Table of Contents
Page created on April 14, 2022. Not updated since.
Non-Hodgkin lymphomas
Introduction and epidemiology
Non-Hodgkin lymphomas (NHLs) are a heterogenous group of lymphomas. We distinguish indolent/low-grade NHLs, aggressive/high-grade NHLs, and intermediary NHLs.
The indolent/low-grade non-Hodgkin lymphomas are much less harmful than the aggressive/high-grade ones. In many cases, patients die with indolent lymphomas rather than of them. They remain asymptomatic for many years and are therefore often diagnosed incidentally on a laboratory test rather than due to the patient presenting with symptoms.
In some cases, they may not even require treatment, as they progress so slowly. Even untreated, the life expectancy is multiple years. The tumor cells don’t proliferate fast. In most cases, indolent lymphomas are uncurable due to their slow growth. Indolent NHLs are more frequent in older patients.
Aggressive lymphomas are very aggressive malignancies, as they proliferate rapidly and untreated the life expectancy is just a few weeks. They can be considered “high-grade”. However, thanks to their rapid growth, they are potentially curable. They are more frequent in children.
Classification
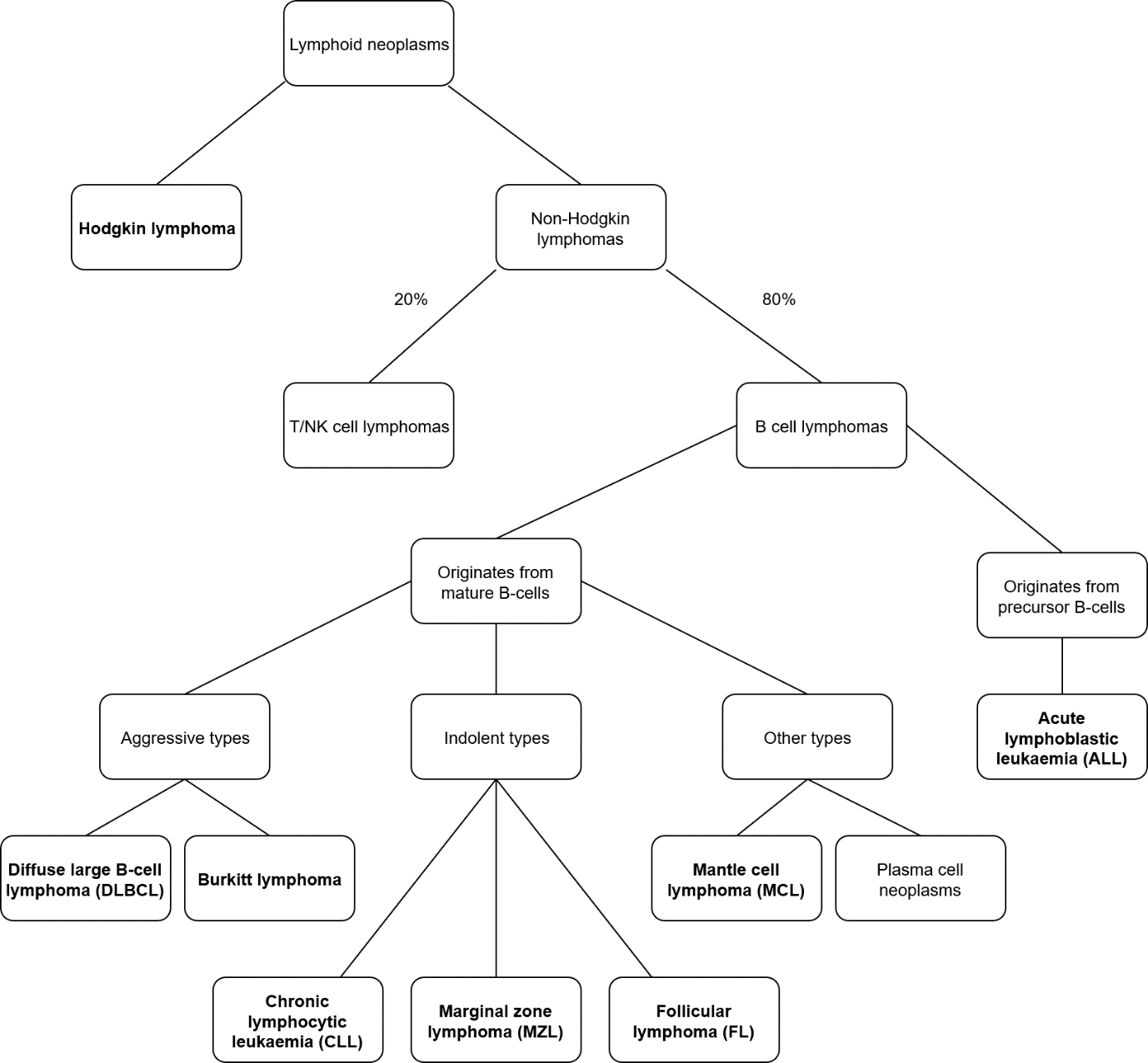
85% of non-Hodgkin lymphomas originate from B-cells. The different types of NHLs are shown in the figure:
The most common NHL is DLBCL, followed by follicular lymphoma.
