Table of Contents
Page created on January 7, 2019. Last updated on December 18, 2024 at 16:57
Summary
- Drugs can be excreted mainly by renal excretion or by biliary excretion
- Drugs with renal excretion above 100 mL/min are secreted to some extent
- The excretion of weak acidic drugs can be enhanced by administering NaHCO3
- The excretion of weak basic drugs can be enhanced by administering NH4Cl
Drug elimination:
When we talk about elimination of drugs we focus on the parent drug. That means that excretion and biotransformation of the parent drug are both elimination mechanisms, but elimination of the metabolites don’t count as elimination of the drug. When the parent drug is metabolized we consider the drug eliminated from the body, but not yet excreted.
The body can eliminate a drug in two ways: by excretion or by biotransformation. Whether the drug is excreted or converted into an inactive metabolite is it considered eliminated from the body.
Excretion occurs via two major pathways and three minor pathways:
- Renal excretion into the urine
- By glomerular filtration or tubular secretion
- Biliary excretion into the feces
- Pulmonary excretion via exhalation
- Glandular excretion into milk, saliva or sweat
- Gastrointestinal excretion across the GI mucosa
Renal excretion
Drugs can be eliminated by the kidneys via two ways, by glomerular filtration or by tubular secretion. In addition to this elimination may be counteracted if the tubules reabsorb the drug that was just excreted.
Clearance
Before we continue must we understand clearly what clearance means. The concept of clearance is the body’s capacity to eliminate a drug. Clearance is a measurement that shows the volume of plasma that a certain substance (such as a drug) can be completely removed from, per unit of time. For example, a clearance of diazepam is around 25 mL/min. That means that every minute will the kidney remove all diazepam from 25 mL of plasma.
You can visualize this like this: Imagine you fill up a large bowl with your plasma volume. The plasma volume contains diazepam. A clearance of 25mL/min means that every minute will the kidney use a ladle to remove 25 mL of plasma volume. It then removes all diazepam molecules from those 25 mL, and after it has done that will it put the cleared plasma volume back with the rest in the bowl.
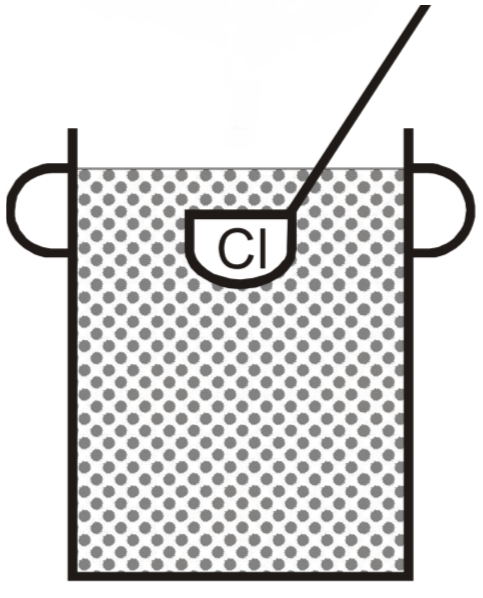
The kidney uses this ladle to remove diazepam (the dots) from a certain volume every minute
We can talk about total body clearance, which includes the clearance of the feces, exhalation and glandular excretions, but when we talk about clearance do we usually mean the renal clearance.
When we talk about clearance we must talk about creatinine and PAH as well. Creatinine is a breakdown product of creatine in the body. What’s special about it is that is completely filtered, not secreted and not reabsorbed. This means that all the plasma that reaches the glomerulus is completely cleared of creatinine. Around 100 mL of plasma reaches the glomeruli every minute, and because all of this is cleared of creatinine can we understand that the clearance of creatinine is 100mL/min, the same as the GFR. The same is true for any compound that is completely filtered and not reabsorbed or secreted.
The clearance of PAH is much higher, around 600 mL/min. Only 100 mL plasma reaches the glomeruli every minute, so how can PAH be cleared from 600 mL of plasma every minute then? This is accomplished because PAH isn’t just completely filtered, it’s completely secreted and not reabsorbed as well. This means that 100 mL of plasma is cleared of PAH by glomerular filtration, and the remaining 500 mL is cleared by tubular secretion of PAH into the filtrate. 600 mL/min is also the total renal plasma flow (RPF) per minute. The clearance of PAH is equal to the RPF because all the plasma that reaches the kidney per minute is completely cleared of PAH, both by filtration and by secretion.
