Table of Contents
Page created on January 4, 2019. Last updated on January 7, 2022 at 22:06
Eicosanoids
You already know these bad boys, prostaglandins, thromboxanes and leukotrienes. They’re synthesized from membrane phospholipids, which are first converted into arachidonic acid by phospholipase A2.
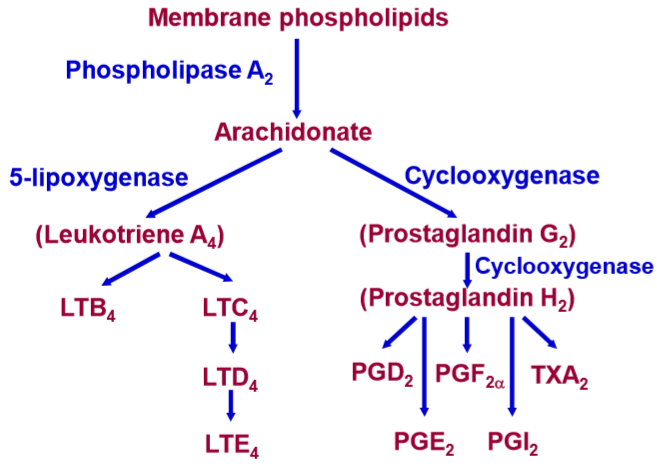
Synthesis of eicosanoids.
These molecules are very short-lived, meaning that they’re rapidly broken down in plasma after they’re produced. Their half-life is only 1 minute! They’re called eicosanoids because they are 20 carbons long fatty acids, and the Greek word for 20 is είκοσι, or eikosi. Prostaglandins, prostacyclins and thromboxanes are collectively called prostanoids.
Prostanoids (prostacyclins, prostaglandins and thromboxanes):
Cyclooxygenase (COX), which produces prostanoids, has two isoforms: COX-1 and COX-2. COX-1 is constantly expressed and produces prostanoids that have physiological, homeostatic functions.
COX-2 on the other hand is inducible, so it’s only activated when needed. It’s activated in response to pathological stimuli like inflammation or injury. These prostanoids play a role in inflammation, pain and fever.
Prostanoids act on G-protein coupled receptors. Here are some of them. This isn’t important to know, just illustrative.
| Receptor | Second messenger | Effect | Distribution |
| IP
DP1 EP2 EP4 |
↑ cAMP | “Inhibitory actions”
Smooth muscle relaxation |
Cardiovascular system
Platelets Neurons |
| TP
FP EP1 |
↑ Ca2+ | “Excitatory actions”
Smooth muscle contraction |
Cardiovascular system
Platelets Immune system |
| EP3
DP2 |
↓ cAMP | “Inhibitory actions”
Smooth muscle relaxation |
Throughout the body |
Here are some of the physiological functions of prostanoids:
- Prostaglandins:
- cause vasodilation
- enhances capillary permeability with histamine and bradykinin
- increases sensitivity of nociceptors
- inhibit platelet aggregation
- cause bronchodilation
- induce cough
- causes contraction of uterus in pregnant women
- causes relaxation and dilatation of cervix in pregnant women
- decreases acid secretion
- vasodilate afferent arteriole in kidney
- increase Na+, K+ and water excretion
- induce fever by acting on the hypothalamus
- maintain the ductus arteriosus
- Thromboxanes:
- cause vasoconstriction
- promote platelet aggregation
Leukotrienes:
Leukotrienes act on BLT1, BLT2, CysLT1 and CysLT2 receptors. They mostly work by activating and stimulating immune cells, but also:
- Increase sensitivity of nociceptors
- Bronchoconstrict
- Cause swelling of bronchi
- Increase mucus secretion in bronchi
- Vasodilate
- Increase capillary permeability
Leukotriene agonists and antagonists
- Leukotriene agonists
- None
- Leukotriene antagonists
- Zafirlukast
- Montelukast
Indications:
Leukotriene agonists have no therapeutic use.