Staging
The staging system for lymphomas is called the Lugano staging system, which is a modified version of the Ann Arbor staging. It is similar to the TNM staging system. It works like this:
- Stage I – cancer in a single region, usually one lymph node and the surrounding area
- Stage II – cancer in more lymph node regions, on one side of the diaphragm
- Stage III – cancer in more lymph node regions, on both sides of the diaphragm
- Stage IV – cancer in one or more extralymphatic organs, like the bone marrow, liver or lung
Also, several modifiers are used:
- E – if there is extranodal involvement
- A – if there are no “B symptoms”
- B – if there are B symptoms
- X – larger than 10 cm mass – called “bulky disease”
Stages I and II are referred to as “early stage” while stages III and IV are referred to as “advanced stage”.
Clinical features
The clinical features differ between high grade and low grade NHLs, although there might be some overlap:
- Low grade
- Lymphadenopathy which may fluctuate or spontaneously remit, and
- Hepatosplenomegaly
- Cytopaenias
- High grade
- Rapidly growing lymph nodes or masses
- B symptoms
Some NHLs present in extranodal tissues, for example as GI polyps (mantle cell lymphoma).
Diagnosis and evaluation
Excisional biopsy of the affected lymph node with immunohistochemistry and flow cytometry gives the diagnosis. Cytogenetic and molecular analysis can show chromosomal changes and mutations which are specific for each subtype.
Bone marrow biopsy and aspirate are necessary to detect bone marrow involvement. Lumbar puncture to look for CNS involvement is indicated in case of T-cell NHL, AIDS, or high grade lymphoma with positive blood marrow.
Treatment
Treatment options for NHLs include:
- Indolent NHLs
- Watch and wait (observation and follow-up)
- Monotherapy with alkylating agent
- R-CHOP
- Allogenic stem cell transplantation
- Aggressive NHLs
- Early stage -> R-CHOP ± radiotherapy
- Advanced stage -> R-CHOP, sometimes intrathecal chemotherapy and radiotherapy
The R-CHOP regimen involves rituximab, cyclophosphamide, doxorubicin (hydroxydaunorubicin), vincristine (Oncovin®), and prednisone. Rituximab is an anti-CD20 antibody and is only given if the disease is CD20+.
Indolent non-Hodgkin lymphomas
Follicular lymphoma
Follicular lymphoma (FL) is the most common indolent NHL, and the second most common NHL overall. It’s caused by a t(14;18) translocation which causes upregulation of the antiapoptotic protein Bcl2. Approximately 15% of cases undergo histologic transformation (HT) to DLBCL.
Mantle cell lymphoma
Mantle cell lymphoma (MCL) is caused by a t(11;14) translocation which causes upregulation of cyclin D1. It can occasionally present as GI polyposis. It has a poor prognosis despite being indolent.
Marginal zone lymphoma
Marginal zone lymphoma (MZL) can be extranodal, nodal, or splenic, where the former is most common. Extranodal MZL originates from MALT and is associated with chronic inflammation or infection, for example in case of:
- H. pylori infection – gastric MALT lymphoma
- Chlamydia psittaci infection in the eye – ocular adnexal lymphoma
- Sjögren syndrome – MALT lymphoma in the salivary glands
Treating the underlying infection or inflammation often causes the malignancy to enter complete remission.
Aggressive non-Hodgkin lymphomas
Diffuse large B-cell lymphoma
Diffuse large B-cell lymphoma (DLBCL) is the most common NHL overall. It may develop de novo or secondary to transformation from an indolent B-cell NHL, often CLL/SLL (in which case it’s called Richter transformation) or follicular lymphoma. The de novo type has better prognosis than the secondary.
Burkitt lymphoma
Burkitt lymphoma (BL) is infamous for being one of the most rapidly growing tumours, with a doubling time less than 24 hours. It’s characterised by deregulation of c-Myc. Three forms of Burkitt lymphoma can be distinguished:
- Sporadic Burkitt lymphoma
- Endemic Burkitt lymphoma
- HIV-associated Burkitt lymphoma
Endemic BL is endemic to equatorial Africa and South America and is highly associated with EBV infection. Non-endemic BL presents as a mass in the abdomen, while endemic BL presents as a mass in the jaw.
Because it’s so rapidly proliferating, BL must be managed as acute leukaemia. There is significant risk of tumour lysis syndrome.