So I had paediatrics final on the 3rd. We got no information on email ahead of the exam, but the time of the exam was 8:30 according to Neptun. I’d heard from other students who had the exam that I should show up at the southernmost part of the main corridor of the main building, close to where the library is. Because I’m an idiot I arrived a bit late, so I wasn’t among the first 3 students to be taken in. After the first student was done with their exam, I entered the room to draw topics and prepare.
The examiner that day was prof. Décsi, and the co-examiner was a young male doctor whose name I don’t know. After each student picked their topics, the professor allowed the co-examiner to choose one of the three topics to examine by himself.
My topics were:
- 15. Disorders of the humoral immune system
- 24. Hepatomegaly. Causes, diagnosis, differential diagnosis
- 15. Most common congenital heart abnormalities not causing cyanosis
The co-examiner chose the hepatomegaly topic to examine me in, and the professor asked me which topic I wanted to start with. I chose the immune system one.
15. Disorders of the humoral immune system
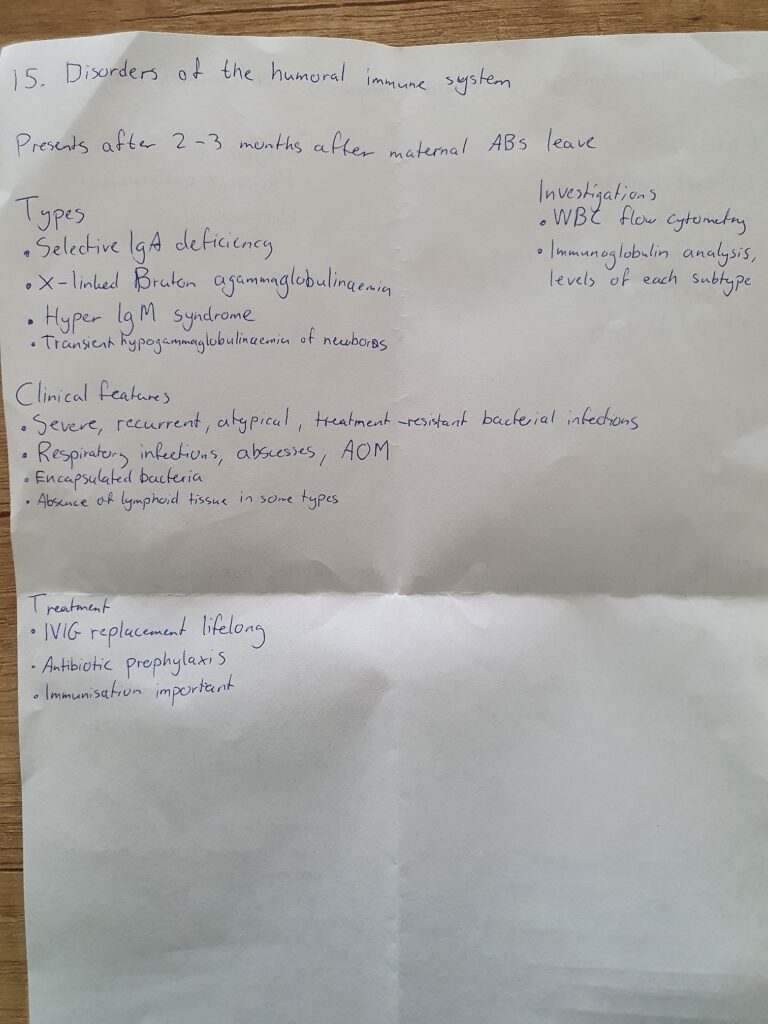
I began by telling him what I’d written down. He then begins asking me questions.
- Examiner: You mentioned the repeated and severe infections as a symptom of these disorders. What other symptoms may draw your intention to a disorder of the immune system?
- Me: So these disorders could also increase the risk of autoimmune diseases
- E: Yes. (But clearly not what he was going for) In a young child what kind of frequently occuring problem may call your attention to a potential immune disorder.
- M: (Not sure) Frequent urinary tract infection?
- E: Yes. (also not what he was going for) And what’s not far from this problem? Which is actually a manifestation of bacterial presence?
- M: Uhm, sepsis?
- E: No, in the end of course but not was I meant.
- M: Pyelonephritis?
- E: Pyelonephritis is also a urinary tract infection. What other tract can be infected and give very specific and easily detected symptoms.
- M: Gastrointestinal infections?
- E: Yes, and what will you see?
