So I had pathophysiology 2 today. I had Professor Garai as my examiner. My topics were “Forms, general pathophysiology and consequences of anemia”, “Portal hypertension” and “Mechanisms and disturbances of bone remodeling. Osteoporosis, osteomalacia. “
Case
I began by presenting the case and my thoughts and explanations for each diagnosis, like this:
My case was a 64-year old female with established congestive heart failure. She had anasarca, shortness of breath on exertion and enlarged heart and spleen, polyuria at night and tachycardia in rest and during exercise. She also has arthritis and takes NSAIDs for the pain.
She recently experienced worsening of the heart failure symptoms. She also has occational gastric pain and decreased appetite. The blood parameters showed anaemia.
The case was that she had developed a gastric ulcer due to NSAID use, which had cause a chronic bleeding with resulting iron deficiency anaemia. This anaemia increased the demand for cardiac output, which worsened the heart failure.
His questions regarding the case were:
- How would you treat this case?
- Check and treat for H. pylori, give iron supplements, try to reduce the dose of the NSAID or switch to an NSAID that is less selective towards the isoform of COX which is present in the stomach (COX1) and more selective towards COX 2, which mediates inflammation
- Which other drugs can you give for gastric ulcer?
- Proton pump inhibitors, histamine antagonists, antacids
- Why did anaemia cause worsening of the heart failure?
- Anaemia increases the peripheral tissues’ demand for cardiac output, which the heart cannot provide when failing
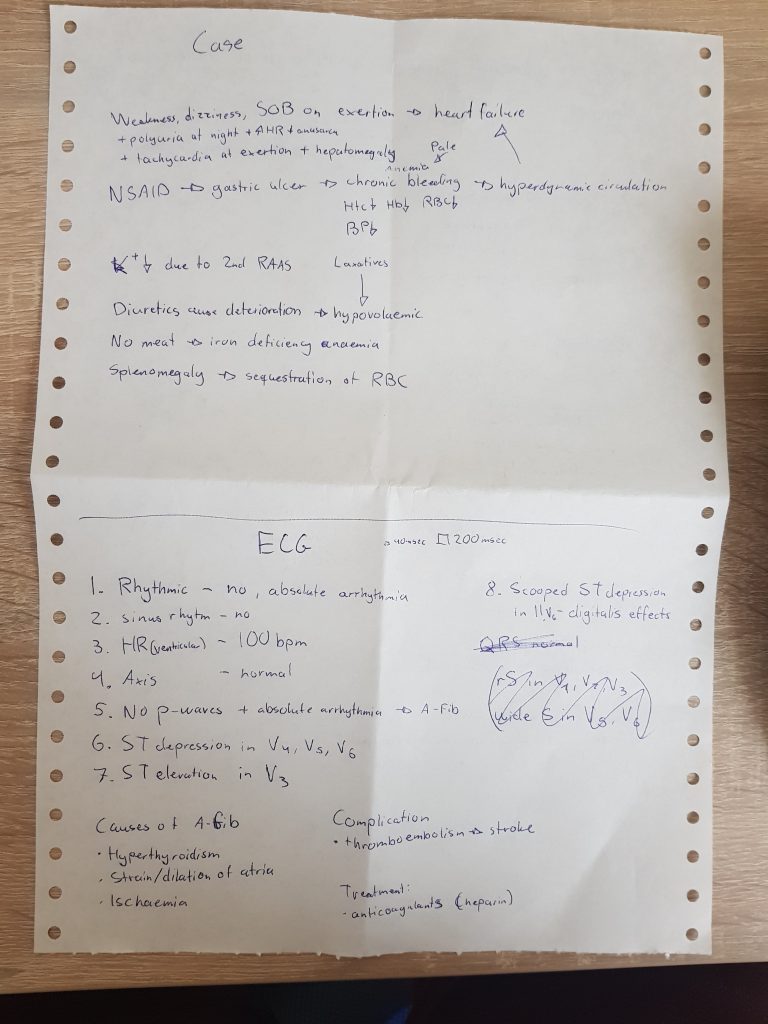
ECG
I went through the ECG stepwise (like everyone should). There were no P-waves and there was absolute arrhytmia, indicating atrial fibrillation.
His questions were:
- What is the most common cause of atrial fibrillation?
- Hypoxia of the atria.
- Which is caused by what?
- Strain or increased load on the atria.
- Which is caused by what?
- Backward congestion of left or right-sided heart failure.
He also asked about some other findings of the ECG that I had mistakenly interpreted for scooped ST depression or deep S waves (which he absolutely didn’t like). They were instead descending ST depression in V4 – V6 and high voltage, indicating left ventricular hypertrophy.
