Table of Contents
Page created on October 20, 2019. Last updated on December 18, 2024 at 16:55
The heart has a special system that allows it to be excited rhythmically and repetitively. There are two components to this system:
- Pacemaker generators that generate rhythmical electrical impulses which initiate rhythmical contraction of the heart muscle
- A conduction system which conducts these impulses rapidly through the heart
When this system functions normally the atria contract one sixth of a second before the ventricles, which allows the ventricles to fill up with blood before pumping the blood through the pulmonary or systemic circulation.
Generators of impulses in the heart
The heart has two impulse generators; the main generator and one “backup” generator in case the main generator doesn’t work. The main generator is the sinus node, and the backup generator is the atrioventricular node. The His-Purkinje system can also act as a backup generator. We call them pacemakers, and they’re comprised of specialized cardiac muscle cells called pacemaker cells.
Sinus node:
The main impulse generator is called the sinus node or the sinoatrial node, often called the SA node. It’s a small piece of specialized cardiac muscle located in the wall of the right atrium right below and lateral to the opening of the superior vena cava.
The SA node has an intrinsic rate of 60 – 100 beats/min, meaning that it generates impulses this many times per minutes on its own. This node contains contractile filaments, but these filaments are weak compared to the contractile filaments of the normal cardiac muscle. The cells of the SA node are interconnected via gap junctions, which enable them to depolarize adjacent cells.
The pacemaker cells slowly depolarize by themselves (phase 4), a property non-pacemaker cells don’t have, which is what accounts for the automaticity of the pacemaker. In addition to this the pacemaker cells have more positive resting potential than normal cardiomyocytes, -60 mV instead of -85 mV. The threshold for depolarization is -40 mV.
The depolarization of pacemaker cells consists of three phases; phases 0, 3 and 4.
Phase 4 is the phase of spontaneous diastolic depolarization (SDD). It occurs due to a continuous inward Na+ current called the funny current and due to the opening of T-type Ca2+ channels. The cell slowly depolarizes by itself during diastole, eventually reaching the threshold at -40 mV, which starts phase 0.
Phase 0 is the upstroke of the action potential. It’s caused by opening of voltage-gated L-type Ca2+ channel, causing Ca2+ influx. This is different from normal cardiac muscle cells, where the upstroke is caused by opening of fast Na+ channels. The calcium channel is slower than the sodium channel, so the upstroke is slower in pacemaker cells than in normal cardiomyocytes.
Phase 3 is the phase of repolarization. It’s caused by opening of leaky K+ channels, which causes an outward K+ current that causes repolarization.
Action potential generated by the SA node propagates through the atria, causing them to contract simultaneously. The action potential eventually reaches the atrioventricular node.
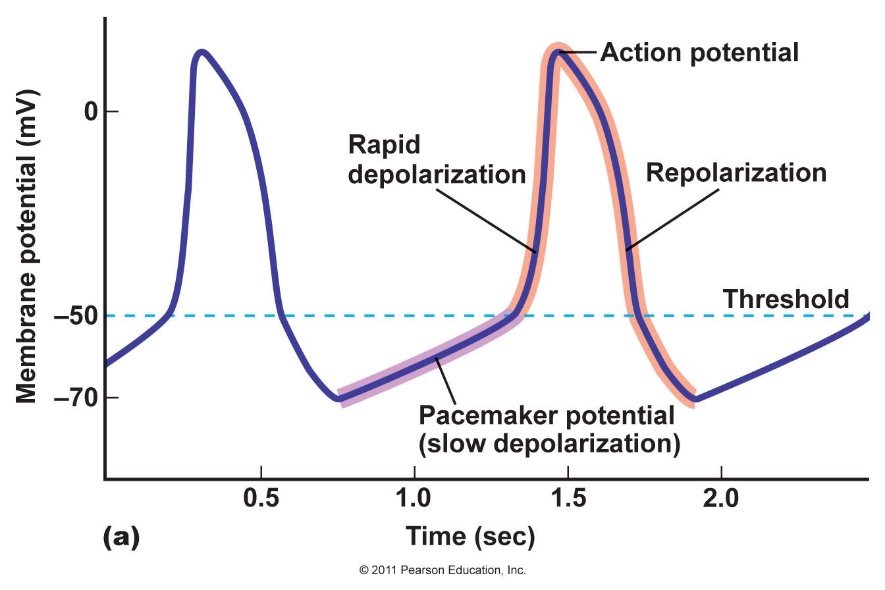
Action potential of the SA node.
