test patients whether they’ve been exposed to m. tuberculosis. Tuberculin is a mixture of proteins that are injected under the skin of the patient. If the patient has been exposed to m. tuberculosis will the patient already have tuberculosis-sensitized TH1 that will travel to the site of injection and cause inflammation. The resulting erythema and induration are a positive result, meaning that the patient has previously been exposed to m. tuberculosis.
The immune reaction caused by TC cells begins when TC cells falsely recognize self-antigens presented by host cells as foreign, which is when the TC cells differentiate into cytotoxic lymphocytes and begin to kill the healthy host cells. This killing is done by the TC cells releasing perforin and granzymes. The former will form holes in the target cell membrane while the latter induces apoptosis.
Here is a table of important cell-mediated hypersensitivity disorders:
| Disease | Antigen | Mechanism | Clinicopathological manifestation |
| Autoimmune myocarditis | Myosin heavy chain protein | CTL-mediated killing of myocardial cells | Cardiomyopathy |
| Contact sensitivity | Environmental chemicals (like poison ivy) | DTH-reaction | Epidermal rash and blisters, possibly necrosis |
| Hashimoto thyroiditis | Thyroglobulin and other thyroid proteins | Inflammation and CTL-mediated killing of thyroid epithelial cells | Hypothyroidism |
| Inflammatory bowel disease | Enteric bacteria? Self-antigens? We don’t know. | Inflammation mainly by TH17 | Chronic intestinal inflammation |
| Multiple sclerosis | Proteins in myelin | DTH-reaction, myelin destruction by macrophages | Demyelination. Paralysis. |
| Rheumatoid arthritis | Collagen? Citrullinated self-antigens? | Inflammation by TH17 | Arthritis, destruction of cartilage and bone |
| Tuberculosis | Mycobacterium tuberculosis antigens | DTH-reaction | Multiple |
| Type 1 diabetes mellitus | Antigens of β-cells | DTH-reaction, CTL mediated β-cell destruction | Insulitis, diabetes |
*I know type IV can be confusing, and different sources differ in their definition of what a delayed-type hypersensitivity really is. Some sources say that all type IV reactions are DTH, while some say that only a few of them are.
Upon subsequent exposure to the antigen will the previously differentiated TH1 and TH17 be recruited to the site of the antigen and immediately secrete pro-inflammatory antigens that recruit and activate neutrophils, macrophages and monocytes.
Should it say pro-inflammatory cytokines?
Thanks for the amazing work, one love
Definitely, yes. I’ll fix it. Thanks you!
Do you think serum sickness is what anti-vaccine people are afraid of? 🤔
I wish I knew what was going on in their minds dude