So I had my pathology 1 exam today. It’s the first day of the exam period and my examiner was Dr. László Kereskai.
The exam begins with you drawing a theoretical topic inside an envelope from a box full of envelopes. They’ll then give you a prep, and they give you a number for the slides. On the computer are the slides numbered (from 100-150 or something), and they give you one number. I’m pretty sure they decide what your prep and slide should be based on your topic. When it was my turn was I told to begin with the slide, then the prep and lastly the topic.
My topics were:
- Clinicopathological classification of acute inflammation with organ examples
- Prostatic hyperplasia slide
- Rectal carcinoma prep
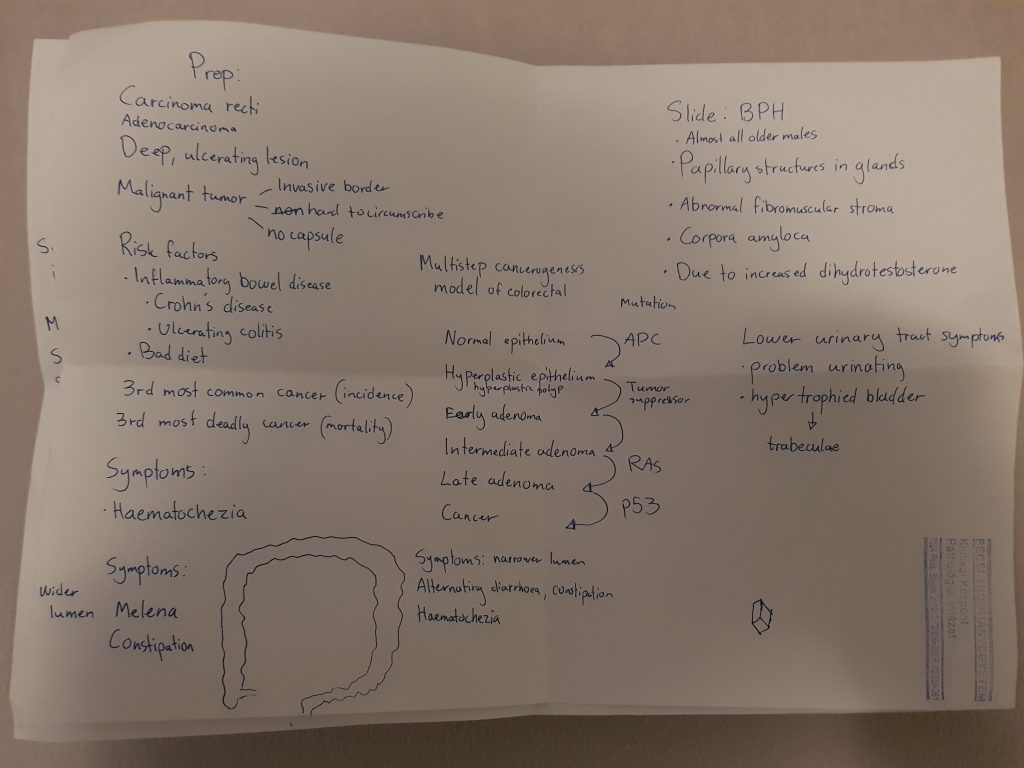
BPH slide
I began by saying that it’s HE stained, and that the urethral lumen and corpora amylacea show that this is the prostate. I then show the papillary structures and show the abnormal fibromuscular stroma (that I personally can’t see what’s normal about), and say that these are features of benign prostate hyperplasia.
I’ll try to include most of the conversation in bullet points. I’m N and he’s K
- K: Why is it called benign?
- N: To illustrate that it’s not a cancerous lesion.
- K: Yes. What types of syndromes can follow?
- N: Problems with urinating. Also, the bladder will be trabeculated because of hypertrophy.
- K: Yes. Do you think this patient was old or young? What was the age?
- N: Definitely old, perhaps 60-70.
- K: Perhaps even older. In the middle of a slide, there is a lobe. Do you know the name?
- N: I don’t.
- K: Okay, it’s called [Home lobe or something, I don’t remember]. Which zone of the prostate in hyperplastic?
- N: The central zone.
- K: Yes. How can you treat this if it causes symptoms?
- N: You can perform radical prostatectomy, wher-
- K: No no, we don’t do that for BPH, only for cancer. There’s something else.
- N: Oh, you can go into the urethra and scrape out the prostate.