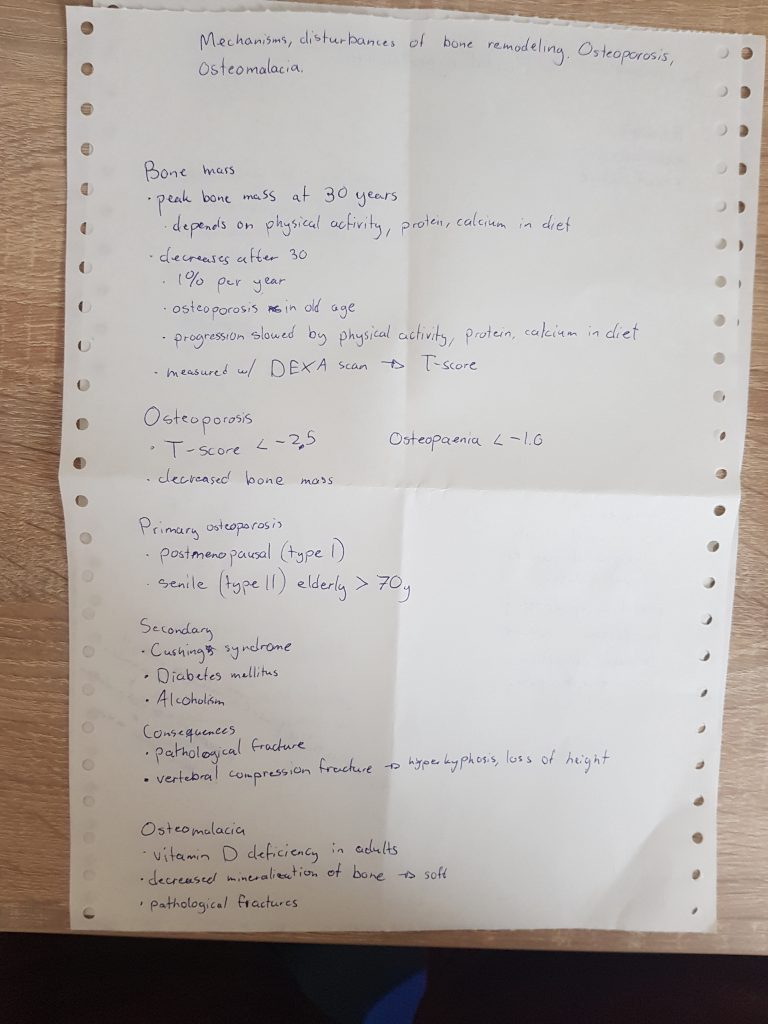
Mechanisms and disturbances of bone remodeling. Osteoporosis, osteomalacia.
I explained everything I had written down. His questions were:
- What is the third primary type of osteoporosis?
- Juvenile osteoporosis
- What else must you have in your diet to prevent bone mass loss?
- Vitamin D
- What other secondary causes of osteoporosis are important?
- Chronic renal failure, hyperthyroidism, iatrogenic Cushing syndrome (I wrote down Cushing syndrome but I had said Cushing disease instead), hypoparathyroidism
He was particularly not happy with how I had just written down three causes for secondary osteoporosis when the list should be 50 diseases long.
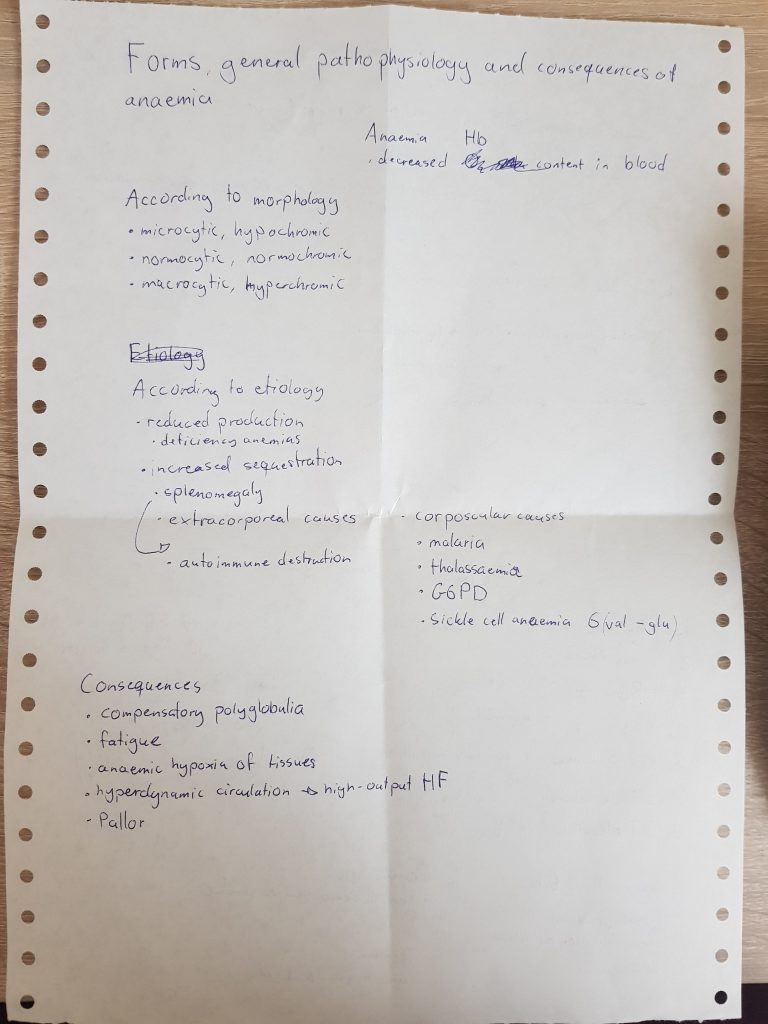
Forms, general pathophysiology and consequences of anemia
I explained the different ways you can classify anaemias (according to etiology, morphology). His questions:
- Which type of anaemia are you missing?
