The exam was last Friday, the 21st of December. My examiner was Dr. András Garami, and there was also a PhD student present as a co-examiner. The co-examiner just observed except for once, when the main examiner told the co-examiner to ask the student one question.
My topics were:
- Hypertension and the adrenal gland
- Pathophysiology of glomerular filtration
- Active heterotopic abnormalities (premature beats)
And the ECG of course. When you enter the room will you draw a green card, and on that card are your three topics. They didn’t give me the ECG until after I’ve been preparing my topics for at least 10 minutes. The examiner preferred to begin with the ECG so that’s what I did.
ECG
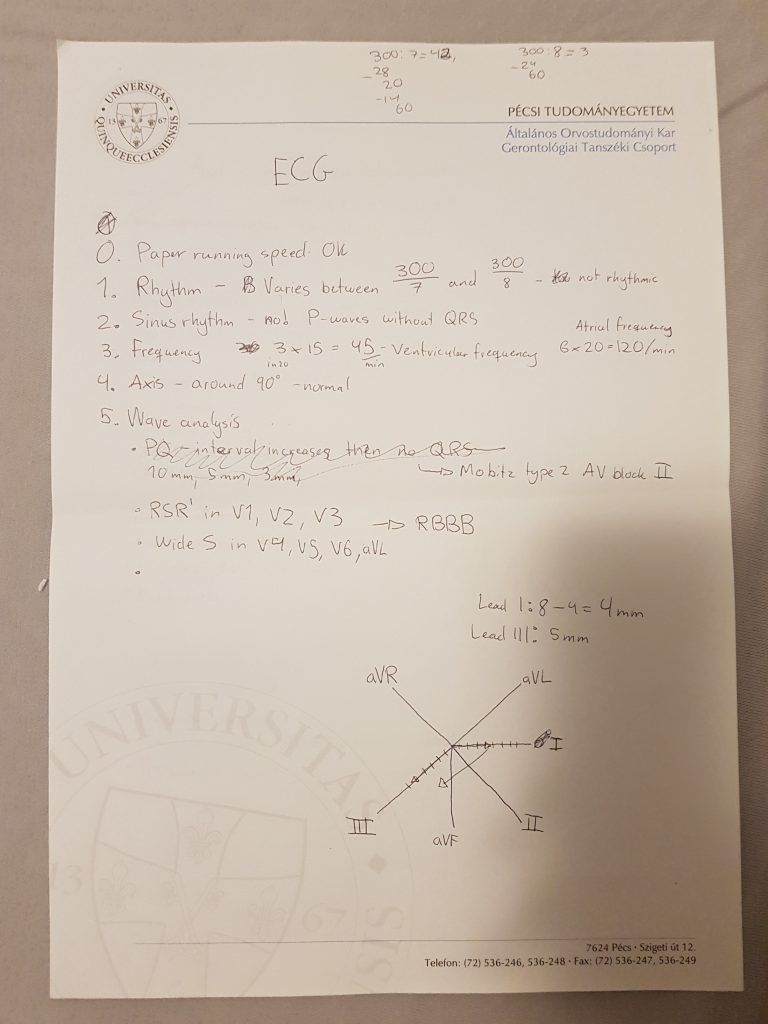
My seminar teacher told us to use that step-by-step approach on the ECG, and the examiner really liked it. I encourage you to do the same.
I determined that there was an RBBB and a type II AV block with Mobitz type II. However when I presented it to him did he show me that at some places was the PQ interval very small, meaning that it couldn’t have been a type II AV block. When he pointed that out did I immediately correct it by saying that it’s more probably a type III AV block with a ventricular escape rhythm. He told me that it’s not a ventricular escape rhythm. I realized my mistake again and said “No, this is not a ventricular rhythm because the QRS complexes are normal. It must therefore be a junctional escape rhythm.” He agreed, and asked me what could be done to fix this. After some back-and-forth did I arrive at the conclusion that a pacemaker was the right answer. We moved on to the theoretical topics.