- K: Yes, that’s right.
Rectal carcinoma prep
I begin by showing that there is a deep, ulcerating lesion, and the borders. He disagrees with the borders and say that only the top of the preparation shows unaffected mucosa.
- K: How would you describe the cancerous growth?
- N: It’s invasive and ulcerating?
- K: Yes, but what else
- N: It looks like many small polyps [This is more easily visible on the back of the preparation]
- K: Yes. What are the predisposing factors for this cancer?
- N: Inflammatory Bowel disease, like Crohn’s disease and Ulcerative colitis
- K: Yes, but they’re not the biggest.
I shouldn’t have begun by mentioning IBD, as they’re a very rare cause. I was just really eager to say Crohn’s disease.
- N: The biggest factor is the presence of polyps with dysplasia, adenomatous polyps. Not hyperplastic ones.
- K: Yes. How can you diagnose this?
- N: By endoscopy. Colonoscopy.
- K: Yes. We can use chemical methods as well but they’re not as good. It’s very uncomfortable so many people skimp on screening because of this, but it’s much better than cancer.
- N: I know it’s uncomfortable, I’ve performed it myself. It’s very uncomfortable.
- K: Yes, especially the day before.
We laugh
- K: What could the symptoms be?
- N: This is in the distal part of the colon, so we could see haematochezia, constipation and diarrhoea. If the cancer was in the ascending colon would the symptoms be different, mostly because the lumen there is wider.
- K: Yes, what about the lumen in this cancer?
- N: It will be smaller
- K: Yes, perhaps even completely blocked. Some endoscopies can’t get past the tumor because of this. Do you know the age of people that get this cancer?
- N: 20-30?
I still had Crohn’s disease in my mind, so I thought about the the age when people with Crohn’s usually get cancer.
