Page created on January 4, 2019. Last updated on January 7, 2022 at 22:21
| Ester type local anaesthetics | Amide type local anaesthetics | Toxins | |
| Benzocaine | Intermediate duration | Long duration | Saxitoxin (STX) |
| Cocaine | Lidocaine | Bupivacaine | Tetrodotoxin (TTX) |
| Procaine | Mepivacaine | Levobupivacaine | |
| Tetracaine | Prilocaine | Ropivacaine | |
Local anaesthetics are drugs that are used to prevent or eliminate pain, often during smaller surgical procedures. This is in contrast to general anaesthetics, which work on the CNS and induces a state where the patient is unconscious and unable to feel pain.
Indications:
- Surface anaesthesia – by applying directly to mucous membrane or skin
- As a spray, gel, ointment, etc.
- Infiltration anaesthesia – by giving multiple injections targeting small nerve branches, as done at the dentist
- Nerve block anaesthesia – giving injections close to major nerve trunks, which anaesthetizes the entire are innervated by this trunk
- Spinal anaesthesia – by administering directly into the subarachnoid space, into the CSF
- Epidural anaesthesia – by administering directly into the epidural space
- IV regional anaesthesia – giving IV and applying a tourniquet to an extremity
Mechanism of action:
Local anaesthetics work by reversibly blocking voltage-gated Na+ channels. These channels are responsible for the upstroke phase of the action potential in nerve fibres. By blocking them will there be no depolarization, so nociceptive nerve signals won’t be carried to the brain. These drugs physically “plug” and therefore block the channels. At high concentrations they may block other ion channels as well.
The degree to which the nerve fibre is myelinated is important for the effect of these drugs; thin myelinated fibres are more affected than thick fibres. Thin fibres like Aδ and C are the most sensitive to local anaesthetics. The Aδ fibres is responsible for the initial sharp pain, while the C fibres are responsible for the prolonged, less intense pain. From this can we understand that local anaesthetics work better against nociceptive nerves than other nerves, which is good.
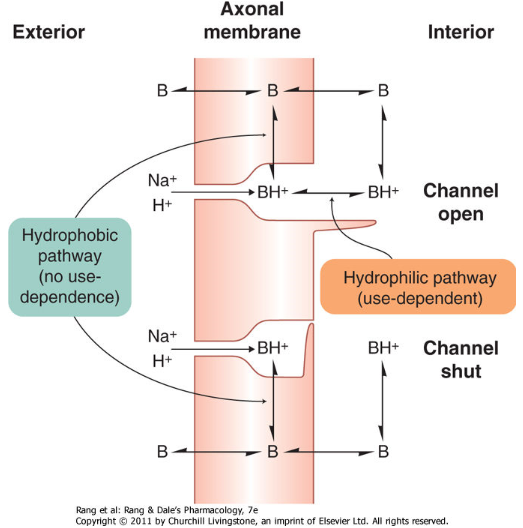
All local anaesthetics are weak bases, meaning that they have pK between 7-9. This means that at physiological pH are most of the drug molecules ionised, i.e. in the form of drug-H+, or BH+, because they’re bases. If the pH is lower than normal are more drugs in the BH+ form, if the pH is higher than normal are more in the lipophilic B form. The BH+ form is the active form.
These drugs bind to Na+ channels from the inside of the fibre, not from the outside. They must therefore diffuse across the lipid membrane of the axon to get to the inside in order to work. We know that charged molecules diffuse more poorly across the membrane, so the more drug molecules that are unionised (in the lipophilic B form, not the BH+ form), the better the diffusion. In other words, the lower the pH the fewer drug molecules can diffuse across the membrane to block the ion channel.
Recall that the pH inside cells is more acidic than in the interstitium and plasma. Because of this will more drug molecules be ionised to the active BH+ form inside the cell. This is called ion trapping.
During rest the voltage-gated Na+ channels are closed from the inside of the cell (see the figure below), so the local anaesthetics can’t plug them. As soon as the action potential arrives and the channels open the drugs will plug them before any Na+ can enter the cell. From this can we understand that more active fibres, fibres that fire more often, are more efficiently blocked, because the ion channels open more often. This phenomenon is called use-dependence, meaning that the anaesthetic effect is increased in more active nerve fibres.
Pharmacokinetics:
The anaesthetic effect stops when the local anaesthetic is absorbed from the tissue they’re applied to into the plasma. From this can we gather that the higher the perfusion of the tissue, the shorter the duration of the drug. Applying vasoconstrictors together with the anaesthetic can therefore prolong the duration of action.
The systemic side effects also occur when the anaesthetics are taken up into the plasma. Therefore, the shorter the plasma half-life, the fewer systemic side effects. Amide type local anaesthetics bind more easily to plasma proteins than ester types, and therefore have fewer systemic side effects.
Esters are hydrolysed in the plasma and liver by pseudocholinesterase while amides are metabolised in the liver by P450.