- M: Bloody stool. (Was thinking of bacterial gastroenteritis)
- E: Yes but mostly just diarrhoea. Frequent and unexplained diarrhoea. And, if the child has repeated infection and diarrhoea, then what other functions of the child will be disturbed?
- M: Growth?
- E: Oh yes. These are the three major symptoms. Next question: If a child has selective IgA deficiency like you mentioned, the diagnostic of which diseases can be complicated by this?
- M: Oh, well that’s a difficult question.
- E: Oh well yes. Up until now you did well so I increase the complexity of my questions. So where do we use IgA in the diagnosis?
- I was thinking hard on this one. For some reason coeliac disease popped into my mind, but I wasn’t confident enough to say it.
- E: It’s no problem if you can’t answer this.
- I gave it some more thought but couldn’t come up with an answer.
- M: I’m not sure.
- E: It’s coeliac disease. (Damn it! I should trust my gut.) If the patient has IgA deficiency, they will not have high levels of the antibodies we use to diagnose coeliac disease. No problem. Next topic.
15. Most common congenital heart abnormalities not causing cyanosis
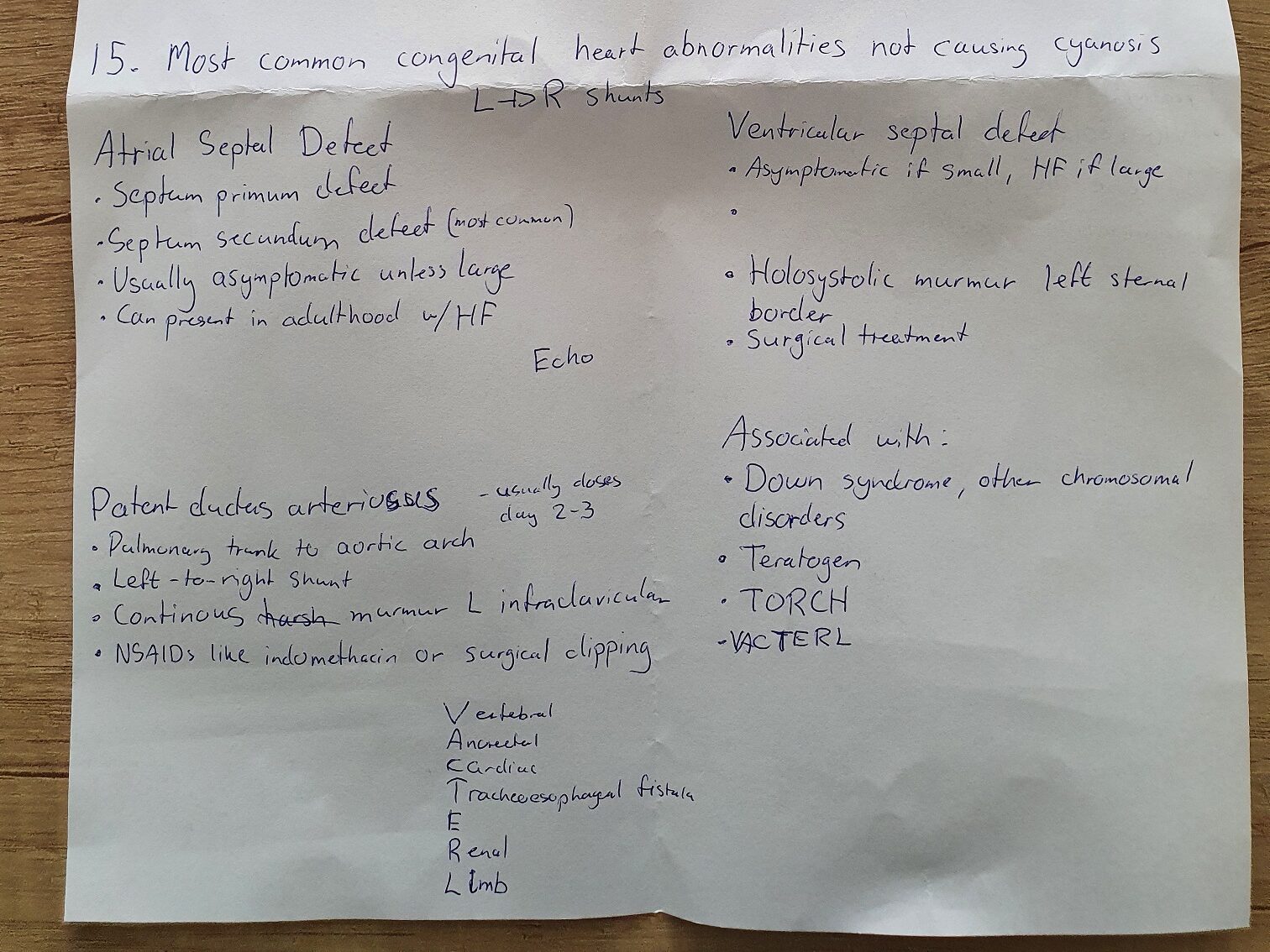
Once again I began by telling him what I’d written down about ASD. I start to list symptoms of heart failure as I explain symptomatic ASD, and I mention hepatomegaly, poor growth, dyspnoea, sweating, problems with feeding. He then interrupts me with a question:
- Examiner: What is the first sign of cardiac decompensation, before the symptoms you mentioned.