Atrioventricular node:
The atrioventricular node is often called the AV node. Like the name implies it lies between the atria and ventricles, more specifically right behind the tricuspid valve.
The main function of the AV node is to delay the conduction of the action potential from the atria to the ventricles. We don’t want the atria and ventricles to contract simultaneously; we want the atria to contract a little time before the ventricles. The AV node is responsible for this delay.
The atrial muscle and ventricular muscle are separated by continuous fibrous tissue at all points except at the AV node. Fibrous tissue doesn’t conduct impulses, so this forces the action potential from the atria to pass through the AV node on the way to the ventricles.
The cells of the AV node contain fewer gap junctions than the other pacemaker cells. This increases the resistance to conduction of the action potential, which is what causes the delay.
If the SA node stops generating impulses for any reason, the AV node will take over. The AV node has an intrinsic rate which is lower than the SA node at around 40 – 60 beats per minute.
The AV node has another property: it can prevent impulses from travelling the opposite way, i.e. from the ventricles to the atria. This one-way conduction is essential for normal, forward heart conduction.
Conductors of impulses in the heart
The impulses of the heart normally originate in the SA node, travel through the atria and to the AV node, where it is delayed before it reaches the ventricles.
After the AV node the impulse reaches the bundle of His, also called the AV bundle. The bundle of His branches into the left and right bundle branches. The bundle branches conduct the impulse through the septum until they reach the apex, where they branch into the Purkinje fibres, which distribute the impulse to the ventricular muscle.
The depolarization of the ventricular muscle occurs in the following sequence: Septum – apex – endocardium – epicardium. The repolarization occurs in the opposite order.
The conduction velocity varies in the different parts of the conduction system:
- In the SA node – 0,05 m/s
- Between the SA node and AV node – 1 m/s
- In the AV node – 0,05 m/s
- In the bundle of His – 1,5 m/s
- In the Purkinje fibres – 4 m/s
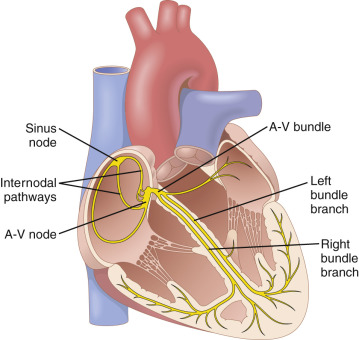
The cardiac conducting system (in yellow). From Guyton.

From Wikipedia
Action potentials in ventricular muscle
Action potentials propagate differently in non-pacemaker cells than in pacemaker cells. These action potentials are fast but last long, up to 300 msec. Here there are five phases instead of three.
Phase 4 is the resting phase. Ventricular muscle has a stable resting potential of -85 mV. There is no spontaneous depolarization like in pacemaker cells. During phase 4 the heart is in diastole.
Phase 0 is the upstroke of the action potential. When an action potential arrives from a neighbouring cell through gap junctions, the potential of the cell will slightly increase. If this increased potential reaches the threshold potential of -70 mV fast sodium channels will open, causing a fast Na+ influx which causes the upstroke of the action potential.
Phase 1 is a brief period of repolarization. The cell is slightly repolarized due to efflux of K+ and Na+.
Phase 2 is the plateau of the action potential. During this phase L-type Ca2+ channels open, causing an influx of calcium. K+ channels also open, causing an efflux of potassium. The inward and outward currents are approximately equal, so the membrane potential is stable, forming a plateau.
Phase 3 is the repolarization. It’s caused by the opening of more K+ channels and closure of the L-type Ca2+ channels, causing a large efflux of potassium. This returns the membrane potential to the resting membrane potential of -85 mV.