In fact, the only way the clearance of a compound (such as a drug) can be higher than 100 mL/min is if it is secreted, because filtration only has a capacity of 100 mL/min. However, not all compounds with clearance > 100 mL/min are necessarily freely filtrated like PAH and creatinine. A drug with clearance 300 mL/min can have 50 mL/min of this clearance done by filtration and the remaining 250 mL/min done by tubular secretion.
Glomerular filtration:
For drugs to be excreted by glomerular filtration must they meet some requirements:
- Be water soluble
- Be smaller than 60 kDa
- Have low plasma protein binding
Glomerular filtration works by molecules passing through pores next to the epithelial cells, and not by carrier-proteins. Antibodies are very large molecules that can’t fit through the pores, so they’re not filtered via the glomerulus.
The rate of glomerular filtration of a drug depends on two things:
- The concentration of the drug in the plasma
- The glomerular filtration rate (GFR)
The higher the concentration of the free (not protein-bound) drug in the plasma, the faster it’s filtrated. The GFR never really increases above the normal, but it can be decreased, such as in renal failure. This decreases the glomerular filtration of the drug, which increases the half life of the drug in the plasma.
Aminoglycosides for example are eliminated mainly in unchanged form by glomerular filtration.
Tubular secretion:
Unlike glomerular filtration is tubular secretion driver by carrier proteins. It has different carrier protein systems for organic acids, organic bases and for organic neutral compounds. Here are some examples of drugs that are excreted by tubular secretion:
- Organic acids
- Cephalosporins
- PAH
- Fluoroquinolones
- NSAIDs
- Organic bases
- Tubocurarine
- Neostigmine
- Organic neutral compounds
- Digoxin
Tubular reabsorption works mostly by diffusion, but some drugs have carrier proteins that reabsorb them into the plasma. Tubular reabsorption is very important in the clearance of some drugs. Let’s look at two drugs with very similar pharmacokinetic characteristics except for their reabsorption.
| Gentamicin | Fluconazole | |
| Plasma protein binding |
Little <10% |
|
| Glomerular filtration |
Freely filtered |
|
| Tubular reabsorption | Minimal <2% | Extensive 80% |
| Renal clearance | 90 mL/min | 18 mL/min |
| Half life | 3 hours | 30 hours |
See how the clearance of fluconazole is much lower than gentamicin? That’s because it has extensive reabsorption compared to gentamicin. Note also how the clearance of gentamicin is almost 100 mL/min, because it’s barely reabsorbed at all, just like creatinine.
What influences the tubular reabsorption of drugs? Two things:
- The tubular fluid flow rate
- The strength of the acid or base
1: The tubular fluid flow rate, which is the rate with which the filtrate is flowing through the tubules can be increased by diuretics. If the filtrate flows faster will the drugs in the filtrate have less time to diffuse back into the blood.
2: Drugs that are strong acids and strong bases are mostly in the ionized form when in the normal pH of the filtrate. Ionized compounds are less lipophilic, so they diffuse less. Weak acids and weak bases exist in both ionized and non-ionized form in the filtrate. The non-ionized form is more lipophilic than the ionized form, so it may diffuse. Weaker acids and bases are therefore reabsorbed more than stronger ones.
By manipulating the pH of the filtrate can we increase or decrease the tubular reabsorption of drugs, like this:
- By administering a base like NaHCO3 intravenously the filtrate will become more basic, which means that the number of H+-ions decreases. For drugs that are weak acids does that mean that the acid equilibrium will be pushed toward the A–-form. This means that more of the drug molecules will be in ionized, hydrophilic form and fewer will be in the un-ionized, hydrophobic form. This decreases the diffusion and therefore the reabsorption. This can be used to increase clearance of acidic drugs.
- By administering an acid like NH4Cl will the filtrate be more acidic. For drugs that are weak bases will more of the drug molecules be in ionized form and fewer in the un-ionized form, which decreases the reabsorption.
Biliary excretion of drugs
Recall from histology that mixed blood from the portal vein and hepatic artery flows in the hepatic sinusoids into the central vein. Hepatocytes and endothelial cells face these sinusoids. The endothelial cells have large pores called fenestrae, and the hepatocytes have microvilli, both of which enhance the diffusion and transport of molecules from the blood into the hepatocytes.
The hepatocytes also face the bile canaliculi which eventually form the bile duct. This means that hepatocytes can take molecules up from the blood and dump them into the bile. The bile is then excreted together with feces.