- Me: Oedema?
- E: Before oedema.
- Thinking
- E: How does the heart try to compensate?
- M: Tachycardia.
- E: Oh yes. Please continue
I continue with VSD and the rest of what I wrote down, and he has no questions after this. I continue with my last topic, at which point I turn to the co-examiner (as this was the topic he chose to examine me on).
24. Hepatomegaly. Causes, diagnosis, differential diagnosis
I begin by listing the possible causes. I then continue like this:
- Me: So in the evaluation of hepatomegaly physical examination is important. In newborns it can be physiological that the liver can be palpated 1 – 2 cm below the costal arch, but in older children you shouldn’t be able to palpate the liver that well. Ultrasound is important in accurate estimation of the size of the liver, but for proper differential diagnosis it’s not enough to only look at the liver, we must look for other features of the disease like jaundice in hepatitis, in mononucleosis you’d have cervical lymphadenopathy, in leukaemia there’d by symptoms of bone marrow failure and splenomegaly. And.. Uhm, yeah, that’s all I had prepared.
- Co-examiner: Okay, so. Hmm. He turns to the professor and says: I think he said everything, I don’t have any questions.
- Examiner: Okay, then let me ask a question. Please give me some special causes of young infant or neonatal hepatomegaly. What is the usual size of the liver at the age of 1 month?
- Oh no, is he expecting a size in centimetres? I don’t know and I’m afraid of guessing because I might be so far off. As I’m thinking about this, he continues:
- E: Is there some difference in the evaluation of liver size below or above one year of age?
- Now this is a common problem of oral exams. I feel like he’s after the fact that the liver can be physiologically palpated in infants, but I already said that in the beginning of the topic. Did he not hear me? Or is he after something else? I’m not sure, but I assume the former.
- M: So, compared to the body size, the liver is larger in infants than in older children.
- E: Yes. Also, the diaphragm is lower. So, during the first year of life, if you palpate the liver 2 cm under the costal arch then it can be physiological.
- I was right, he didn’t catch it when I said it the first time.
- E: Let’s say you have a one month old child with a liver palpateable 4 cm below the costal arch. What might be the cause?
- M: Something like biliary atresia?
- E: Yes, what other features of this biliary atresia can you see or detect during the physical examination?
- M: They would have jaundice.
- E: What type of jaundice?
- I don’t know of multiple types of jaundice, so I assume he means indirect/direct hyperbilirubinaemia?
- M: They would have direct hyperbilirubinaemia.
- E: Yes, and with your eyes, what can you see on the patient? What will be the colour of the skin?
- Now this is kind of a lucky coincidence, because I learned the answer to this exact thing during my paeds practice here in Pécs. Apparently (and allegedly), direct hyperbilirubinaemia causes a more greenish jaundice than the “usual” indirect hyperbilirubinaemia. This isn’t something I’ve heard of anywhere else, and internet search doesn’t reveal more than a few papers about it. However, as he asked this question I was pretty certain that that was the answer he was looking for.
- M: It will be more greenish.
- E: Yes, excellent. It’s a 5.
Conclusion
My exam took about 10 minutes. Neither examiner interrupted me often while I was presenting my topic, and if they did it was usually just to say “yes” or “good” now and then, which was nice. I also think it was nice of the professor to allow the co-examiner to practice examination like this. As they say, it sucks to study for paeds but the exam is quite nice. It was a good experience.
I have my thesis defence on March 11th, and neuro on April 7th. Until then, I’ll be playing Elden ring.
Bro where is the location of the paediatrics exam ? Is it that big library with all the books just near the entrance, but we have to wait near the stairs to the pulmonology ward ? Kindly let me know, thanks
I’m sorry but I don’t clearly remember. You’ll have to ask someone who had it more recently.