Page created on September 29, 2018. Last updated on December 18, 2024 at 16:56
Introduction
Circulatory shock is a circulatory disorder that’s caused by severely decreased tissue perfusion. It is a potentially life-threatening disorder because the tissue hypoperfusion results in defective supply of oxygen and nutrients and defective removal of waste-products, which damages the peripheral tissues and can lead to death.
The common clinical findings are:
- Hypotension
- Confusion
- Tachycardia
- Tachypnoea
- Cool skin
- Oliguria
Unlike syncope is this hypoperfusion not improved by assuming supine position, and levels of consciousness is actually maintained until the very last stages.
There are four types of shock. Here are the most important causes of each type:
- Hypovolemic shock – loss of intravascular fluid
- Massive blood or fluid loss
- Distributive shock – redistribution of body fluids
- Trauma
- Sepsis
- Anaphylaxis
- Acute pancreatitis
- Heat stroke
- Ileus
- Cardiogenic shock – inability of the heart to circulate blood
- Myocardial infarct
- Acute heart failure
- End-stage chronic heart failure
- Cardiac arrhythmias
- Cardiomyopathies
- Obstructive shock
- Occlusion of large vessels, pulmonary embolism
Pathomechanism
This pathomechanism is for hypovolaemic shock, but it is similar for other types as well.
When a large amount of blood is lost the body wil increase the sympathetic activity to try to maintain the blood pressure. This causes tachycardia and vasoconstriction. If the blood loss is severe enough the tachycardia and vasoconstriction are ineffective in maintaining the blood pressure.
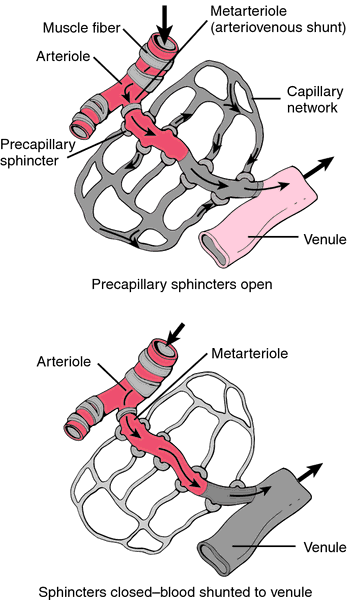
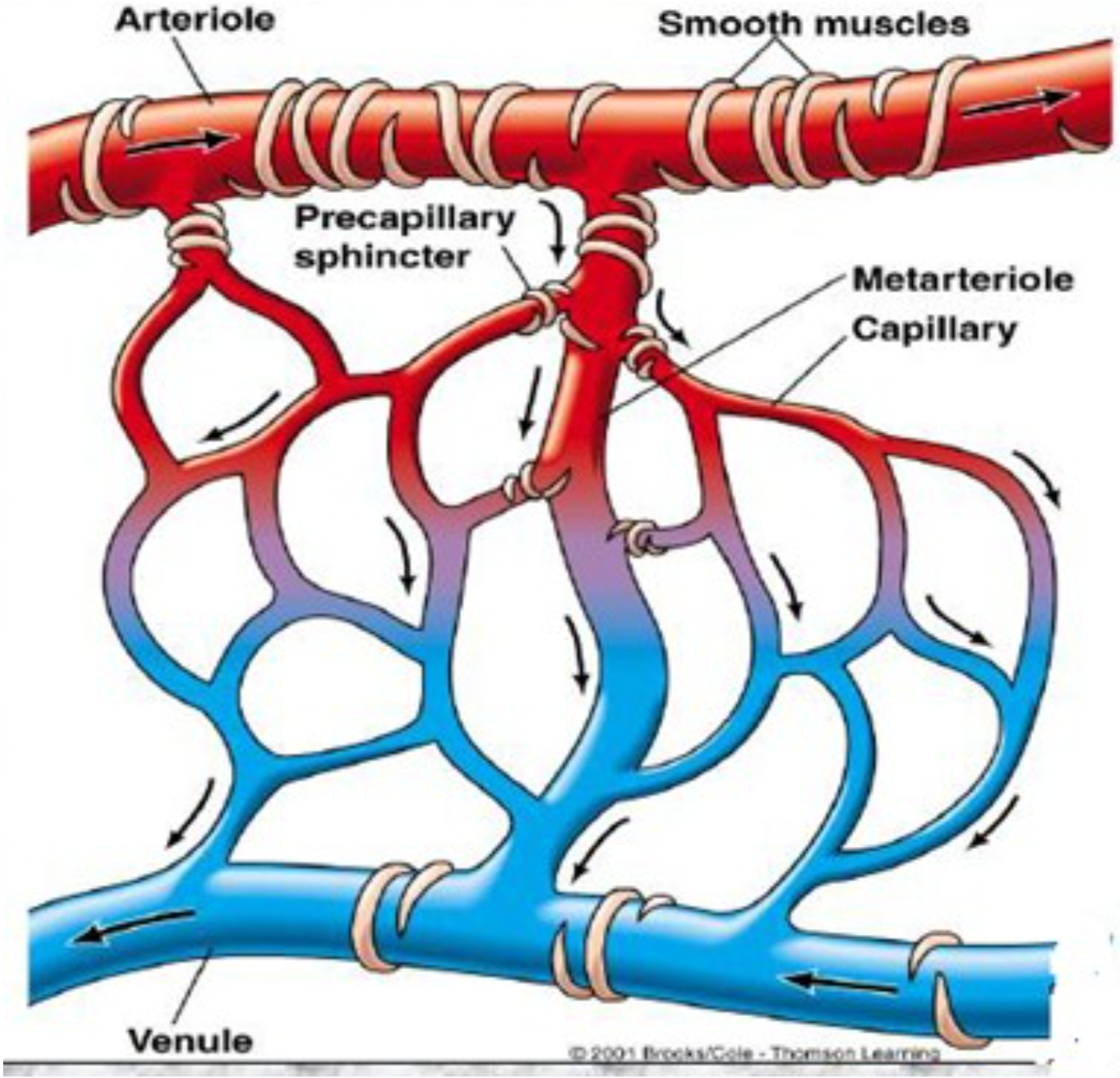
Recall that the diameter of the arteriole lumen is the main determinant of total peripheral resistance and therefore blood pressure. Due to the increased sympathetic activity the arterioles will be severely vasoconstricted. The low blood pressure and the severe constriction of arterioles decreases the amount of blood that reaches the capillaries, which causes generalized ischemia. This impaired microcirculation is fundamental in all types of shock, not just hypovolaemic shock.
