So I had obgyn 1 yesterday. The day before me and the other 14 students who had the exam were added to a new team on teams. There, the secretary Dora Szigeti wrote a message that at 8:00, we would receive our topics, and when it was our turn, the examiner would call us. Another student asked her who our examiner would be, and she answered “Dr. Bálint Farkas”.
At 8:00 the next day, we all joined the meeting. There, the secretary gave us some more information, about how all students will at least get 30 minutes preparation time. She then drew one A topic and one B topic for each of us, in alphabetical order by last name. I was the eighth student to draw topics, so I knew I would be the eighth student to have the exam as well.
My topics were: A7 – Prolapse of the foetal cord and limb, and B3 – Placenta accreta, increta, percreta.
She told us that while we prepare we must leave our cameras on but microphones off, and we could leave the room and eat and drink as we wanted, no need to ask for permission.
Because I knew the alphatical order, I could tell when my turn was coming up, which was nice. I was the eighth student, so my exam began at 10:40 when Dr. Bálint Farkas called me. He began asking for ID, and then left me to explaining my topics. I began with my A topic.
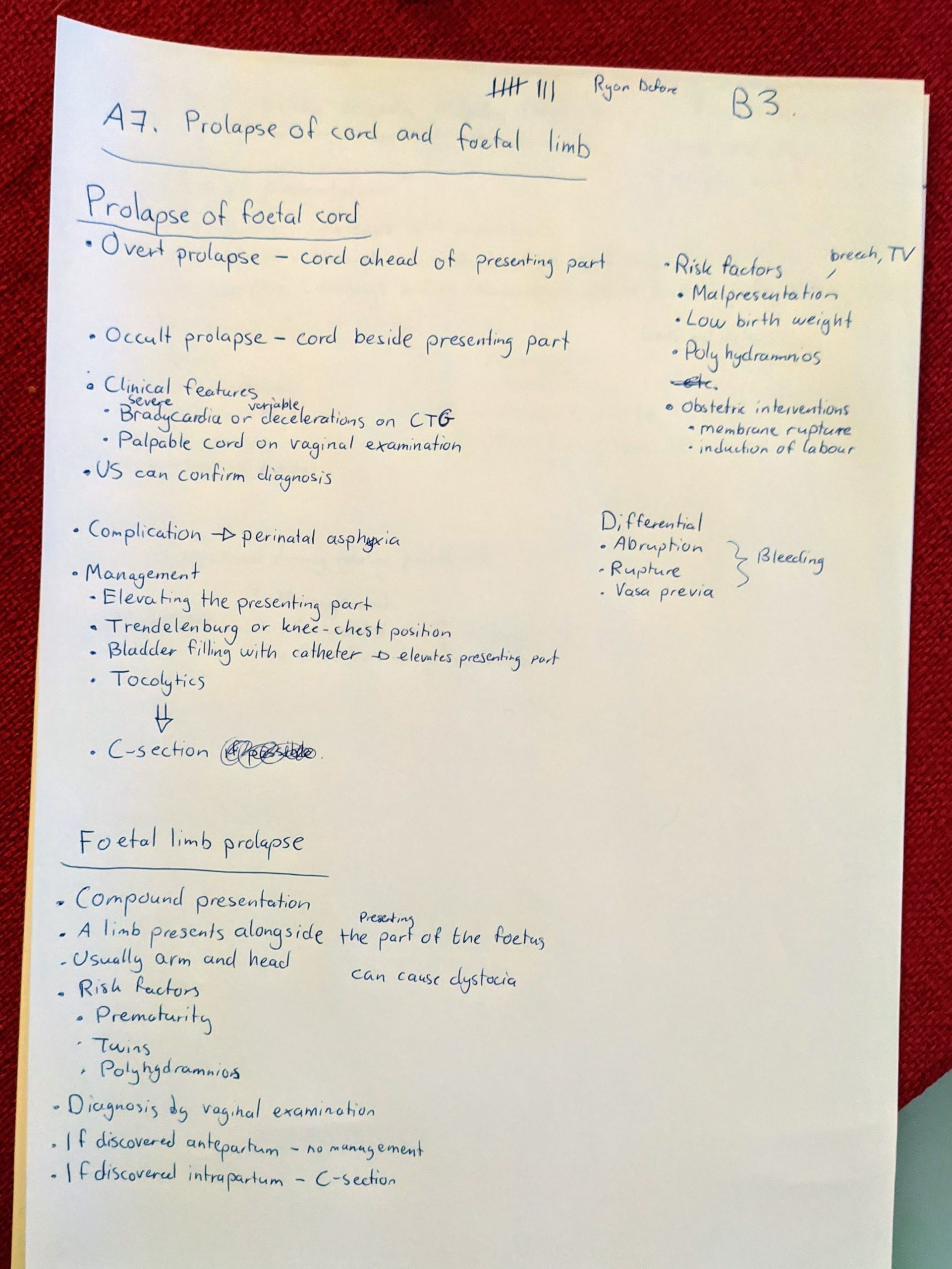
I began by telling him everything I’d written about umbilical cord prolapse (except the differentials). After I’d mentioned perinatal asphyxia, right before I was going to mention the management, he asks “What would you do about it if you diagnosed this on the labour ward. What would be the management?”. I continued with what I’ve written about management. He said “OK”, so I continued on with what I’d written about foetal limb prolapse. He said “OK, next topic”. So there were no questions to this. I continued on with my B topic.