Leukotriene antagonists are used in the maintenance treatment of bronchial asthma. They’re taken orally.
Aspirin asthma:
Leukotrienes are involved in the development of NSAID-induced airway obstruction, so-called “aspirin asthma”. NSAIDs inhibit COX. When COX is inhibited all the arachidonic acid molecules that are produced will be converted into leukotrienes. Leukotrienes cause swelling, increased mucus secretion and bronchoconstriction in the bronchi, causing asthma.
Prostanoid analogues
- Alprostadil (= prostaglandin E1)
- Misoprostol (prostaglandin E1 analogue)
- Dinoprostone (= prostaglandin E2)
- Epoprostenol (= prostacyclin I2)
- Carboprost (prostaglandin F2α analogue)
- Latanoprost (prostaglandin F2α analogue)
Indications:
- Misoprostol
- Termination of pregnancy
- Induction of labour
- Preventing NSAID-related ulcers
- Maintaining ductus arteriosus
- Erectile dysfunction – as an injection into the corpus cavernosum
- Dinoprostone
- Induction of labour
- Carboprost
- Postpartum haemorrhage
- Epoprostenol
- Inhibit platelet aggregation during extracorporeal circulation
- Primary pulmonary hypertension
- Latanoprost (eye drops)
- Open-angle glaucoma
Eicosanoids in general have very short half-life, so instead of giving eicosanoids we often give eicosanoid analogues, which are molecules that are similar in structure and have similar effects but have longer half-life. However, many of the drugs mentioned are just drug names for endogenous eicosanoids. Dinoprostone is the exact same molecule as prostaglandin E2, for example.
Mechanism of action:
Prostaglandin E1 and E2 analogues induce contraction of the uterus, thereby causing termination of pregnancy or induction of labour, depending on the concentration used.
Prostaglandin F2α analogues like carboprost induce contraction of the uterus and induce lysis of the corpus luteum, thereby stopping post partum bleeding. Normally, contraction of the uterus during labour compresses the blood vessels and thereby prevents haemorrhage. A lack of uterine contraction, called uterine atony, is the most common cause of post partum haemorrhage and can be treated with carboprost.
Prostaglandin E1 analogues like misoprostol acts on EP3 receptors in the stomach and inhibits HCl secretion and induces gastric mucus secretion, thereby preventing ulcer development.
Prostaglandin E1 is important in maintaining the ductus arteriosus in infants. Alprostadil keeps the ductus arteriosus open, which is beneficial for congenital heart defects that need surgery when the ductus arteriosus is necessary for the survival before the surgery, so-called ductus-dependent congenital heart lesions.
Alprostadil relaxes vascular smooth muscle in the corpus cavernosum when injected into it, thereby inducing erection.
Epoprostenol (prostacyclin I2) induces vasodilation in the pulmonary circulation when given IV. It also inhibits platelet aggregation.
Latanoprost decreases intraocular pressure.
Pharmacokinetics:
The only orally active prostanoid analogue is misoprostol. All the others must be given by injection or as eye drops.
Adverse effects:
- For all
- Fever
- GI symptoms
- Prostaglandin F2α analogues
- Bronchoconstriction
- Hypertension
- Prostaglandin E2 analogues
- Hypotension
- Prostacyclin I2 analogues
- Hypotension
Drugs that inhibit formation of eicosanoids
NSAIDs inhibit COX-1 and/or COX-2, depending on the type of NSAID.
Glucocorticoids increase the synthesis of lipocortin, a protein which inhibits phospholipase A2.
Drugs which relax smooth muscle
- Spasmolytics
- No clinical use
- Papaverine
- Drotaverine
- Metamizole
- Butylscopolamine
- Bencyclane
- No clinical use
Many drugs act on smooth muscle, including eicosanoids, however we reserve the name spasmolytic drugs for drugs that prevent spasms of the smooth muscles in the GI tract or genitourinary tract.
