Table of Contents
Page created on June 8, 2021. Last updated on January 17, 2022 at 14:59
Definition and epidemiology
Pelvic organ prolapse (POP) is the protrusion or herniation of bladder, rectum, intestines, uterus, cervix, or vaginal apex into the vaginal vault due to decreased pelvic floor support. This may cause symptoms of pressure in the vagina or symptoms related to the prolapsing organ.
It’s a common disorder, mostly affecting elderly women. Women have an ~5% lifetime risk of developing POP.
Risk factors
Risk factors for POP are those which lead to weakening of the pelvic floor.
- Menopause
- Pregnancy – the weight of the pregnancy puts stress on the pelvic floor
- Multiparity
- Vaginal childbirth (especially in case of macrosomia, episiotomy, etc.)
- Chronically increased intraabdominal pressure (COPD, constipation, obesity)
- Connective tissue disease (Marfan, EDS)
Pathomechanism
One theory is that the levator ani muscle is important in the pathomechanism, which is either directly damaged or suffers denervation or ischaemic injury.
Another theory is that connective tissue failure is important.
DeLancey has distinguished three levels of vaginal support:
- Level I support – apical suspension
- Damage results in apical compartment prolapse
- Level II support – midvaginal lateral attachment
- Damage results in anterior compartment prolapse
- Level III support – distal perineal fusion
- Damage results in posterior compartment prolapse or perineal deficiency
Classification
We classify the pelvic organ prolapses according to the prolapsed organ:
- Anterior compartment prolapse (prolapse through the anterior vaginal wall)
- Cystocoele – (prolapse of the bladder)
- Urethrocoele
- Apical/Middle compartment prolapse
- Uterine prolapse
- Vaginal apex prolapse
- Cervical prolapse
- Posterior compartment prolapse (prolapse through the posterior vaginal wall)
- Rectocoele
- Enterocoele
The most common forms are cystocoele and rectocoele. Patients may experience prolapse of more than one organ or compartment simultaneously.
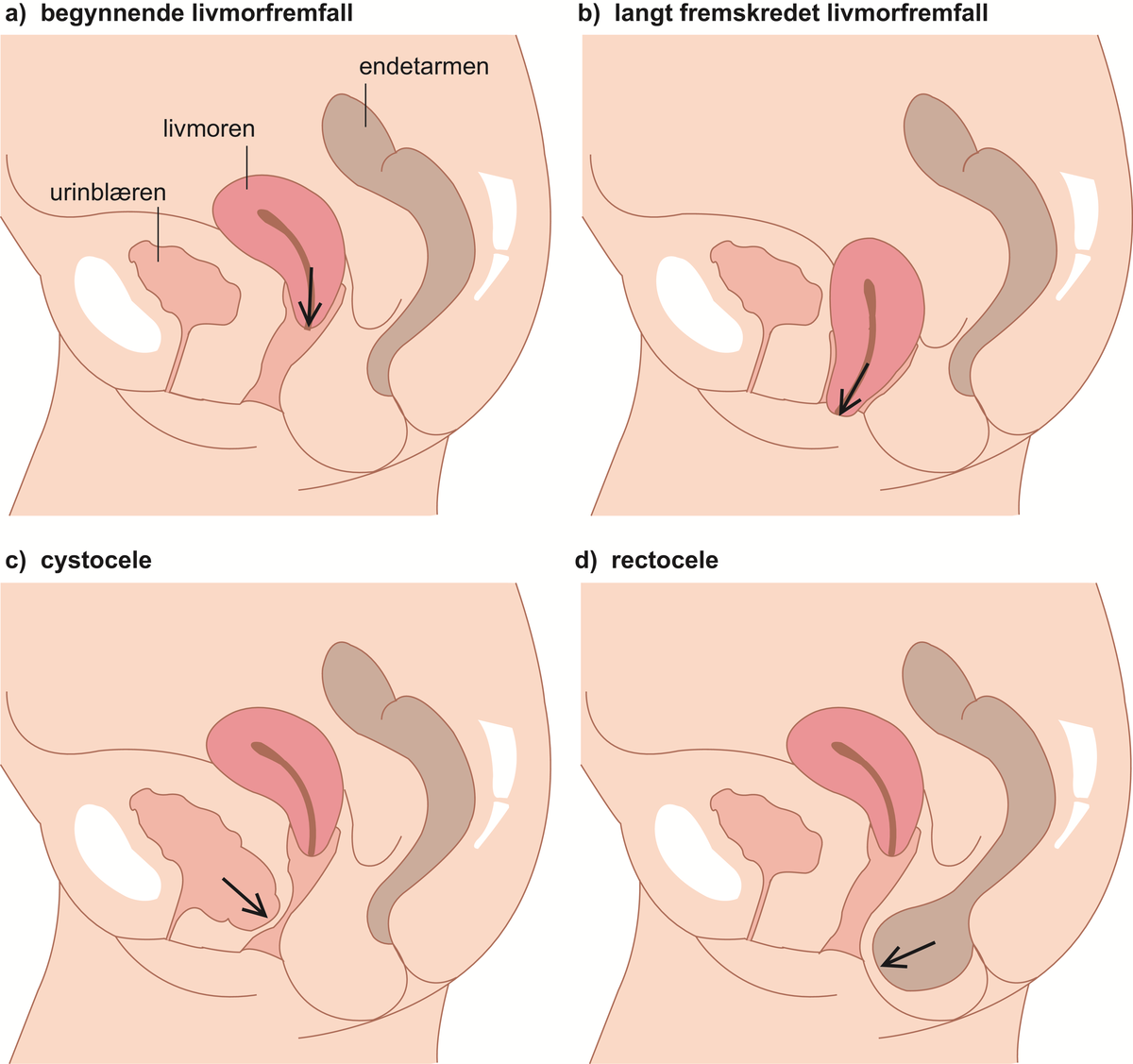
a) and b) show a beginning and manifest uterine prolapse. From https://sml.snl.no/fremfall