- K: No not at all. Perhaps they’re born in 1920 and 1930. They’re very old
Great joke actually
- K: Do you know when we start to screen for colorectal cancer in Hungary?
- N: Around 50?
Pure guess
- K: Yes, around 55. What can the treatment be?
- N: Removal of the affected part or whole colon.
- K: Yes, if there’s no spreading.
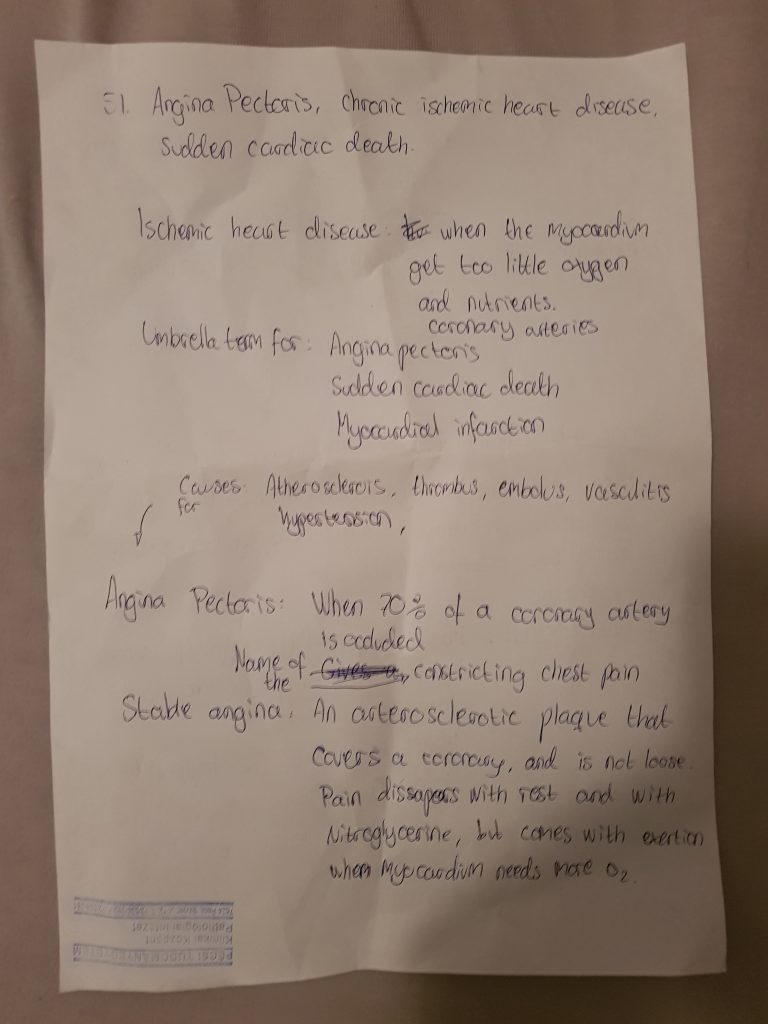
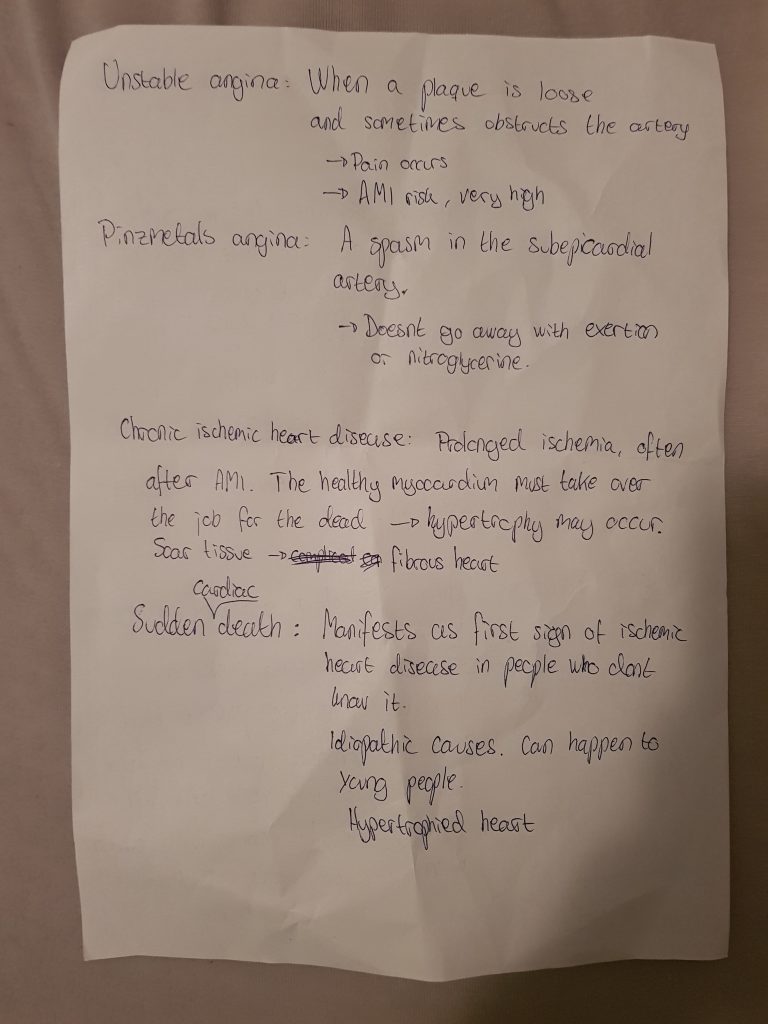
Acute inflammation
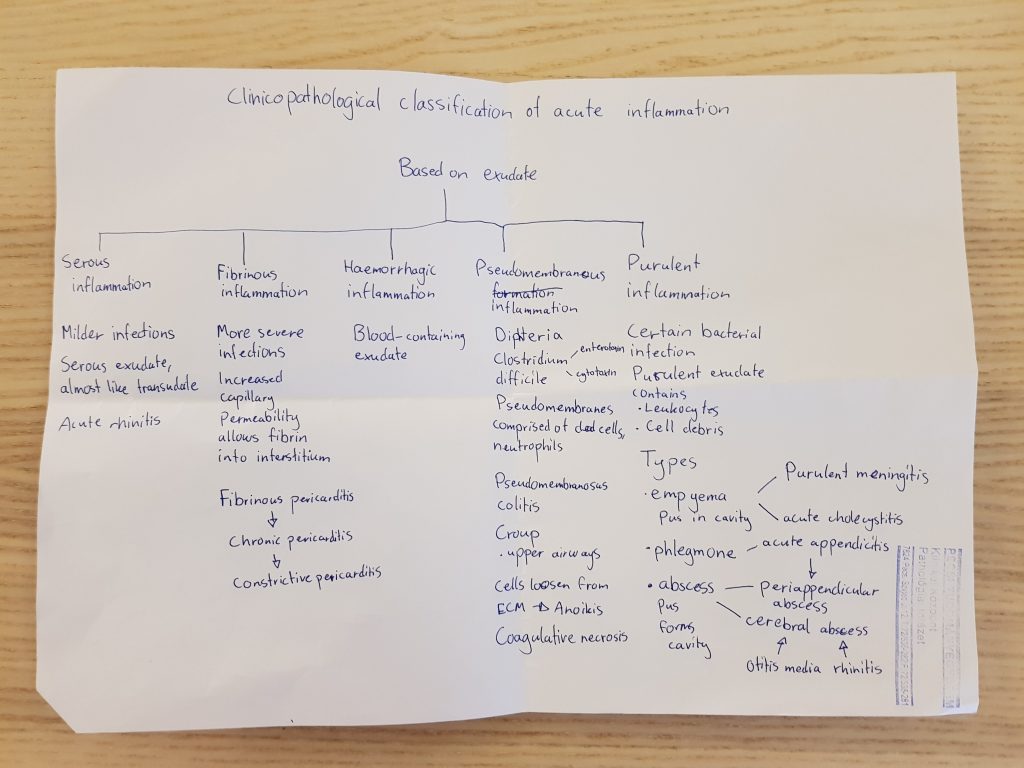
- K: Tell me about the types
- N: You have serous inflammation, where the exudate is almost like transudate, with low protein content.
- K: Can you name an organ example?
- N: Acute rhinitis?
I was very unsure about that answer
- K: Yes. There is a particular disease group that commonly affects serous membranes. Do you know which?
- N: No, I can’t recall.
- K: Autoimmune diseases. Now, what about fibrinous inflammation?
- N: It’s often due to more severe infections. The capillary permeability is increased enough that fibrin can enter the interstitial space.
- K: Can you name an example?
- N: Fibrinous pericardits
- K: What’s the most important cause of that?
- N: Acute myocardial infarction
- K: Yes, definitely. Can you mention another cause?
- N: Bacterial infection?
- K: No, no. There’s something else.
- N: I don’t recall anything.
- K: There was a story written on the fibrinous pericarditis preparation. It was taken from a woman with kidney failure, which ca-
- N: Oh, uraemia!
- K: Yes, uraemia is the other big cause of fibrinous pericarditis. Indeed is infection not a normal cause for that.
- K: What about haemorrhagic inflammation?
- N: Here will the exudate contain blood as well.
- K: Can you name any examples?
I was hoping he wouldn’t ask that
- N: Pneumonias?
- K: Yes, what types?
- N: Bacterial?
- K: No, no. Rather viral. There is a special organ that is characteristic for haemorrhagic inflammation. Which?