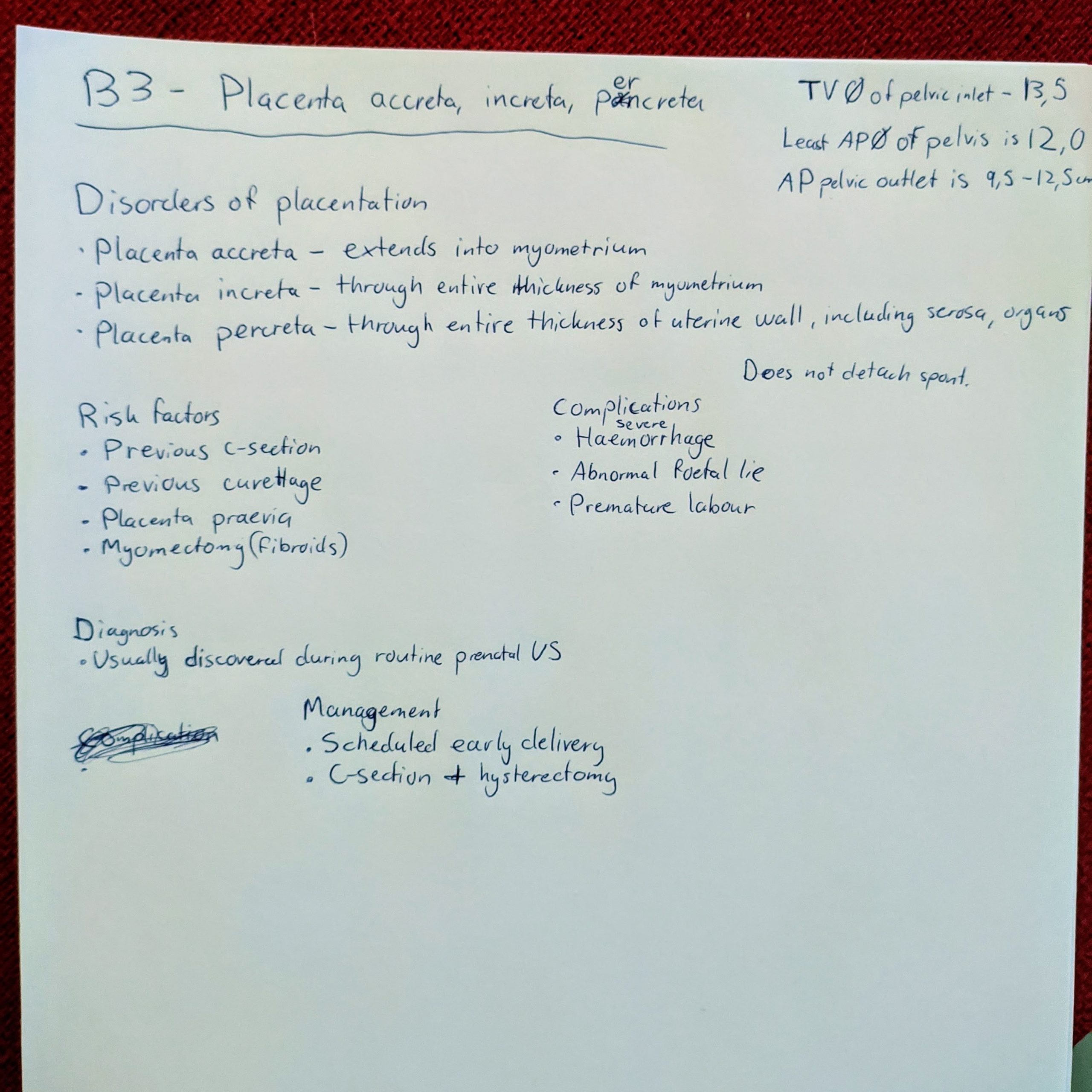
I tell him everything I’d written. He had no questions to this topic either, but began asking me general questions, where my performance wasn’t exactly excellent.
- Examiner: Can you tell me other causes of postpartum bleeding?