The objective severity of the prolapse is measured relative to the hymen according to POP-Q system:
- Grade 0 – no prolapse
- Grade 1 – descent reaches no further than 1 cm proximal to the hymen
- Grade 2 – descent reaches to within 1 cm proximal or distal to the hymen
- Grade 3 – descent reaches further than 1 cm distal to the hymen
- Grade 4 – maximum descent (total prolapse)
Clinical features
There’s often a discrepancy between the findings on physical examination and the patient’s complaints. An objectively severe prolapse may cause the patient few symptoms or vice versa.
Pelvic organ prolapse can cause a variety of symptoms, many depending on the prolapsed organ.
- Bulge symptoms
- Sensation of vaginal bulging or protrusion
- Pelvic or vaginal pressure or heaviness
- In case of cystocoele or urethrocoele
- Urinary incontinence
- Frequency
- Urgency
- Feeling of incomplete emptying
- Hesitency
- In case of rectocoele or enterocoele
- Faecal incontinence
- Feeling of incomplete emptying
- Hard straining to defecate
- Sexual symptoms
- Dyspareunia
- Decreased lubrication
- Decreased sensation
- Pain (lower abdominal or back)
The patient may complain of having to manually reduce the prolapse to start voiding or defecating.
Diagnosis and evaluation
The patient should be physically examined in the lithotomy position with a full bladder. The patient is asked to perform the Valsalva manoeuvre or to cough. This triggers the prolapse.
Then the patient is examined with vaginal retractors (and not the Cusco speculum). This allows us to assess each of the compartments of the vagina, the anterior vaginal wall, the posterior vaginal wall, and the apical compartment. This is required to assess the POP-Q and the severity of the prolapse.
Transvaginal or transperineal ultrasound can be used to evaluate the pelvic floor. It’s also important to look for the vaginal rugae, as the absence of these can indicate POP.
The Q tip test can be used to assess urethral hypermobility and urinary incontinence. A Q tip is inserted to the urethra-vesicular junction, and the patient is asked to perform Valsalva. If the Q tip lifts more than 35 degrees, the test is positive.