- Aplastic anaemia
- Also “anaemia of complex etiology”, but I didn’t know that
- What is aplastic anaemia caused by?
- Tumor infiltration of the bone marrow, radiation, osteopetrosis
He also asked me some causes of the different types.
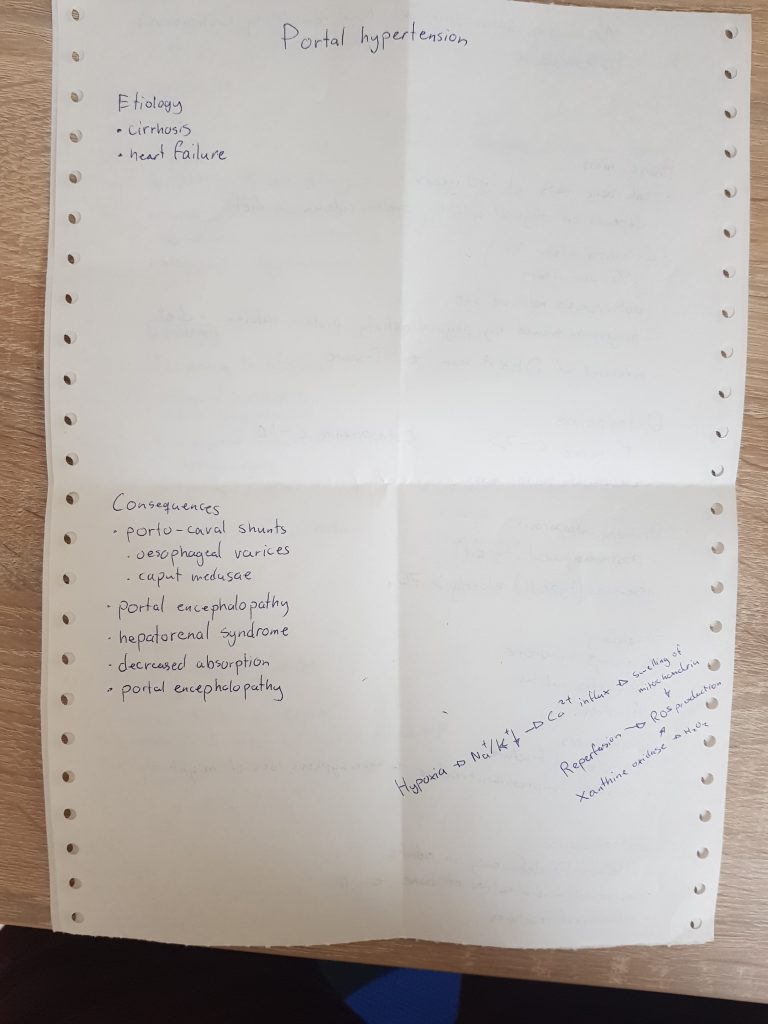
Portal hypertension
I didn’t write down a lot here as I didn’t remember a lot at the top of my head. His questions:
- What is the mechanism of portal encephalopathy?
- Blood from the intestines containing ammonia, short chain fatty acids etc are shunted directly to the systemic circulation instead of through the liver
- Where is the ammonia produced?
- By enteric bacteria
- Where else?
- (The answer was the kidney but I didn’t know that)
- How is ammonia toxic to the brain?
- It increases the permeability of the blood brain barrier and it inhibits the TCA cycle
- Which shunts do you have other than in the oesophagus and caput medusae?
- I said in the rectum, but apperarently there are three more shunts that I didn’t know of
He also asked some questions about hepatorenal syndrome but I can’t remember what.
Closing thoughts
I got a 5 in the end, which I’m really proud of. He was really nice and patient, both with me and with the people before me. The assistant was nice and helped out too. If there’s something he wants you to say he will do everything to make you say it (which can take some time). Just don’t get discouraged if he says “Jesus christ” if you say something stupid.
He didn’t ask me many questions and my exam was over relatively quickly, but he did spend a lot of time with those before me. To be honest he didn’t ask me very difficult questions either, at least not compared to those he asked those before me. I couldn’t answer all his questions and many times he had to help me find the correct answer. I said some very wrong things about the ECG and the topics but he didn’t care too much as long as you correct them.
If you’re worried about pathophysiology, I understand, but believe me when I say that they’re very nice. They will most likely pass you if they see that you have studied, even though you don’t know all the mechanisms or details. If you’re really worried, consider being a witness to someone else’s exam so you can see for yourself how chill it is and how nice they are.
Congrats man!!
Thank you <3
Congratulations 🌹❤️
Thank you <3