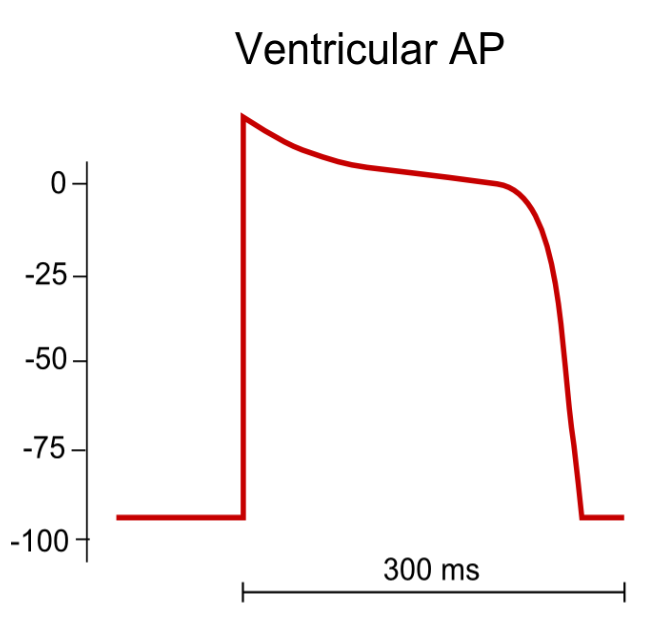
Action potential in ventricular muscle.
All-or-none law:
Phase 0 will only occur if the increased membrane potential reaches the threshold potential. If the membrane potential doesn’t reach the threshold there will be no response, but if it does reach the threshold there will be a full response. There can only be no response or full response. This is called the all-or-none law.
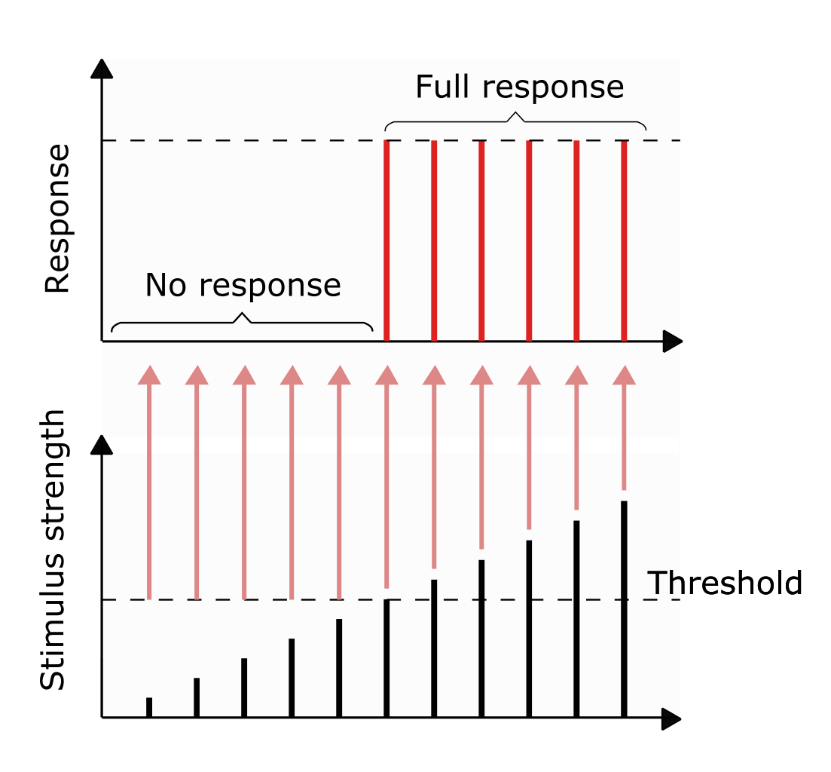
There will either be a response or there won’t be. A larger initial stimulus (black) doesn’t cause a larger response.
Refractory periods
For some time after the cardiac cell was excited it cannot be re-excited. This is called the refractory period. There are two types:
- Absolute refractory period – where no action potential can be initiated at all
- Relative refractory period – where an action potential can be initiated only by a very large current
For the ventricular muscle cells the absolute refractory period is 0,25 – 0,30 seconds, which corresponds to the plateau of the action potential. The relative refractory period is 0,05 seconds.