- N: I don’t know.
- K: The bladder, actually. Okay, what about pseudomembranous inflammation?
- N: It’s due to diphteriae or clostridium difficile, and commonly occurs in colon and upper airways.
- K: Yes, diphteriae in the upper aiways and clostridium in the colon. What is the cause of pseudomembranous colitis?
- N: Antibiotic treatment
- K: Yes. What do you think is the treatment for it?
- N: Other antibiotics that are specific for clostridium?
Qualified guessing by me
- K: Yes. It’s caused by antibiotics but we treat it with antibiotics. We use [some types I don’t remember]. What about purulent inflammation?
- N: We have three types, empyema, phlegmone and abscess.
- K: Can you name an example for empyema?
- N: Yes, like purulent meningitis.
- K: Yes, and for phlegmone?
- N: It can occur in soft tissue, or walls of organs like in acute appendicitis.
- K: What can acute appendicitis lead to?
- N: A periappendicular abscess.
- K: Yes, but that’s not the most common. Something else can happen
- N: I can’t remember
- K: It can become gangrenous inflammation.
That’s the end of what I remember. I obviously used a lot of time to think when he asked questions, and sometimes he had to help me find the answer. The whole thing took about 15 minutes I’d say.
I was really lucky with my topics. Also, I sat next to the cabinet with the preparations, so when I needed some organ examples for acute inflammations I just turned around and checked some preps 😂
Dr. Kereskai asked all of us many clinical questions, like what are the symptoms, what are the risk factors, how can you diagnose it, how can you treat it etc. I was told that he really likes immunology but he didn’t talk to me about that at all. He didn’t ask about definitions, not for hyperplasia or inflammation, or the signs of inflammation or anything like that.
