Table of Contents
Page created on March 7, 2018. Last updated on November 19, 2018 at 17:16
Summary
- In the well-fed state, the pancreas produces insulin, which puts the body into an anabolic state, which signals the body to start using glucose and ATP for maintenance processes
- In the fasting state, the pancreas produces glucagon, which puts the body into a catabolic state, which activates processes that increase blood glucose that the brain and muscles can use.
- Adipose tissue produces a hormone called leptin, which inhibits hunger and activates AMPK
- Ghrelinergic cells in the GI tract produce ghrelin, a hormone which increases hunger
- Adipose tissue also produces another hormone, adiponectin, which activates AMPK
Leptin
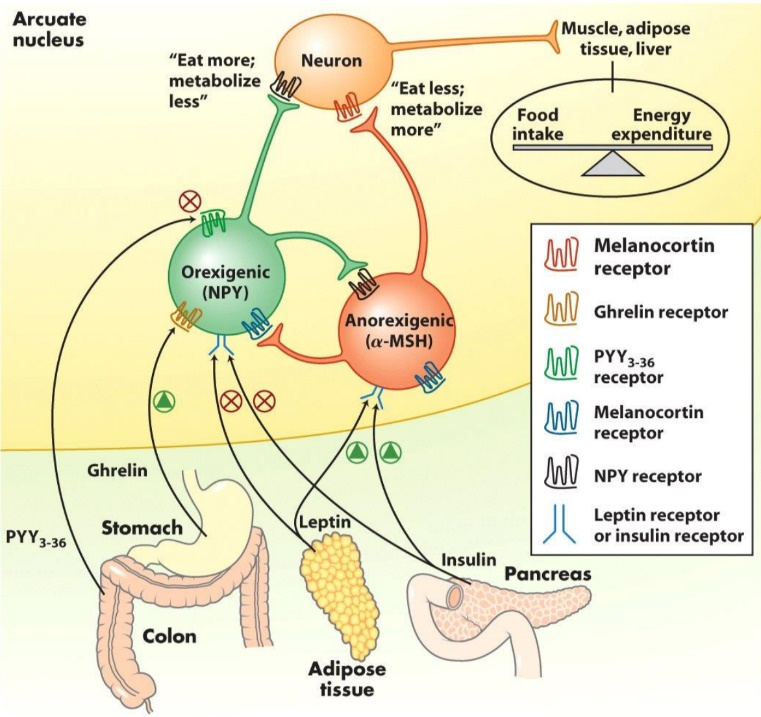
Leptin is a peptide hormone produced and secreted by adipose tissue. Leptin travels with the blood into the brain where it interacts with the arcuate nucleus in the hypothalamus. Specifically, it activates anorexigenic (α-MSH) neurons (orexi means appetite in Greek and an means “anti”, meaning anti-appetite-stimulating neuron). It also inactivates the orexigenic (NPY, neuropeptide Y) neurons. Leptin stimulates these neurons through the JAK-STAT pathway. The anorexigenic neuron will decrease hunger, while increasing the energy expenditure of the body.
After the arcuate nucleus has received the leptin signal, it will send a nerve signal with a sympathetic nerve cell to adipose tissue. The nerve signal releases norepinephrine to bind to a β3-adrenergic receptor on the cell surface of the adipocyte. The receptor will activate adenylyl cyclase which increases [cAMP], which activates PKA. It therefore activates the same pathway as glucagon and epinephrine. It also activates AMPK.
PKA, in addition to doing regular PKA things, has two unique effects in the adipocyte. Firstly, it activates a protein called perilipin, which coats lipid droplets in adipocytes. Perilipin usually protects the lipid droplets from being digested, but when phosphorylated by PKA, it stops protecting them, allowing them to be broken down by hormone-sensitive lipase, a lipase also activated by PKA.