Indications:
They’re used to treat spasms, often those that occur due to bile stone or kidney stone.
Mechanism of action:
There are two types of spasmolytics: the directly-acting ones, that work by influencing ion channels or enzymes, and the indirectly-acting ones, which act on receptors. Papaverine, drotaverine, bencyclane and metamizole are direct spasmolytics. Butylscopolamine is an indirect spasmolytic.
Papaverin is a phosphodiesterase (PDE) 3 and 4 inhibitor, and it also inhibits L-type calcium channels. Drotaverine is similar but is specific for PDE4 and doesn’t act on calcium channels.
Bencyclane acts by inhibiting L-type calcium channels.
Metamizole is an NSAID with additional direct spasmolytic effects.
Butylscopoloamine is a quaternary amine muscarinic receptor antagonist, which gives it indirect spasmolytic effects.
Drugs which contract smooth muscle
- Oxytocin
- Prostaglandins (see above)
- Dinoprostone
- Misoprostol
- Carboprost
- Ergot alkaloids
- Ergometrine
- Ergotamine
Prostaglandins and oxytocin are essential for contraction of the uterus. Prostaglandins’ role in this was discussed above.
Indications:
- Oxytocin
- Induce labour
- Postpartum haemorrhage
- Promote lactation
- Ergot alkaloids
- Induce abortion
- Postpartum haemorrhage
Mechanism of action:
Oxytocin is a peptide hormone formed in the hypothalamus but released from the posterior pituitary. It acts through a Gq-coupled receptor, meaning that it activates phospholipase C. When secreted it evokes rhythmic contractions of the uterus and cause milk ejection in the breasts. Between the contractions are periods of complete relaxation so that foetal asphyxiation doesn’t occur.
The ergot alkaloids act by unknown mechanisms. They cause a sustained contraction with no periods of relaxation, so if they were used while a live foetus is in the uterus the foetus would die.
Pharmacokinetics:
Oxytocin has a short half-life due to rapid elimination by the liver and kidney.
Tocolytics
Tocolytics are drugs which postpone labour by causing uterine smooth muscle to relax. Many drugs can act as tocolytics:
- β2 adrenergic agonists
- Terbutaline
- Salbutamol/albuterol
- Calcium channel blockers
- Nifedipine
- Oxytocin receptor antagonists
- Atosiban
- NSAIDs
- Indomethacin
I believe prostaglandins increase Na+,K+, H2O EXCRETION not retention. Thanks for everything!
I believe you’re correct. Fixed.
You’re welcome!
Latanoprost is misspelled under prostanoid analogues as:
Latanaprost (prostaglandin F2α analogue)
Eye game strong
It says Dineprostone under indication of PROSTANOID ANALOGUES and Dinepristone under DRUGS WHICH CONTRACT SMOOTH MUSCLE. Is there mispelling of Dinoprostone?
I’ve corrected all misspellings of dinoprostone. Good catch
Is there a misspelling in the table? I don’t understand how both increase and decrease of cAMP can have the same inhibitory effect. Could you please explain this to me?
It’s not a mistake. Reduction or increase in cAMP is not the “target” in cell signalling, it is only a second messenger. Whether a reduction or increase in the level of the second messenger has “excitatory” or “inhibitory” effects on the cell depend on the mechanisms downstream from the cAMP, which may differ from one type of cell to another. In some cells an increase in cAMP may produce smooth muscle relaxation, in others a decrease may produce relaxation.
Anyway, the table is not important to know.
Is there a role of prostaglandins in retinopathy of prematurity? ROP is due to vascular disfunction of retina. Prostaglandins can be in high concentrations in PDA of prematures. will the same conditions can cause ROP ?
I know literally nothing about ROP, but a quick google search reveals that you are right. According to this article the high perinatal level of prostaglandins is involved in the pathogenesis of ROP.
This was very greek <3