Hypertension and the adrenal gland
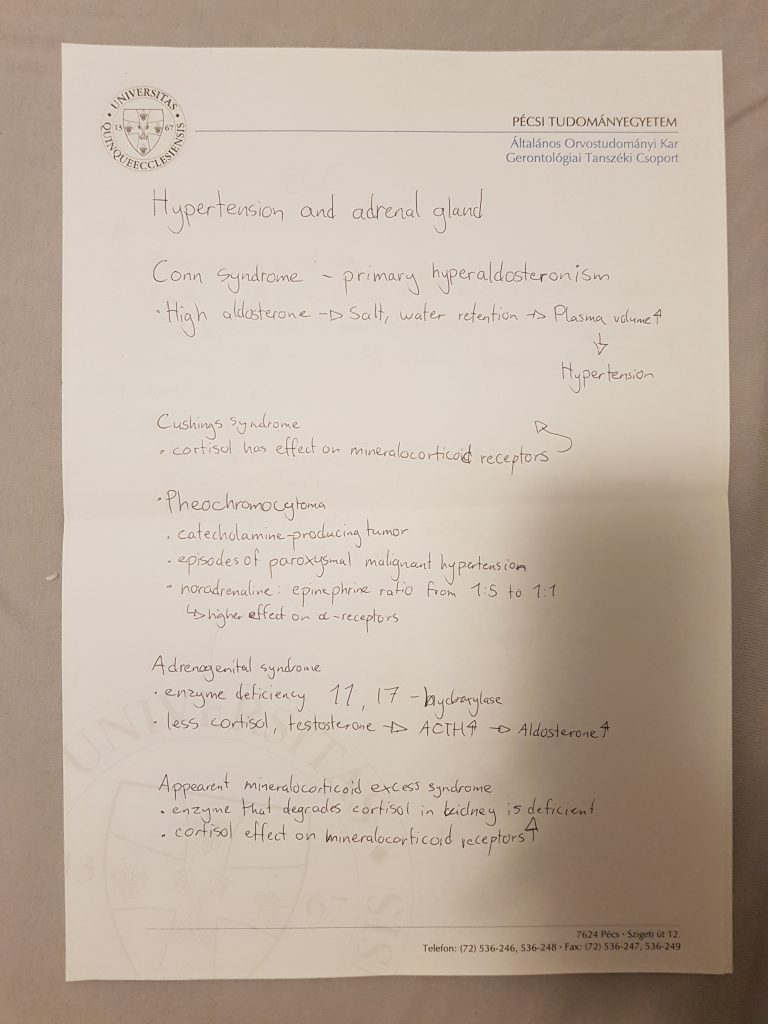
I began with this because it’s my strongest theoretical topic of the ones I drew. I basically just explained to him what I’d already written. He then asked some questions. It went something like this:
- Garami: How is the blood pressure in Cushings in comparison to Conn syndrome?
- Nikolas: It should be lower, because cortisol has a weaker effect on mineralocorticoid receptors than aldosterone.
- G: That’s what you would think, but in real life it’s actually higher than in Conn syndrome.
- N: Really? I’m not sure.. [I spent some time thinking] Oh, is it because cortisol increases the sensitivity to catecholamines?
- G: Exactly. Now, how can we diagnose a pheochromocytoma?
- N: We can measure catecholamines breakdown products in the urine.
- G: Yes, how would you do that?
- N: Like, with a urine sample?
- G: Yes, but what else?
- [I didn’t really understand what he meant, but I think he wanted me to say that we should measure urine in a 24 hour period. I don’t really remember.]
- G: Okay, how does aldosterone increase the blood pressure?
- N: Well, you have increased salt and water retention that will cause the plasma volume to increase.
- G: Yes, but what happens to this volume?
- N: It stays in the plasma? I guess it could go into the interstitium if there was low oncotic pressure or the capillary hydrostatic pressure was increased for some reason.
- G: No, that’s not what I mean. There is no oedema. Will the vessels just continue to fill up with fluid? Wouldn’t they burst?
- N: Maybe the aldosterone receptors are desensitized after a while?
- G: No, that’s not what happens. Something “counteracts” the aldosterone.
- N: Oh, like the natriuretic peptides? Atrial natriuretic peptide and brain natriuruetic peptide?
- G: Yes. Why are they produced?