Secondly, PKA increases expression of the gene for uncoupling protein, or UCP. UCP does what its name suggest, and “uncouples” the mitochondria. This means that it allows protons to cross the inner mitochondrial membrane without passing through ATP synthase, the protein that usually takes advantage of these protons passing through it to phosphorylate ADP to ATP. The consequence of uncoupling is that the energy produced in the mitochondria goes out as heat instead of being converted into ATP. This increases the amount of energy the body uses, which means it also increases burning of fat.
Ghrelin
Ghrelin is a peptide hormone produced by ghrelinergic cells in the gastrointestinal tract. It works oppositely to leptin, by influencing the brain to increase the feeling of hunger, and to metabolize less. It follows the same pathway into the arcuate nucleus as leptin but stimulates orexigenic neurons instead of inhibiting them, therefore having the opposite effect as leptin.
PPARs
Peroxisome proliferator-activated receptors, or PPARs are a group of nuclear receptors in the cell that function as transcription factors when they bind their ligand. The PPARs linger in the cytosol, until they bind a ligand, such as a fatty acid, or a drug. After binding, it binds with another protein in the cytosol, called Retinoid X receptor, or RXR. The complex of ligand-PPAR-RXR then travels into the nucleus, where it binds to a response element, a DNA sequence that either increases or decreases transcription of certain genes.
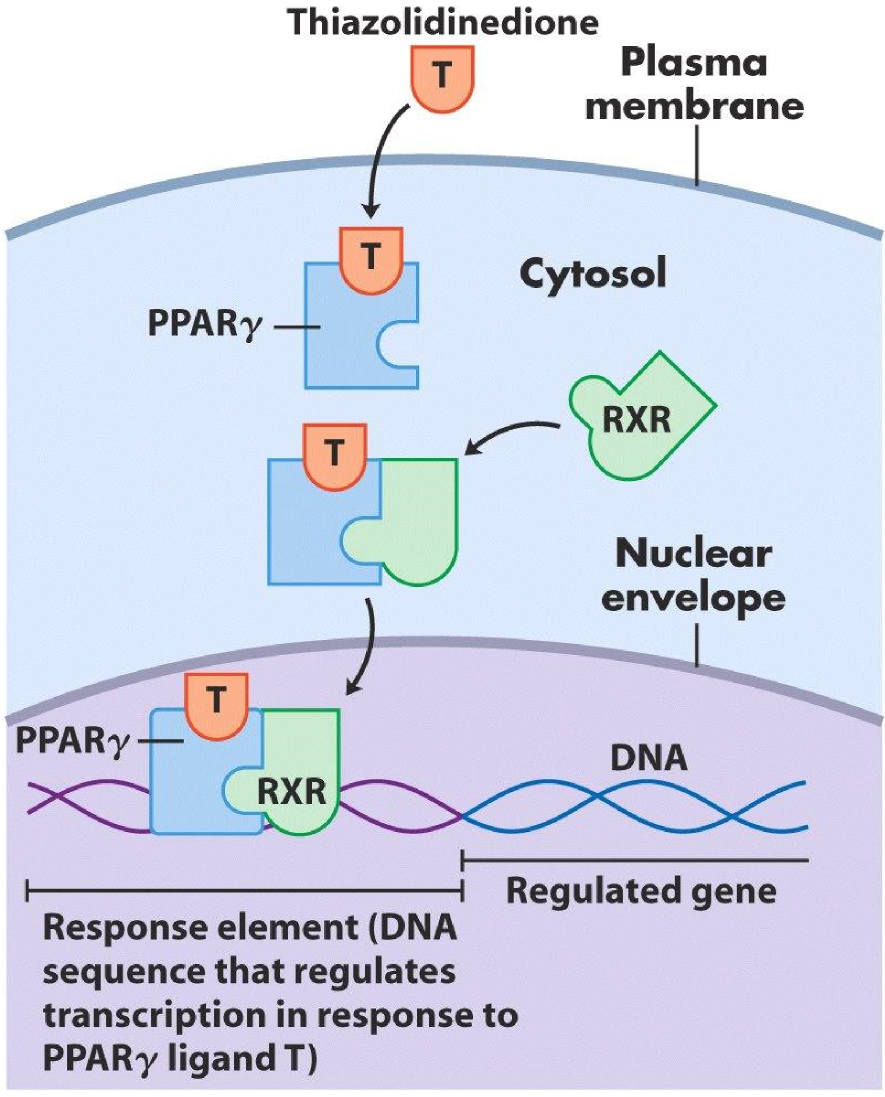
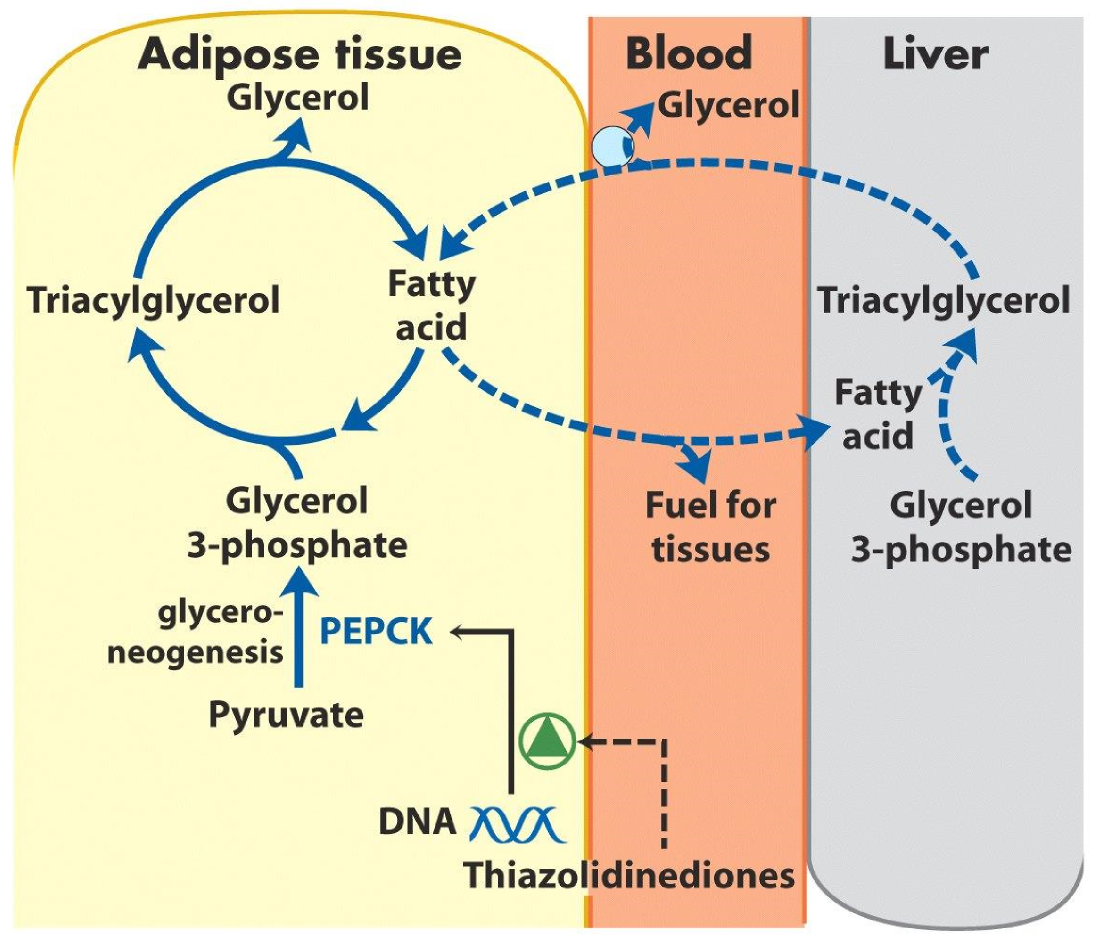
A drug that acts as a ligand for PPARγ is thiazolidinedione. This drug is used to treat type 2 diabetes by increasing transcription of PEPCK in adipose tissue, so that the adipose tissue can produce more glycerol to produce more fat. In order for adipose tissue to produce fat it needs blood glucose. All in all will thiazolidinedione lower blood glucose.
