Table of Contents
Page created on September 16, 2018. Last updated on December 18, 2024 at 16:56
Necrosis (on the macroscopical level) can be divided into four types, coagulative type, liquefactive type, caseation type and adiponecrosis.
In the coagulative type of necrosis, the rough tissue structure is upheld and can be recognized. Four subtypes of coagulative necrosis exist, infarct, decubitus, pseudomembrane formation and gangrene.
Infarct
An infarct is an area of ischemic necrosis in an organ that is caused by occlusion (blockage) of the supplying artery or draining vein. There are two types of infarct, anaemic and haemorrhagic infarct.
Anaemic infarct
The name anaemic means “without blood”, showing how this type of infarct usually is not accompanied by bleeding. Four organs are at risk for anaemic infarct:
- The heart,
- The kidney,
- The spleen
- The liver
This is because these organs have a relatively simple circulation system: They have an artery that goes in, a capillary network inside the parenchyme, and a vein that drains it. They are also solid organs, unlike to the spongy lung and intestines for example. Myocardial infarction is the most common anaemic infarction.
The infarction happens when there is occlusion of the supplying arteries (usually) or draining veins (less frequently). This is most frequently due to the formation of a thrombus in the vessel, an embolus or due to vasculitis (rare).
Usually only a small artery inside the organ is blocked, meaning that a part of the organ dies and not the whole organ. Because these organs are solid, there is a limit to how easily blood can “flow” inside the organ. This makes so that there is little overlap between the blood supply of different arteries, meaning that a certain slice of the parenchyme is often supplied by only one artery. If this one artery is blocked, the parenchyme supplied by the artery will receive no blood and will therefore die.
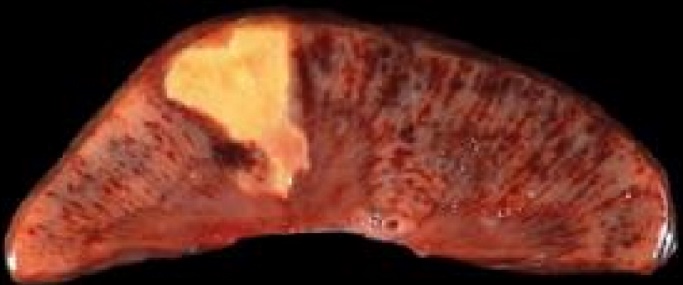
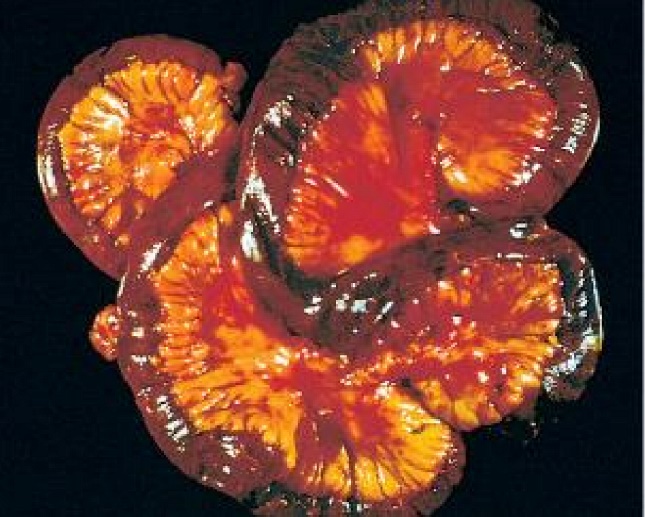
The infarcted area is often macroscopically greyish, dry and fragile, with a well-defined border, meaning there is a clear border between the dead and healthy tissue. The infarcted area is also commonly found near the surface of the organ, and often has a triangle or dome-like shape. The second and third macropreparations are good examples for what it looks like.
Haemorrhagic infarct

The haemorrhagic infarct is characteristic for the lung and gastrointestinal tract and can occur either when the artery or the vein is blocked. The word haemorrhagic means “bleeding”, which refers to how this type of infarct is accompanied by bleeding. Both the lung and the GI tract have dual circulations, as the lung has both the pulmonary and bronchial circulations and the GI tract has an anastomosis between the two mesenteric arteries. Occlusion of one of the circulations causes ischaemia and hypoxia, but the other circulation is still functioning, causing the haemorrhage. Haemorrhagic infarct in the lung is usually due to a pulmonary embolism.