- N: Because of increased stretch of the atria and pressure receptors in the CNS?
- G: Yes. In fact, due to the increased plasma volume will organs vasoconstrict so that they aren’t overperfused. This means that the excess fluid doesn’t really reach the organs, but instead stays in the arterial system. Do you know what the mechanism where aldosterone is counteracted by natriuretic peptides is called?
- N: Aldosterone escape mechanism? [This was a half-guess. I’ve heard about aldosterone escape before, but I didn’t know that it’s this.]
- G: Yes! Great.
Pathophysiology of glomerular filtration
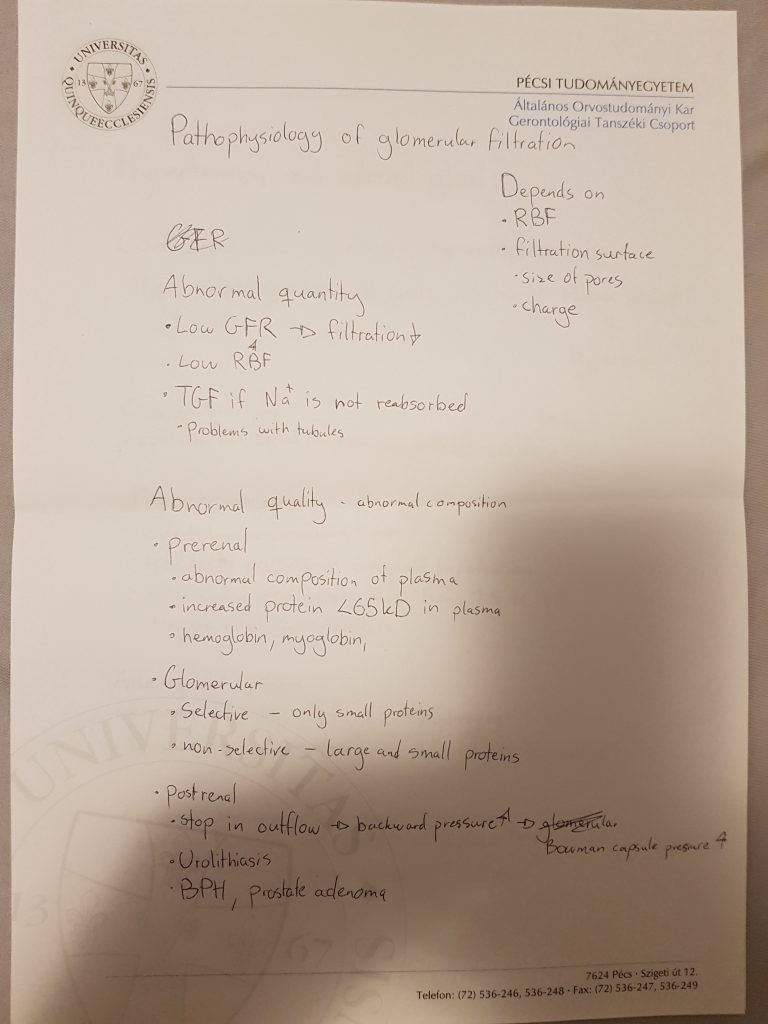
I don’t really remember what we talked about here. I explained what I’d written down, and he pointed out that I forgot to write that GFR also depends on the filtration pressure. He asked me to name an example for how TGF can cause problems for filtration (I think I said osmotic diuresis).
He disagreed that kidney stone, BPH or prostate adenoma would cause postrenal problems with filtration, as they would actually cause postrenal acute renal failure instead. He mentioned some better examples but I can’t remember which.