Adiponectin
Adiponectin is a peptide hormone produced by adipose tissue. It’s special in a way that it’s very abundant in the blood compared to other peptide hormones. It activates AMPK, and therefore has the same effects on the metabolism as AMPK; increased β-oxidation, reduced gluconeogenesis and so on.
AMPK activates β-oxidation by inhibiting Acetyl-CoA Carboxylase. ACC produces malonyl-CoA which inhibits the transportation of fatty acids into the mitochondria by the carnitine shuttle, which is necessary for β-oxidation. By inhibiting the enzyme that inhibits β-oxidation, it is activated.
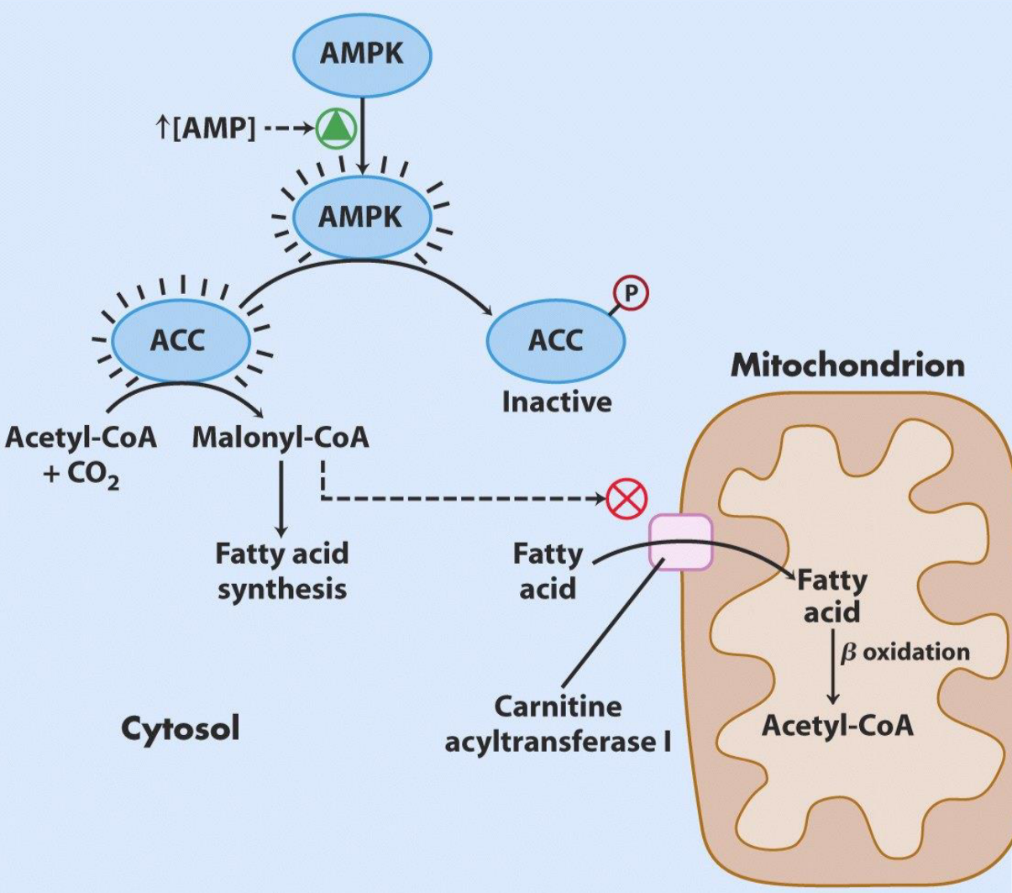
The activation of β-oxidation by AMPK, and therefore by adiponectin. Notice that the activation of β-oxidation is by inhibiting the inhibitor of it.