So which molecules are excreted into bile? We call compounds that are preferentially excreted in bile rather than urine cholephilic compounds. They have both of these characteristics:
- Relatively large molecules (> 500 Da)
- Amphipathic molecules (molecules that are both apolar and polar on different sites of the molecule)
Not too many drugs fit these characteristics, so we can understand that renal excretion is more common than biliary excretion. However, some important molecules are excreted through bile, such as:
- Bile acids (of course)
- Ceftriaxone (3rd generation cephalosporin)
- Statins
- Rifampin
- Erythromycin
Biliary excretion works by carrier-mediated transport, meaning that only drugs that are substrates of the carrier proteins found on the hepatocytes can be excreted into bile. Several carrier proteins are present on the hepatocyte membranes, like:
- MRP family
- Pgp
- BCRP
- OAT
- OCT
- OATP
Often are drugs carried from the sinusoidal blood into the hepatocyte, where they are biotransformed and then transported into the bile to be excreted. Sometimes are drugs taken up by the hepatocytes and exported back into the blood without doing any biotransformation, and sometimes will the hepatocyte take up a drug, biotransform it and export it back into the sinusoidal blood.
Intestinal reabsorption
Not all drugs that are excreted into the bile are excreted with the feces. There is a long way from the sphincter of Vater to the anus, meaning that drugs excreted into the bile have a lot of time to be at least partly reabsorbed by the intestines and back into the blood. This is called enterohepatic circulation (EHC).
In some cases can the biotransformation done by the liver be reversed in the colon. This happens with drugs that are glucuronidated as part of the biotransformation. Intestinal bacteria produce an enzyme that removes glucuronic acid from the metabolite, often converting it back into the parent drug!
In some cases is a drug excreted both as the parent drug and as a metabolite. Rifampin for example is partially biotransformed, so both unchanged rifampin and its metabolite are excreted through bile. The unchanged rifampin is reabsorbed, while the metabolite isn’t.
It’s easy to see that drugs that are reabsorbed in the intestine is eliminated from the body slower, meaning it has a longer half-life (T1/2). If the EHC returns large amounts of drug will there be a second peak in plasma concentration a few hours after the drug was administered.
We can use the EHC to our advantage. If we want a drug with long-lasting effect can we choose one that is excreted by bile and reabsorbed in the intestines instead of one that would need multiple oral or IV doses.
Sometimes do we want to interrupt the EHC, for example in overdosing, to increase the elimination of the drug. We can do this by giving the patient charcoal or cholestyramine orally, which binds to the drug in the intestine and prevents it from being reabsorbed.
The EHC can also by accidently interrupted by use of antibiotics that kill the intestinal bacteria. These bacteria are important for the intestinal reabsorption, as explained above.
Clinical significance
Why is it important to know the method of elimination for a drug? Multiple reasons:
- Drugs eliminated by biliary excretion are safer for patients with kidney problems than drugs eliminated by renal excretion
- Drugs eliminated by biliary excretion are less safe for patients with cholestasis or significant liver dysfunction
- Antibiotics excreted into bile may be more effective against biliary infections
Certain drugs may precipitate in the bile, causing it to block the bile flow. This is the case for ceftriaxone, a 3rd generation cephalosporin. Prolonged high-dose ceftriaxone treatment may cause obstructive jaundice.
Other excretory routes
- Pulmonary excretion
- For gases and volatile liquids
- Glandular excretion
- Into milk, saliva or sweat
- Not very clinically important, but can be used to detect traces of illegal drugs
- Gastrointestinal excretion
- Drugs excreted into stomach: Amphetamine, methadone
- Drugs excreted into intestine: Phenobarbital, theophylline
hello greek.doctor
in the last part, you wrote that amphetamine is excreted into the stomach, but in ”21. Psychomotor stimulants and nootropic agents”, amphetamine is excreted unchanged from the urine. is it a typing error or it depends on the situation?
thanks alooot.
Amphetamine is mainly elimiated by urine. According to the seminar, amphetamine is also excreted into the stomach. I can’t find any other source for this, so I’d take it with a grain of salt. I suspect that only a clinically insignificant amount of amphetamine is excreted into the stomach.
thanks alot. u rock
Hey bro in the beginning of the topic in the summary you wrote:-
The excretion of weak basic drugs can be enhanced by administering NaHCO3
The excretion of weak acidic drugs can be enhanced by administering NH4Cl.
……it should be the opposite!! although i am sure its just a typo cause you explained right below.
thanks for everything 🙂
Thanks bro! Yeah, just a typo, luckily I didn’t make the same typo in the flashcards. Fixed now.