Active heterotopic abnormalities (premature beats)
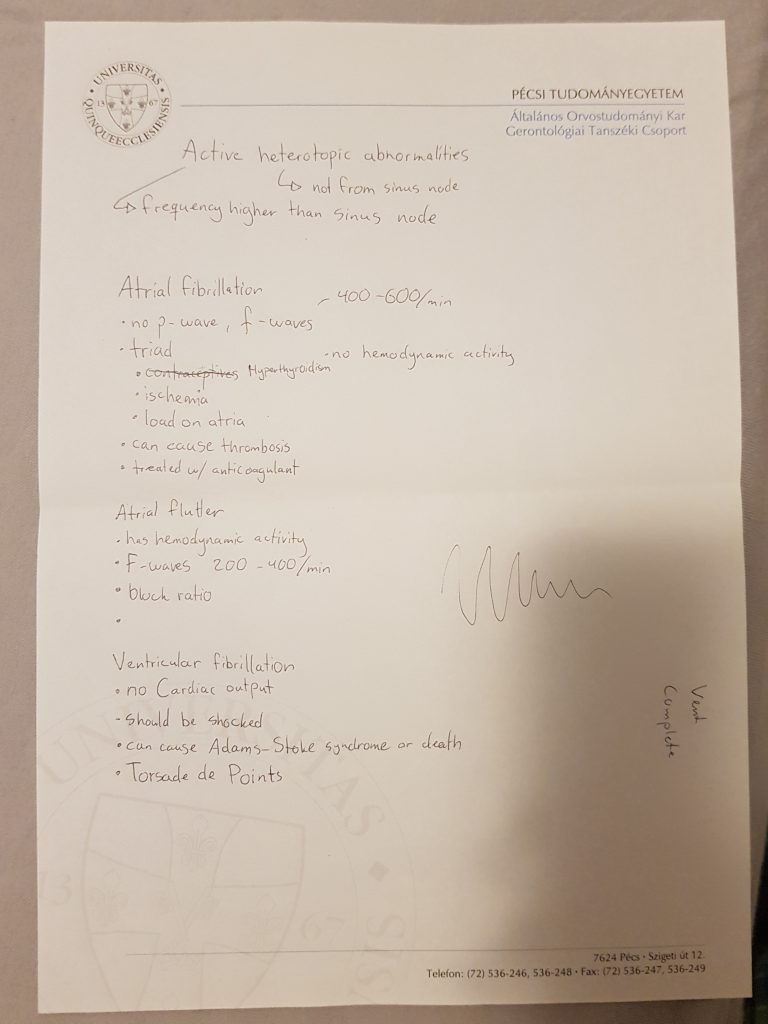
Now, you might already notice that what I wrote was about a completely different topic. I’m really bad at the ECG topics (you might know that since I didn’t write about them), so when I drew that topic I became slightly panicked. I’ve looked through them the day before (Idun notes), and my girlfriend told me what active heterotopic means. However, I couldn’t come up with any examples, so I just wrote about fibrillation and flutter, because I thought that maybe they were a part of the topic (they technically are, but they have their own topic).
He instantly saw what I’d written and was very confused. He said “what’s this?” and that’s when I realized I’d fucked up completely. I tried to save it.
- N: Oh, maybe I should’ve written about extrasystoles and escape rhythms as well?
- G: Extrasystoles and tachycardias yes, but escape rhythms no. It even says “premature beats” in the topic name.
He asked me about types and classification of tachycardias (supraventricular and ventricular) and their compensatory pauses. He also asked me what Torsade de Points is, which is when I drew the spindle-like ECG you can see on my notes.
- G: If you can explain to me why the compensatory pause is different in ventricular and supraventricular tachycardias will I give you a 5.
I couldn’t. I didn’t even know they had different compensatory pauses. He tried really hard to make me “recall” why it was, but I’ve never learnt it so I couldn’t recall it. He eventually understood that I didn’t know the answer and gave up.
- G: I’ll give you the 5 anyway, as encouragement.
All in all was the experience very good, mostly the same as for patho. He was extremely nice and passed everyone, even those who failed to answer certain basic questions either because they didn’t know or they couldn’t recall the answer. Just be aware that they’ll always find ways to ask questions you are not prepared for. My notes (and the book and lectures) don’t cover absolutely everything, so you can’t be prepared for every possible question, but it’s still possible to get a 5.
Do you know about anyone who got a 2, or approximately how sucky I can be and still get a 2? Exam soon, and really struggling over here.
Hey!
Don’t worry. You can suck pretty hard and still pass. Trust me.
The examiner said that they expect more on the final exam. But as long as you show them that you’ve studied even a little bit this semester should you pass.