- Me: Uterine atony, is the most important cause.
- *I couldn’t recall any other causes*
- E: What does “cotyledon retention” mean?
- M: It means that one or more cotyledons have been retained in the placenta (I meant to say uterus), so that not all of the placenta has been expulsed in the third stage
- E: What is uterine inversion?
- M: It is when the uterus sort of prolapses out of the cervix
- E: Can you tell me a reason for that?
- M: I don’t know a reason for that.
- E: It can be artificial if you pull the cord without the placenta detached, so it brings the uterus with it, or if the cord is too short, so it pulls the uterus with it. It’s very painful and causes very heavy bleeding.
- E: What is the so-called Crede manouevre?
- *He actually sent me the word “crede” on message because I couldn’t understand the word*
- M: Is it the one where they return the inversed uterus?
- E: No.
- M: Then I don’t know.
- E: It’s a maneouvre to fascilitate the detachement of the placenta through the abdominal wall. You squeeze it out like a plum.
- M: Okay.
- E: Do you know what the Ritgen maneouvre is?
- *Once again he sent me the word “Ritgen” on message*
- M: No, I don’t recognize that name either
- E: So you’re not really a maneouvre guy, are you?
- *We laugh*
- E: Okay. It’s when you grab a sterile towel and hold the perineum when the head is deflexed to protect the perineum.
- M: Okay, I had heard of that, I just didn’t know the name.
- E: What is an episiotomy by the way?
- M: It is when you cut the perineum to increase the opening of the birth canal, either midline or slightly oblique.
- E: Yeah. How many stages of layer do you know?
- M: Four.
- E: How many movements does the foetal head do during normal labour?
- M: So it begins with descent, …
- E: No
- M: Engagement, descent, and flexion at the same time?
- E: Flexion, okay.
- M: Yeah flexion, and then internal rotation, and then the head extends out of the birth canal, and then the external rotation back, and then the anterior shoulder and then the posterior shoulder.
- E: Yeah, okay. What is shoulder dystocia?
- M: It is what occurs if the shoulder has not been born, so to say, in the same contraction or the contraction after the contraction where the head was born. So it’s a form of mechanically obstructed labour.
- E: What can you do about it?
- M: Operative delivery, so foreceps or vacuum
- E: No, the head is already out.
- M: Oh no, yeah of course. You do the, uhm.. I don’t remember the name of this maneouvre either, but you pull the legs of the mother, and put pressure on the pelvis somewhere, to try to help the shoulder out.
- E: So where would you put the pressure on the pelvis?
- M: On the symphysis
- *I was only half-sure that symphysis was the right answer, which is why I didn’t specifiy where to put pressure initially
- E: On the symphysis, yeah? To remove the stuck shoulder. The manouevre is called McRoberts. What if that doesn’t work?
- M: I remember there’s a list of possible managements. I don’t think.. You can also cut the clavicle or the symphysis of the mother, but I don’t think that’s the next stage..
- E: Those are drastic movements …
- M: Yeah, there is another movement you would rather do before that.
- E: Cutting the symphysis of the mother, wow. Cutting the whole urethra and bladder and everything. That’s a bloodbath, man.
- M: Yeah..
- E: I mean, one of my collegues who retired like 20 years ago told me about how they used to do that in the 1970s, but I haven’t seen it before.
- M: I’m glad. I just remember that it was mentioned on the lecture. Uhm.. I’m drawing a blank. I remember there’s a different maneouvre but as we established I’m not good on manouvres.
- *We laugh*
- E: Yeah. I’ll give you a 4, okay?
- M: Yeah, I’m happy with a 4.
- E: It wasn’t bad, but it wasn’t excellent, yeah?
Completely deserved, although it’s annoying that they mention procedures on the lecture which apparently haven’t been used for 50 years.
My whole exam lasted 10 minutes. I spent almost exactly 5 minutes with my topics, and the remaining 5 minutes were used to uncover how little I knew about manouvres.
Either way it was a pleasant experience. He can sometimes seem a little intimidating but I was much less nervous during the exam than I was while waiting for it.
My last exam is paeds 1, on Friday. Looking forward to being done!
Congratulations! Can u share ur paed 1 exp, too?
Thanks! I will. Tomorrow.
How many whole days did you need to study for this? Thanks for the exam experience!
I studied maybe 3 – 4 whole days, but I spent a couple of them going through the lectures, which after all I don’t think was worth it. I read through Hatem’s notes the remaining days.
Hi
Thanks for sharing your experience:)
Did you make any note for OBGYN1? If yes, would you share it with us? It’s very helpful! Thanks!!
No, I didn’t make any notes. I used Hatem’s notes and uptodate, mainly. I also went through the lectures once but I don’t think that was worth it.