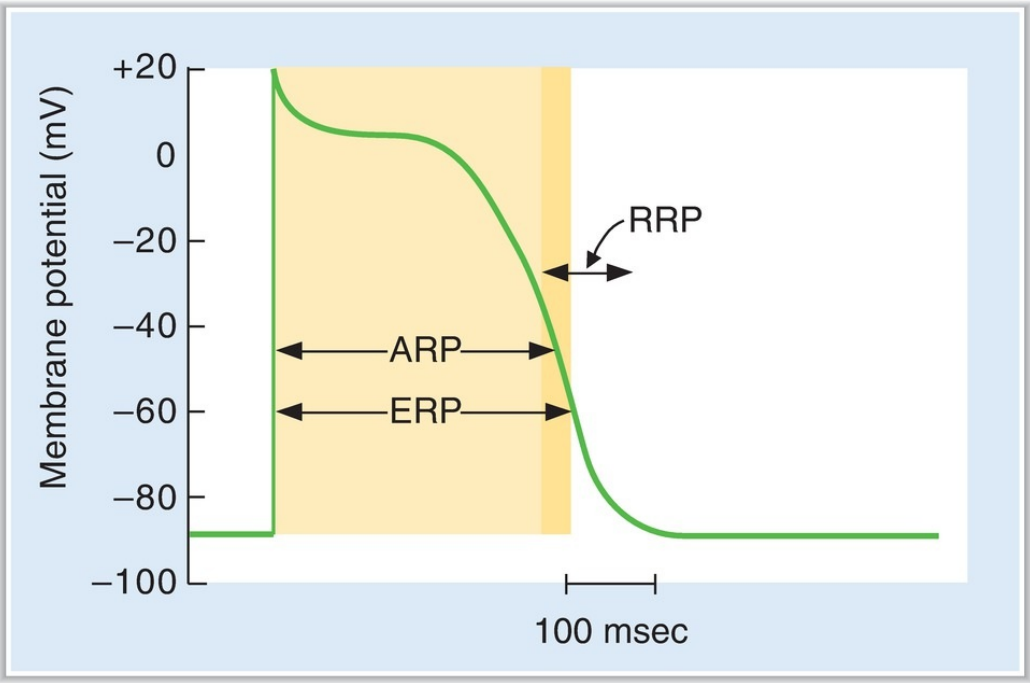
The refractory periods of ventricular muscle. RRP = relative refractory period, ARP = absolute refractory period. Ignore the ERP.
Excitation-contraction coupling
Excitation-contraction coupling refers to the physiological process of converting an electrical stimulus to a mechanical response. More specifically it refers to how an action potential can cause a muscle to contract.
When the action potential arrives to a ventricular muscle cell L-type calcium channels will open during the plateau. This causes an influx of calcium. This increase in intracellular calcium triggers the release of more calcium from the sarcoplasmic reticulum. This calcium will bind to a protein called troponin, which is bound to the actin filament. This causes troponin to change conformation, which causes myosin to bind to actin. Myosin will then use ATP to move actin along, which causes the muscle fibre to shorten.
Innervation of the heart
Different parts of the heart are innervated by both the sympathetic nervous system and the parasympathetic nervous system. The sympathetic nerves innervate all parts of the heart while parasympathetic nerves innervate only the SA and AV nodes. Together these two nervous systems regulate the heart rate, the conduction velocity, the excitability and the force of contraction of the heart. These modalities have specific names:
- Rate of rhythm of the SA node – the chronotropic effect
- The conduction velocity (through the AV node) – the dromotropic effect
- The excitability – the bathmotropic effect
- The force of contraction – the inotropic effect
Parasympathetic stimulation:
Parasympathetic stimulation of the heart causes the following:
- Negative chronotropic effect – reduced heart rate
- Negative dromotropic effect – reduced conduction velocity
- Negative bathmotropic effect – reduced excitability
Parasympathetic stimulation occurs during rest, etc.
Sympathetic stimulation:
Sympathetic stimulation of the heart causes the following:
- Positive chronotropic effect – increased heart rate
- Positive dromotropic effect – increased conduction velocity
- Positive bathmotropic effect – increased excitability
- Positive inotropic effect – increased myocardial contractility
Sympathetic stimulation occurs during exercise, etc.