Phases of shock
1. Reversible phase:
Due to arteriolar constriction is there not enough blood in the capillaries, so the capillary hydrostatic pressure is low. This causes fluid to be absorbed from the interstitium into the capillaries, which helps to maintain the blood pressure.
The skin is cool and pallor as there is vasoconstriction in the skin which shunts blood from the skin to the vital organs.
2. Compensated phase:
The little blood flow in the capillaries leads to hypoxia of the tissues. The products of hypoxic metabolism like lactate, CO2, adenosine and K+ will accumulate in the tissues. These products are vasodilators and cause precapillary sphincters to open. Little blood actually enters the capillaries due to the low blood pressure and still constricted arterioles. The circulation through the capillaries is very slow.
3. Progressive (refractory) phase:
The blood flow in the capillaries is so slow that blood stagnates and starts to clot, forming microthrombi. This is a condition called Disseminated Intravascular Coagulation (DIC). The microthrombi further impair circulation.
During this stage will there also be an accumulation of metabolic substances, lysosomal enzymes and osmotically active substances. Necrosis continues and the prognosis depends on the amount of microthrombi; the more microthrombi, the lower the chance for survival. The endothelium starts to take hypoxic damage.
4. Irreversible phase:
The irreversible phase starts when the endothelium is so damaged that causes plasma fluid starts to leave the blood and enter the interstitium. Plasma volume decreases further. At this point is there nothing can be done, and death is certain.
DIC accumulates in capillaries in all parenchymal organs. Blood volume and pressure is very low. The result of these vicious processes has reached a point where there is no recovery, multiple organ failure and death will follow.