All in all, he was really nice, and so was the other examiner in the room (for the most part). Everyone in the room passed, despite some not knowing certain things and answering wrong to some questions. We all did.
I got 4, 4 and 4/5 on my topics (don’t remember which one was 4/5, I believe it was the prep). The end grade was 4.
I’d encourage everyone to never begin with the diagnosis on the slide and prep. Instead, start with the staining, show some healthy tissue (if present), say the organ, show the abnormalities, and then come with the diagnosis. Also, they were really nice. I’m certain that anyone who has studied pathology 1 well can pass it without too much problem.
My next exam is pathophysiology 1 next Wednesday (unless I can get a spot on next Friday. Hit be up if you don’t want your spot next Friday).
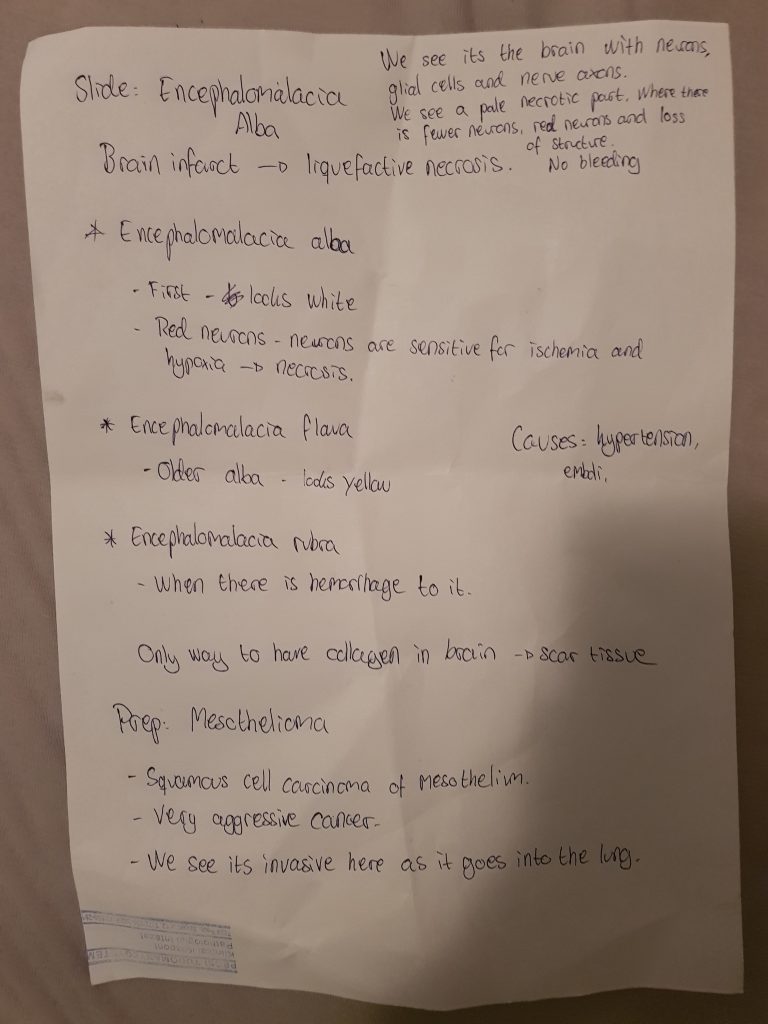
Edit: Here are the exam notes of my girlfriend, who got a 5
I got the same topic. when I compare your answers to examiner’s question to mine, and at the same time comparing your grade and the one that is offered to me ;I conclude that …………☹️☹️😡🤬.
Maybe it is better to be ……. Than studious !!!!!!
(many other words censored ………)
You don’t need to censor words, this is not a family-friendly website 🙂
I wholeheartedly feel your anger.
You are my hero!! Thanks for sharing all your notes 🤩
Thank you so much for your kind words! <3 😄😄
Congratulations!!
when will you take PathoPhys
and can you tell us how it goes
PLÉÁSÉ!
Hello! I had it on Friday and I just published my experience.
And thank you!
Congrats on the pathophys!
And thank you for making this site, it really is super helpfull. Easy explanations of the topics, and excellent(5) preps and slides.
10/10
Thank you so much for your kind words! ❤
I’m glad I can help.
Treatment of clostridium difficile is metronidazole or vancomycin!
Congratulations ! And thank you for sharing
Good luck for all other exams ❤️
Thank you <3 ! You too (if you have exams, that is)