Summary of pharmacodynamics and pharmacokinetics:
- The effect of local anaesthetics during inflammation is weaker
- Because in inflammation there is acidosis, meaning that fewer drug molecules are in the B form that can diffuse across the membrane.
- Highly active nerve fibres are blocked more efficiently than less active fibres
- The more lipophilic the drug is the more suitable it is for surface anaesthesia
- The effect of local anaesthetics is terminated by absorption into the systemic circulation
- Giving a vasoconstrictior like adrenaline together with the local anaesthetic decreases the perfusion of the anaesthetized area, thereby decreasing the absorption of the drug into the plasma.
- This decreases systemic side effects and increases the duration of anaesthesia
Side effects:
Voltage-gated Na+ channels are found everywhere, so when the local anaesthetics are absorbed into the plasma channels all over the body can be affected.
- CNS effects:
- Tremor
- Confusion, agitation
- Paralysis
- Seizures
- Cardiovascular effects:
- Bradycardia (negative chronotropic effect)
- AV block (negative dromotropic effect)
- Decreased contractility (negative inotropic effect)
- Arrhythmias
- Vasodilation
- Allergic reactions
- Mostly to ester local anaesthetics
Spinal anaesthesia carries some extra risk. Not only sensory nerves travel in the spinal cord, but autonomic and motor nerves as well. The following effects may occur:
- Sympathetic block -> Bradycardia, hypotension
- Parasympathetic block -> urinary retention
- Paralysis of phrenic nerve
Ester type local anaesthetics
- Cocaine
- Procaine
- Tetracaine
- Benzocaine
Indications:
Cocaine and procaine are rarely used. Tetracaine is mainly used before venipuncture.
Benzocaine is not absorbed through the skin and can be used in wounds and ulcerated surfaces.
Pharmacokinetics:
Procaine has short duration of action. Tetracaine has long duration of action.
Tetracaine is metabolized slowly and should therefore be given with a vasoconstrictor.
Benzocaine is not soluble at all and is instead given in solid form, as a powder, suspension or a gel.
Side effects:
Cocaine is also a sympathomimetic drug, so it causes psychomotor stimulation and euphoria. It also causes local irritation.
Amide type local anaesthetics
- Intermediate duration of action
- Lidocaine
- Prilocaine
- Mepivacaine
- Long duration of action
- (Levo)bupivacaine
- Ropivacaine
Indications:
Lidocaine is the most used local anaesthetic for the skin as it has the highest penetration to the skin. It can also be given IV as an antiarrhythmic. As a gel Lidocaine can be used prior to catherization of the bladder or in the form of a spray prior to performing laryngoscopy.
Side effects:
Prilocaine can cause methaemoglobinaemia.
Bupivacaine is cardiotoxic. Levobupivacaine is less cardiotoxic.
Related toxins
Tetrodotoxin (TTX) and saxitoxin (STX) are two toxins produced by fish. They are very potent and highly selective Na+ channel blockers and aren’t used clinically. They act from the extracellular side of the fibre, unlike the drugs. Tetrodotoxin does not affect Na+ channels in the heart or in nociceptive fibres.
Paralysis of the respiratory muscles is what kills you.
Under “All local anesthetics…” You wrote that they are bases. But the pH in the human body is slightly basic 7.35-45. Shouldn’t the molecules be in lipophilic form then?
They’re in an equilibrium, so a proportion of them are probably in lipophilic form, yes.
Probably written wrong in our lecture then, because I see now that the sequence what you wrote is the same as in mine, so the first part must be a mistake.
Thank you for checking! I just had to be sure, sorry to doubt you!
No need to apologize! I’ve received more than 300 comments on the website and almost every one of them find something which is wrong in my notes. Only very rarely are the commenters wrong.
Hi!
I was reading through the lecture from this topic, and there it says “Faster, more effective block on the thick fibres” etc… I think you have written the opposite? Could you check that? 🙂
I don’t know if your lecture is wrong or if you misread what it says, but what I’ve written is correct. The book agrees. The lecture I have from last year writes:
● thin (C és Aδ) fibers are more susceptible to block than thick
ones (Aβ, Aγ és Aα), the myelin sheath reduces sensitivity;
however, the thin myelinated praeganglionic (B-type) and
unmyelinated postganglionic sympathetic (C-type) fibers are
highly sensitive
● sequence of loss of sensory modalities: pain → cold → warmth
→ touch → pressure → motor function
● in thick nerve bundles superfical motor fibers are blocked first
It wouldn’t make sense for them to block thick fibres better than thin fibres anyway.
Hi!
Would you mind explaining this? You have written: “The systemic side effects also occur when the anaesthetics are taken up into the plasma. Therefore, the shorter the plasma half-life, the fewer systemic side effects. Amide type local anaesthetics bind more easily to plasma proteins than ester types, and therefore have fewer systemic side effects.”
On the lecture it says that Esthers have a shorter half-life compared to Amides, would not Eshters have fewer side effects?
Appriciate your notes!!
Good question. I suppose the plasma protein binding and ester group itself contribute to the side effects of the esther drugs.