Hemorrhagic infarction of the GI tract (often called intestinal gangrene) has a very high (up to 80%) mortality. Reasons for infarct can be occlusion of a mesenteric artery by thrombus or embolus, occlusion of portal vein, or mechanical causes like incarcerated hernia, volvulus, invagination or strangulation of the intestine. The mortality rate is so high because infarction causes perforation of the intestine, leaking the contents into the peritoneum, which will eventually cause sepsis. The treatment is emergency surgery to remove the necrotic segments.
Decubitus
Decubitus, also called pressure ulcer, occurs in cases where patients lie on their back in the same position over extended periods of time. This causes several parts of their bodies will be compressed by the weight of the rest of the body, including the sacrococcygeal area (most frequent), calcanei, scapulae and occiput regions. These regions will have their blood supplies compressed, which will eventually result in a type of ischemic necrosis.
Gangrene
Gangrene is the term for infarction of the extremities (although gangrene is also used to describe haemorrhagic infart of the GI tract). There are two types, dry and wet gangrene.
Dry gangrene occurs when the extremities (mainly the toes and feet) receive inadequate blood flow. This occurs mostly due to atherosclerosis (called peripheral artery disease) or uncontrolled diabetes mellitus, or a combination of both. The affected tissue becomes cold, loses its normal color, becoming darker and darker until it becomes completely black and falls off completely if not treated.
Wet gangrene occurs when there is a saprophytic superinfection on top of the dry gangrene, which causes the tissue to rot. Saprophytic pathogens are bacteria and fungi that thrive in dead tissue. The result is the formation of pus, often foul-smelling. Wet gangrene can also occur in the lung and the intestine.
Gas gangrene may be regarded as a third type, although it’s not a pathological entity on its own. Gas gangrene refers to the wet gangrene caused by the bacterium clostridium perfringens, which produces gas, resulting in the formation of bubbles in the soft tissue.
The treatment of gangrene is surgical, as the necrotic tissue must be removed. In cases of wet gangrene, antibiotic therapy is also necessary.
Pseudomembrane formation
Pseudomembrane formation may occur in two different places:
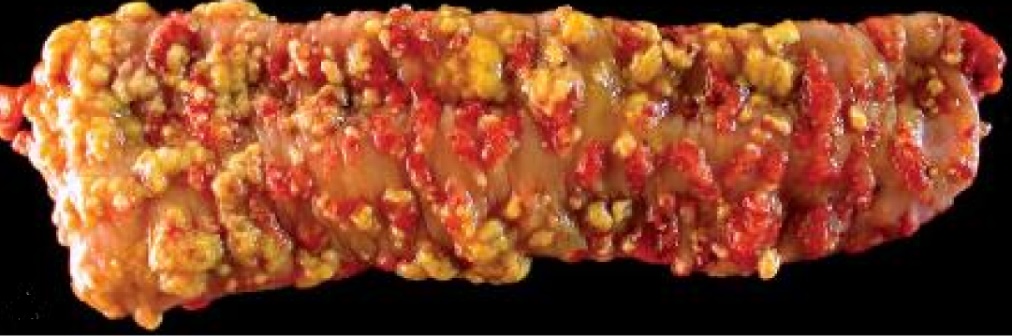
- in the colon due to clostridium difficile infection
- In the pharynx due to diphtheria infection
Clostridium difficile colitis occurs in patients treated with antibiotics for other infections. These antibiotics wipes out the healthy bacteria in the colon, allowing clostridium difficile to grow without competition. The bacterium produces two toxins, enterotoxin A and enterotoxin B, which cause necrosis of the tissues. This eventually causes formation of a kinda-membrane called pseudomembrane, which consists of leukocytes, fibrin and necrotic cell debris. The colonic crypts are distended by pus. The clinical features are pain, fever and diarrhea. The treatment is oral antibiotics which target clostridium difficile, like vancomycin.
why does liver get anemic infarcts ? doesnt it have a double blood supply? im confused.
Btw, thank you for all that you do!
It is actually extremely rare for that very reason. You can read more about it here. https://radiopaedia.org/articles/hepatic-infarction-1
You’re welcome 🙂
hello
whats the difference btw saprophytic and pyogenic pathogens?
which one would be occur in wet gangrena?
Saprophytic organisms eat an live on dead tissue. Pyogenic organisms form pus when they infect tissues. Saprophytic ones cause wet gangrene.